Journal of Nutrition & Food Sciences
Open Access
ISSN: 2155-9600
ISSN: 2155-9600
Research Article - (2025)Volume 15, Issue 2
Background: A large proportion of hospital patients are malnourished. At admission, approximately 30% to 50% of patients are at risk of malnutrition, and many of these patients experience further nutritional decline during their hospital stay. Malnutrition in hospitalized patients has significant clinical consequences, including an increased risk of medical complications, a longer length of stay, and a lower quality of life in adult patients. Despite this there is a scarcity of evidence on the change in nutritional status among adult hospitalized patients and the factors that influence it.
Methods: From June 1 to July 30, 2021, a hospital-based prospective cohort study involving 270 medical, surgical, and gynecologic wards admitted adult patients aged 18 years was conducted at Mettu Karl Compressive Specialized Hospital. At admission and before discharge, the patient's nutritional status was assessed within 24 hours using the subjective global assessment. The chi-square and student t-test were used to determine the statistical difference between nutrition change category and outcome variable groups. The predictors of declining nutritional status were identified using logistic regression models. In all hypothesis tests, a statistical significance of 0.05 was used.
Results: On admission, a total of 270 patients were included, of these 203 patients had stayed greater than 7 days in the hospital and measured both subjective global assessment at admission and discharge. The median length of stay in the study population was 10 days (8, 12). Overall 31% improved, and 19.2% declined nutritionally from admission to discharge. Odds of occurrence of complications were significantly greater (OR=2.274, 95% CI, 1.052, 4.915), patients with deteriorated nutritional status had longer length of stay in the inpatient treatment.
Conclusions: In this study, less number of patients declined their nutritional status during hospitalization. Being female, older age, and poor nutritional status at admission are the predictive factors that contribute to nutritional declination during hospitalization.
Hospital malnutrition is a widespread problem that has an impact on clinical outcomes worldwide [1-3]. Malnutrition in hospitals was first identified by Charles Butterworth before the 1970’s; defining malnutrition is frequently overlooked, undiagnosed, and undertreated in hospitals, resulting in adverse clinical effects [4]. Hospital malnutrition does not have a universally accepted definition. Malnutrition has been defined by Soeters and fellows as any form of nutrient imbalance, including under and overnutrition: Over nutrition (intakes in excess of dietary requirements) and under nutrition (intakes less than dietary requirements), with adverse effects on body composition and associated clinical outcomes among hospitalized patients [5].
Malnutrition in admitted patients is typically associated with under nutrition as a result of decreased intake and increased metabolic rate disease. Malnutrition, as defined in clinical nutrition, is a change in nutritional status caused by an illness, its complications, or treatment procedures during a hospital stay. The combination of these factors changes in tissue shape and body composition, which have been linked to poor clinical outcomes during hospitalization [6].
Malnutrition in hospital subclinical care settings has been reported to be up to 65 % worldwide [7]. An estimated 40% of the patients were malnourished upon admission, and 75% of patients who stayed in the hospital for more than one week lost weight during their stay [8]. Only a few studies on changes in nutritional status during hospitalization have been published in developed countries. Two studies reported that 20% of patients admitted during a hospital stay had a decline in nutritional status and another study found that 25% of patients had a decline in nutritional status while being hospitalized [9].
A prospective observational single center study with a retrospective component was conducted in the United States of America to assess changes in nutritional status in 404 patients using Subjective Global Assessment (SGA) at admission and discharge [10]. The findings revealed that a decline in patients' nutritional status during hospitalization, regardless of their nutritional status at admission, was associated with significantly higher hospital charges as well as a higher likelihood of complications and Length of Stay (LOS) in patients who stayed for more than 7 days. When testing the associations between nutritional status and LOS, no covariate adjustment for demographics or co morbidities was performed. In Italy examined the associations between malnutrition and prolonged LOS (>17 days) while controlling for several potential nutritional and clinical confounders recorded at admission and collected during and at the end of the hospital stay. They discovered that a nutritional risk index of less than 97.5 at admission and an inhospital weight loss of 5% were linked to a longer LOS. One of the confounders in that study, the physician-assessed severity score, was performed only within 36 hours of admission and was not repeated at discharge. Furthermore, because the nutritional risk index is a weight-based measure, patients with edema were excluded from the study.
