Journal of Nutrition & Food Sciences
Open Access
ISSN: 2155-9600
ISSN: 2155-9600
Research Article - (2019)Volume 9, Issue 3
Malnutrition is the most common pathological condition of deficiency/excess of necessary nutrients. It is a significant cause of morbidity and mortality in children worldwide. It causes 60% deaths of children in the developing countries. The current study investigated types, risk factors and co-morbidities of Protein Energy Malnutrition in children at Gadarif eastern Sudan. It was a descriptive cross-sectional study conducted during 2017. Seventy-eight children (<15 years old) with confirmed PEM were selected for this study through Gadarif Hospital. 62.8% of the children were males and 37.2% were females. 92.3% of the affected children belonged to 0-3 years old age group. There was significant statistical difference between the age groups and PEM (χ2 = 34.876, df =12, p=0. 000). Underweight (30.8%) was the most common form of PEM. Low socioeconomic status (96.2%) which includes poverty was observed. Illiteracy of mothers was 94.9% and for fathers it was 89.7% (statistically significant p=0. 034). Family size associated with the disease was significant (χ2 = 71.821, p=0. 02). Malaria (57.7%) and anemia (26.9%) were the most common associated co-morbidities. 65.4% of the children were recovered and discharged with good condition while 5.1% of the children died due to hypothermia, severe dehydration and hypovolemic shock. PEM in Gadarif, Sudan was due to low socioeconomic status, illiteracy and large family size. For effective management of malnutrition; multiple and synergistic interventions must be implemented in agriculture and micronutrients as well as nutrition-based education, provision of balanced-quality health services and fighting of illiteracy and poverty.
Protein energy malnutrition; Types; Risk factors; Children; Sudan
Sudan consists of 18 states and 184 localities with an estimated population of 31 million people. On the other hand, Gadarif State is located in eastern part of Sudan. It borders by Ethiopia at the South-East and four Sudanese states; Kassala at the East, Gezira at the West, Sinnar at the South and Khartoum at the North- West [1]. Gedarif State consists of 12 localities. The state has a population of approximately of 1.917 million [2]. Most of Gadarif State’s populations (71.7%) live in the rural areas and 28.3% live in the urban areas of the State. Almost 70% of the State populations work in agriculture, forestry and hunting [2].
Malnutrition refers to under-nutrition or insufficient intake of nutrients and or energy. Malnutrition may be a significant factor in diseases of human. In this context, symptoms of malnutrition are related to poverty. Malnutrition is also related to dietary practices inconsistent with health [3]. On the other hand, in humans, nutrition and birth weight are strongly associated. Studies on maternal nutrition suggest that adequate nutrition is an important determinant of birth weight. Improving the nutritional status of malnourished mothers increases the birth weight and therefore, survival of their infants. Inadequate maternal nutrition decreases infant birth weight, which is associated with increased morbidity and mortality [3]. Food supplies body with energy and specific nutrients. The latter are essential dietary factors such as vitamins, minerals, essential amino acids and essential fatty acids, which cannot be synthesized by the human body and fulfill essential physiological and metabolic functions. Adequate supply of metabolic fuels (carbohydrates, lipids and proteins) and nutrients is related to good health [3]. Malnutrition is the most common pathological condition resulting from deficiency or excess of necessary nutrients [4]. Malnutrition is a significant cause of morbidity and mortality in children worldwide [5]. For instance, malnutrition is the cause of approximately 60% deaths of children in the developing countries [6]. Malnutrition impairs body function, normal growth, cognitive development, reproduction, physical work capacity and it negatively predisposes to disease. Generally, malnutrition impairs performance, health and survival of human [5]. Inadequate dietary intake of protein resulted in the form of malnutrition called protein energy malnutrition (PEM) [5]. The PEM is a major health problem in developing countries and a major risk factor of morbidity and mortality of children [5]. In sub- Saharan Africa [7,8] the mortality due to the PEM is in the range of 25-35%. There are several risk factors associated with protein energy malnutrition deficiency such as poverty, low education and socioeconomic status [9].