According to Ethiopia's 2014 report, the prevalence of hospital malnutrition among adult patients was 55.6%. This study, on the other hand, was primarily concerned with their nutritional status at the time of admission [11]. There is a scarcity of evidence addressing changes in nutritional status that occur in hospitalized patients and how these are related to the occurrence of complications and length of hospital stay in general adult admitted patients from Ethiopia. There are no other studies assessing nutritional status and associated factors in adult hospitalized patient populations, and no multi-center studies. Furthermore, no studies have taken into account the factors associated with in-hospital nutritional status changes.
There is a scarcity of evidence addressing changes in nutritional status that occur in hospitalized patients and how these are related to the occurrence of complications and length of hospital stay in general adult admitted patients from Ethiopia. This study is expected to fill this gap by providing scientific information and knowledge about changes in nutritional status among adult hospitalized patients and the associated factors in MKCSH in South-West Ethiopia.
Study area and study period
The study was conducted in Ilu Aba Bor zone, Mettu Karl compressive specialized hospital in Southwest Ethiopia. Mettu Karl Referral Hospital is one of the Oromia regional national state's zonal hospitals. The Hospital is located in the heart of Mettu Town, the capital city of the Ilu-Aba bor Zone. It is the only governmental hospital in the town, which is located 595 kilometers South-West of Addis Ababa. It was founded in 1932 by Swedish Missionaries and Ras Teferi. It currently provides full health care services to the estimated 1.5 million people in the Ilu-Aba bor zone and its surroundings. There are a total of 180 beds in the surgical, medical, gynecology-obstetrics, and pediatrics wards of the hospital and the annual bed occupation rate of the hospital is 97.68%. Data was collected from adult patients admitted to the hospital for medical treatments and procedures between June 1 and July 30, 2021.
Study design
A hospital-based, single prospective cohort study was conducted.
Source population
All adult inpatients who were admitted in Mettu Karl compressive specialized hospital.
Study population
All adults who were admitted >24 hours, in the selected wards from June 1-30, 2021, and who are eligible for the study.
Inclusion and exclusion criteria
Inclusion criteria: The study will include all adult patients over the age of 18 and those admitted for more than 24 hours to the surgical, medical, and gynecologic wards between June 1 and July 30, 2021.
Exclusion criteria: The study excluded critically ill and psychiatric patients, lactating mothers, pregnant mothers, palliative care patients, and patients over the age of 65.
Sample size determination
To calculate sample size, single population proportion formula was used considering the in-hospital changes in nutritional status 20%, with a 95% confidence interval and a 5% margin of error [12].
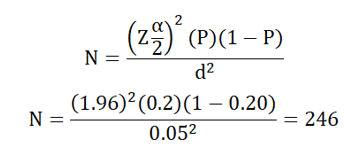
By considering a non-response rate of 10%, 271 samples were taken.
Sampling procedure
The MKCSH wards that met the inclusion criteria were compiled into a list. There are three types of eligible wards: Medical, surgical, and gynecology. The number of patients recruited from each ward is calculated using the total number of beds (154) available in each ward-category. A selection of newly admitted patients (24 hour admission) was recruited each morning per ward when possible. The procedure was repeated until the sample size for the study was reached.
Data collection tools and process
A service for admitted adult in-patients was chosen. Patients admitted for 24 hours are identified directly from medical, surgical, and gynecologic wards participating in medical treatment or procedures at MKRH. The participant's nutritional status was then evaluated using a Subjective Global Assessment (SGA). A review of medical records for all participants on patients' demography, ward admission, primary admission diagnosis, presence/absence of cancer, history of surgery while hospitalized or within 3 months before admission, and presence or absence of complication was recorded at admission [13].
Each day, patients were randomly selected for inclusion in the study. The nutritional status of the patients was assessed at admission and discharge using two different measurement forms of Subjective Global Assessment (SGA). The admission data collection form was only completed within 24 hours of admission. The discharge data collection form was completed only for patients who had a hospital stay of more than 7 days prior to discharge. As a result, the study sample only included a patient's hospital stay of more than 5 days, as well as both SGA admission and discharge ranking.
Study instrument
Subjective Global Assessment (SGA) is a tool that evaluates nutritional status based on recent weight loss, dietary changes, and a physical examination of subcutaneous fat, muscle mass, and fluid balance. Baker et al. first described the Subjective Global Assessment (SGA) in 1982, which assesses the patient for malnutrition at the bedside without the need for precise body composition analysis [14]. The anthropometric measurements are required for this study is the weight. Anthropometry measurement is required for SGA and was collected at admission/discharge data collection form. Bodyweight will be measured in light clothes with shoes off using electronic portable scale in the hospital will measure to the nearest 0.5 kg.
Takei physical strength dynamometer was used to assess the patient’s functional status. This data is needed to complete the SGA. Participants will be asked to perform maximal contraction with the dominant hand and to hold it for a few seconds. Measurement will be taken on stand upright shoulders back, with feet even and hip-width apart, the elbow positioned in a complete extension, and the arm not supposed to touch any part of the body, in a neutral position, with the instrument in their dominant hand. If the patient is unable to stand, the measurement was taken in a seat position. All clinical examination was performed for the presence of subcutaneous fat loss, signs of muscle wasting, and the presence of edema for SGA sore. The researcher was assessed the patient for subcutaneous fat loss by assessing the patient’s lumbar, upper arm, orbital and thoracic regions. Muscle wasting is assessed by evaluating the quadriceps and deltoids part of the patients. Findings are interpreted according to the established SGA. The researcher was assessing the patient for edema around the ankle, sacral, and abdomen for ascites. The findings were interpreted according to the established SGA. The Carlson co morbidity index was assessed to classify the prognostic co morbidity. The CCI predicts the 10-year mortality for a patient who may have a range of co morbid conditions (up to twenty-two conditions), where each condition is assigned a score of 1, 2, 3, or 6, depending on the risk of dying associated with it. Scores are summed to provide a total score to predict mortality. Based on the CCI score, the severity of co morbidity is categorized into three grades: Mild, with CCI scores of 1-2; moderate, with CCI scores of 3-4; and severe, with CCI, scores ≥ 5. The higher the score, the more likely the predicted outcome will result in mortality or higher resource use. Numbers of medications will be collected from medical records. Poly pharmacy is defined, as the use of five or more medications daily.
Data quality management
A pretest was conducted prior to one week of actual data collection to ensure the consistency and clarity of the questionnaire. The data extraction checklist was then modified based on the results, such as missing words. Three days before data collection, the supervisor and data collectors were trained on the overall objectives of the research and how to extract information. At the start of the interview, the respondents were given a clear explanation of the purpose of the study. During data collection procedures, the supervisor and principal investigator provided close supervision. The data collectors and principal investigator reviewed each respondent's data for completeness, clarity, and consistency.
Operational definitions
Change in nutritional status: Is a difference between SGA measurement at admission who admitted ≥ 24 hrs and a patient stayed ≥ 7 days and before on SGA.
The decline in nutritional status: Is a change that shows SGA A at admission to SGA B or SGA C at discharge and SGA B at admission to SGA C at discharge.
Improved nutritional status: Is defined as the nutritional status of SGA C at admission moving to SGA B or A by discharge and SGA B moving to SGA A by discharge.
LOS: Is defined as the difference (days) between the date of discharge and the date of admission to the hospital.
Complication: A complication was defined as a state in which a disease or accident is added to an existing illness without being related specifically to illness (any complication).