Sudan has the highest rate of acute malnutrition in Africa [10]. A national survey conducted in 2013 revealed that 128 of the total 184 Sudan’s localities have a stunting (chronic malnutrition) rate classified as “high” that were above 30% [11]. According to the UN Children's Agency [12], some two million children under age five in Sudan suffer from chronic malnutrition. Moreover, another one million children under age five in Sudan suffer from acute malnutrition resulting in an average global acute malnutrition (GAM) rate of 16.3%, which is above the 15% threshold that constitutes a critical emergency [10]. Among these, Gadarif has the highest stunting rates, estimated as 73% [10,12].
PEM is a serious problem in Africa in general and in Sudan in particular. There is still a huge lack of knowledge on this problem. The problem of PEM is not well mapped in Africa in general and in Sudan in particular. There is a need for huge collective efforts to adequately address PEM in Africa in general and in Sudan in particular. Research to address factors responsible for inadequate nutrition in children is important for human and national economic development. Up to date, Gadarif State has had only general data on the nutritional status of its populations including children and women. A comprehensive investment plan for addressing child malnutrition in Gadarif State is urgently needed. The aim of the present study was to determine types, risk factors, and co-morbidities in children with PEM in Gadarif State, eastern Sudan.
This a descriptive cross-sectional hospital-based study that was conducted from 1st January to 31st June 2017 to investigate the epidemiology of PEM including risk factors, types and co-morbidities among children in Gadarif Hospital, eastern Sudan. The study included a total of 78 children (ages ≤ 15 years old) who were presented to the outpatient clinics of Gadarif Pediatrics Teaching Hospital and admitted to malnutrition ward with confirmed diagnosis of PEM.
The study was approved by the research and ethical committee of the Faculty of Medicine & Health Sciences at the University of Gadarif, Sudan.
Data statistical analysis
Data was analyzed using Statistical Package for Social Sciences (SPSS) software version 20.0. Descriptive analyses for demographic data and clinical findings and outcomes were performed with statistically significant value <0.05.
This study comprised 78 PEM affected children, out of which 49 (62.8%) were males and 29(37.2%) were females, with the M: F ratio of 1.7:1. 54(69.2%) of affected children were from rural areas. 36 (46.2%) of children were from Hawsa tribe followed by Noba 10(12.9), Miseria 8(10.3), Dabiana 5(6.4%), bani-aamer 5(6.4%), Kenana 2 (2.6%) and Jaaleen 1(1.3) tribes and 11 were of unknown races. The most common form of PEM noted in this study was underweight 24 (30.8%) as shown in Table 1. More forms of PEM were noted in males than in females except underweight, but this finding was not statistically significant (χ2 = 6.3, df =3, p=0.098).
| Type | Female | Male | Frequency |
|---|---|---|---|
| Marasmus | 4 | 14 | 18 |
| Kwashiorkor | 5 | 12 | 17 |
| Marasmic-Kwashiorkor | 5 | 11 | 16 |
| Underweight | 12 | 12 | 27 |
| Unclassified | 3 | 0 | 3 |
| Total | 29 | 49 | 78 |
Table 1: Sex-wise distribution of SEM types in the study population.
PEM was most commonly found among the age group 0-3 years, with a frequency of 72 out of total of 78 subjects (92.4 %; Table 2).
| Type | 0-3 | 4-7 | 8-11 | 12-15 |
|---|---|---|---|---|
| Marasmus | 16 | 0 | 0 | 2 |
| Kwashiorkor | 16 | 1 | 0 | 0 |
| Marasmic kwashiorkor | 16 | 0 | 0 | 0 |
| Underweight | 22 | 2 | 0 | 0 |
| Unclassified | 2 | 0 | 1 | 0 |
| Total | 72 | 3 | 1 | 2 |
Table 2: Distribution of different SEM types according to age group of the study subjects.
There was statistically significant difference between the age groups and different forms of PEM (χ2 = 34.876, df =12, p=0. 000) (Figure 1).
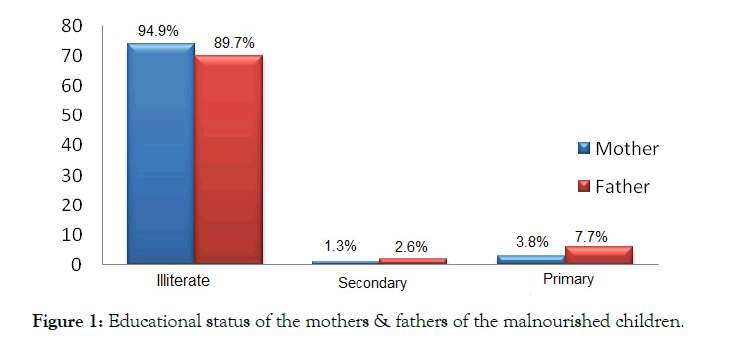
Figure 1: Educational status of the mothers & fathers of the malnourished children.
Education status of the parents was investigated, in which the illiteracy level was found to be higher in mothers 74 (94.9%) than in fathers 70 (89.7%) (χ2 = 10.400, df =4, p=0. 034), considering primary and higher secondary school education of parents (Figure 1).
Low and moderate socio-economic status was observed in this study accounting for 75 (96.2%) and 3(3.8%), respectively. The employment status of the fathers of the affected children was analyzed in which laborers were found to be the highest 52(66.7%), followed by farmers 24 (30.8%) and lastly idles 2 (2.5%) (Figure 2).
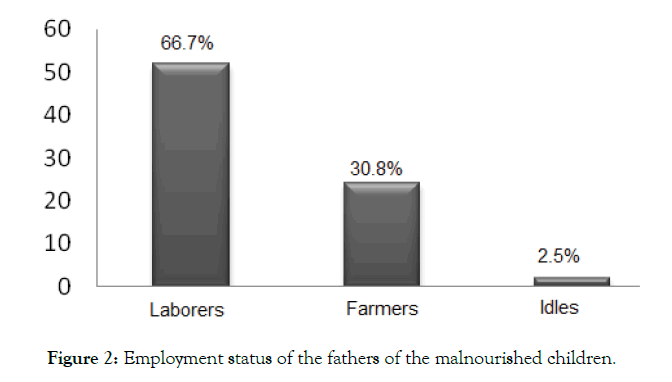
Figure 2: Employment status of the fathers of the malnourished children.
In the present study the family size was found to be significant (χ2 = 71.821, p=0. 02); 51(65.4%) of children belonged to family size of sixth or more, while 27(34.6) children belonged to family size of fifth or less.
Non-exclusive breast feeding in first six months was found in 53(67.9%) subjects while exclusive breast feeding was found in 25 (32.1%) subjects as shown in Table 3. Regarding weaning practice 57(73.1%) were suddenly weaned while 17(21.8%) were weaned gradually (Table 3).
| Frequency | Percentage | |
|---|---|---|
| Breast feeding | ||
| exclusive breast feeding1-6 months | 25 | 32.1 |
| Not exclusive breastfeeding | 53 | 67.9 |
| Weaning practice | ||
| Gradually | 17 | 21.8 |
| Suddenly | 57 | 73.1 |
| unknown | 4 | 5.1 |
| Total | 78 | 100.0 |
Table 3: Breast feeding status of the study subjects.
Diarrheal diseases and anemia were the most common associated conditions in 37 (47.4%) and 21(26.9%) of the children respectively as shown in Table 4.
| Frequency | Percentage | |
|---|---|---|
| Anemia | 21 | 26.9 |
| Malaria | 4 | 5.1 |
| Chest infection (pneumonias, acute bronchitis and other) | 16 | 20.5 |
| Diarrheal diseases | 37 | 47.4 |
| Total | 78 | 100 |
Table 4: The PEM co-morbidities among the study subjects.
51 (65.4%) of children were recovered and discharged with good condition while 4(5.1%) children died as shown in Figure 3.
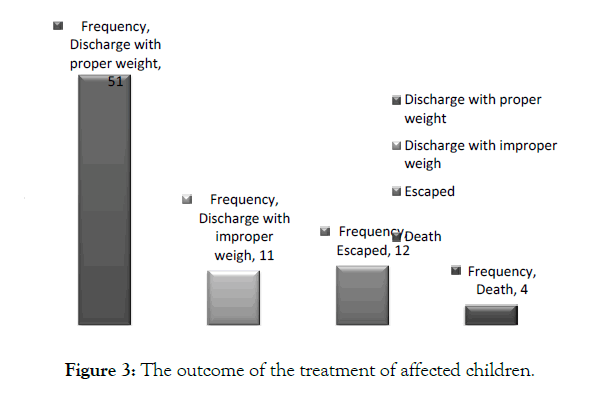
Figure 3: The outcome of the treatment of affected children.
The balanced diet must contain six important components in appropriate quantity and quality; these components are carbohydrates, lipids, proteins, vitamins, minerals and water. Carbohydrates and lipids are mainly needed for energy production, while proteins are essential for normal growth and development, repair of tissues and their maintenance. Vitamins are needed to function as coenzymes and are essential for many physiological and biochemical processes and reactions in the human body. Minerals in the human body fulfill many vital functions that include electrolyte balance, ionic equilibrium, activation of chemical processes and acidbase equilibrium. Water serves as a solvent for all intracellular and extracellular chemical reactions and processes taking place in the human body, it acts as a cooler evaporator, transporter, it is the main source of hydrogen ions in the body, it is essential for the stability of all cellular and sub-cellular structures and it is required to replace the daily fluid losses through skin, lungs, feces and urine [3].
Proteins are the bases of protoplasm. The main source of proteins for man is the dietary proteins. Dietary proteins are essential for the biosynthesis of hemoglobin, plasma proteins and tissue proteins. The quality of proteins in the diet is determined by their easy digestibility, the content of their amino acids and the efficiency of amino acids’ absorption [3]. In this respect, animal proteins are superior in biological value to vegetable proteins. Whole egg proteins and milk proteins rank highest with meat, kidney and other proteins ranking next [3]. Deficiency of the dietary proteins in one or more of the essential amino acids leads to the disturbance of the nitrogen equilibrium and nitrogen balance [3]. The lack of adequate amount of proteins in the diet results in insufficient availability of amino acids to the cell to synthesize new proteins. In case of deficiency of the dietary proteins, tissue proteins are degraded to supply the missing amino acids and that results in an increased loss of non-protein nitrogenous compounds in urine. The first effect of protein deficiency in children is the slowing of growth and loss of weight. Dietary proteins are essential for the biosynthesis of intestinal mucosal proteins and the effective functioning of the digestive glands [3]. The intestinal mucosa and the digestive glands have normally a very rapid proteins turn over (the continuous synthesis and degradation of proteins). Thus, a child with protein deficiency malnutrition suffers failure of digestion and absorption of food that results in diarrhea, loss of water in stool and aberration of electrolytes. Liver also fails to perform its normal functions. Fats accumulate in the hepatocytes due to lack of lipotropic factors that have to come from proteins and amino acids and also due to decreased synthesis of lipoproteins. The liver fails to synthesize albumins that results in reversal of albumin/globulin ratio in plasma, leading to tissue edema.
Protein deficiency leads to a failure in the maintenance of the integrity of skeletal muscle and may lead to muscle wasting and atrophy. It manifests promptly in the decreased biosynthesis of hemoglobin and red blood cells and a nutritional anemia ensues in severe protein deficiency [3]. Also, the glandular tissues are affected and their functions are compromised due to their protein depletion. The proteins of the heart muscle, central nervous system and brain remain intact even in moderately severe protein deficiency. However, a decreased mental function and loss of memory may ensue in such conditions.
According to World Health Organization protein energy malnutrition is the most serious public problem in under-developed countries and infant mortality in these countries is 20- 50 folds higher than in the USA, Europe and other prosperous countries [3].
Kwashiorkor, marasmus, and marasmic kwashiorkor are some of the clinically defined manifestations seen in children subjected to prolonged malnutrition. Both kwashiorkor and marasmus are protein energy malnutrition. In kwashiorkor, the contribution of protein malnutrition is quite high and there is edema. Both kwashiorkoric and marasmusic children suffer from caloric inadequacy and secondary protein deficiency. Marasmic kwashiorkor is an intermediate stage between kwashiorkor and marasmus, which is a combination of both that, is characterized by less defined forms. Vitamins’ deficiency accompanied by protein-energy malnutrition, mal-absorption syndrome, intestinal infections, diarrhea etc. lead to nutritional dwarfing or marasmus (a wasting of flesh without fever or apparent diseases especially in infants).
In the present study, among the 78 subjects studied 29(37.2%) were females and 49(62.8%) were males. This is in line with a previous study conducted in Botswana [13]. In our case, more than half of the PEM affected children were from the rural areas, the majority of the affected children 36 (46.2%) were from Hawsa Tribe, an African tribe with their own colloquial language and nutritional culture. Children of the isolated tribal communities were more susceptible to malnutrition; this might due to low socioeconomic status, integration in the local communities, illiteracy, nutritional practices and higher fertility rate.
Our study showed that underweight was the commonest in 24 (30.8%) children, followed by Marasmus in 18 (23.1%) children. Our findings were in line with a previous study [14,15] which reported that there were 38.2% underweight children, marasmus and kwashiorkor were found in 6.4% and 0.9% children respectively and no case of marasmic-kwashiorkor was found in the studied subjects. Cartmell et al. (1981) reported that kwashiorkor and marasmus were the most common types among children in Maputo in 1983. However, the cases were changed to kwashiokor and marasmic-kwashiokor in 2001. Also, Chakraborty et al. [16] found more cases of marasmic patients among males aged less than a year. This might give an indication that there are no constant geographical patterns in children malnutrition that can predict the type of PEM but it seems that malnutrition in children is affected by many factors.
Seventy two (92.4%) of the affected children were in the age group of 0-3 years; this age group showed significantly higher frequency of PEM compared to other age groups (p= 0.000), and this results agrees with [17,18]. Illiteracy and low socioeconomic status which includes poverty was observed in families of affected children in the present study; illiteracy of mothers was significantly important risk factor involved in PEM with p = 0. 034. Abdalla et al. [3] reported that mother's education was to be key factor in prevention of malnutrition in children. Also, Chatterjee (1990) reported that children of illiterate mothers are three times as likely to be severely under-nourished compared to children of mothers with at least a high school education. The percentage of the Laborers in this study was highest 52 (66.7%) followed by farmers 23(29.5%). Chakraborty et al. [18] found significant difference in prevalence of PEM among children of laborers and farmers in comparison to those who were in service/business/skilled professions. Srivastava (1983) reported that prevalence of PEM amongst children were highest among families of labor class compared to other classes. All these findings about the causes of malnutrition in children proved that education of parents especially mothers was the most important factor in fighting malnutrition in children. Education is a powerful emancipator that provides knowledge for better understanding of all things including food values, importance of hygiene, importance of prevention of diseases; it secures jobs, provides better income and it fights poverty.
The number of family size is an important factor in children healthiness. In the present study, the association of family size with PEM was found to be significant (p=0.02); this finding agrees with previous studies. Ejaz and Latif (2010) found that children who were of the first or second birth order were at the lower risk for malnutrition. Low rate of breast feeding and sudden weaning were observed. Small family size allows mothers for providing more care to their children and also allows mothers to control breastfeeding for suitable period and to introduce suitable food during the gradual weaning that can help in avoiding sudden weaning.
PEM is also associated with a number of co-morbidities such as tuberculosis, diarrhea, malaria and anemia [16]. Ubesie et al. [9] reported that diarrhea and malaria were the most common co-morbidities. In this study, diarrheal diseases and anemia were the most common associated diseases representing 37 (47.4%) and 21(26.9%) of the children, respectively. 51 (65.4%) of children were recovered and discharged with good condition while 4(5.1) children died due to hypothermia, severe dehydration and hypovolemic shock [19].
In Gadarif, Sudan, PEM was due to low socioeconomic status, illiteracy and large family size. As malnutrition is a multi-factorial disease, for its effective management, multiple and synergistic interventions embedded through multi-sectorial programs must be followed that include intervention programs in agriculture and micronutrients and provision of healthy drinking water, nutritionbased education with special emphasis on elderly people, pregnant women and children, and provision of balanced-quality health services [5]. Lastly implement the UN 7 goals of the Millennium Summit in 2000: universal primary education; empowerment of women; improved maternal health; decreased child mortality; advances in the prevention and management of HIV/AIDS, malaria and other diseases; environmental protection; and global partnerships for development [5].
The authors declare that, they do not have any conflict of interest regarding this study.
The authors are very thankful for the children included in this study and for their parents. Also, the authors are grateful to the staff of Gadarif Pediatrics’ Teaching Hospital for their cooperation during the conduct of this study.
All the authors conceived and designed the study, achieved its implementation, its data collection and analysis and drafted the final manuscript. All the authors have read and approved the final version submitted.
Citation: Ahmed MAA, Massaad SO, Abdalla KO, Omar SM, Adam GK (2019) Protein Energy Malnutrition in Children at Gadarif Eastern Sudan. J Nutr Food Sci 9:758.
Received: 04-Apr-2019 Accepted: 15-May-2019 Published: 23-May-2019 , DOI: 10.35248/2155-9600.19.9.1000758
Copyright: © 2019 Ahmed MAA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.