Data analysis procedure
Data was manually cleaned and entered into Epi-data version 4.4.2.1, where it was checked and cleaned for consistency and missing values before being exported to IBM statistics version 25 for analysis. First, SGA classified changes in nutritional status as normal to normal (reference group), normal to moderate, normal to severe, moderate to normal, moderate to moderate, moderate to severe, severe to normal, severe to moderate, severe to severe, and severe too severe. Participants were divided into three groups for further analysis: Group N, improve, and decline. Data was analyzed by comparing those who declined nutritional status and those who did not decline nutritional status to assess how outcomes varied according to classification. The variables were described using summary statistics (frequency table, mean and median, SD). The nutritional status was classified into three groups using the Chi-square and student ttest. A samples t-test was used to test the relationship between continuous factors of interest and nutritional decline. To identify predictors of a decline in nutritional status, multinomial logistic regression models with 95% CI were used to calculate the Odd Ratios (ORs). In all hypothesis tests, a statistical significance of 0.05 was used.
Description of study participants
During the total of two months of the study period, 270 patients were admitted, among this 67 patients exclude who were discharged within less than seven days and nutritional measurement at discharge was not done. The remained 203 patients were included in this study, whose SGA measured both at admission and discharge, and stayed for >7 days in the ward. The majority of the study participants 114 (56.2%) admitted to general medicine, followed by surgery 79 (38.9%), and gynecology ward 10 (4.9%).
Socio-demographic characteristics of participants
The study participants were aged from 18 to 65 years with median age was 45. From 203 participants 88 (43.4%) were male and 115 (56.6%) were female. In this study 90 (44.3%) of the respondents are orthodox, and 175 (86.3%) were married. Almost one-fourth of 45 (22.2%) participants completed their primary school, and 65 (32.2%) of respondents were government employed (Table 1).
| Characteristics | Category | Number | Percent (%) |
|---|---|---|---|
| Sex | Male | 88 | 43.4 |
| Female | 115 | 56.6 | |
| Total | 203 | 100.0 | |
| Age in year | 18-32 | 60 | 29.6 |
| 33-45 | 69 | 33.9 | |
| 46-65 | 74 | 36.5 | |
| Total | 203 | 100.0 | |
| Educational status | Unable to read and write | 28 | 13.8 |
| Able to read and write | 27 | 13.3 | |
| Primary level (1-8) | 45 | 22.2 | |
| Secondary level (9-12) | 39 | 19.2 | |
| Technical/Vocational | 26 | 12.8 | |
| Higher (University) | 38 | 18.7 | |
| Total | 203 | 100.0 | |
| Marital status | Single | 13 | 6.4 |
| Married | 175 | 86.3 | |
| Divorced | 11 | 5.4 | |
| Widowed | 4 | 1.9 | |
| Total | 203 | 100.0 | |
| Occupational status | Government employed | 65 | 32.2 |
| Unemployed | 21 | 10.3 | |
| Merchant | 48 | 23.6 | |
| Farmer | 62 | 30.5 | |
| Student | 7 | 3.4 | |
| Total | 203 | 100.0 | |
| Religion | Orthodox | 90 | 44.3 |
| Catholic | 5 | 2.5 | |
| Protestant | 77 | 37.9 | |
| Muslim | 31 | 15.3 | |
| Total | 203 | 100.0 |
Table 1: Socio-demographic and clinical characteristics of adult hospitalized patients in MKCSH, Mettu, Ethiopia, 2021.
Clinical characteristics of participants
Out of 203 patients, 50 (24.6%) were under SGA A, 125 (61.6%) were SGA B and 28 (13.8%) were SGA C at admission. The median hospital LOS of the study participant was 10 (8-12) days. 112 (55.2%) of the study participants have developed a medical complication during their hospital stay. The overall prevalence of malnutrition (SGA B or C) on admission is 153 (75.4%). Out of 153 malnourished participants, 104 (68%) is evident among medical patients, 43 (28.1%) among surgical patients, and 6 (3.9%) among gynecology unit patients. The primary diagnosis of most patients included in our study was a gastrointestinal disease 43 (21.2%).
Change in nutritional status from admission to discharge
At the time of discharge, all 203 patients were reassessed using the SGA discharge assessment and 80 (39.4%) were SGA A, 98 (48.3%) were SGA B and 25 (12.3%) were diagnosed as SGA C. The incidence of malnutrition at discharge (SGA=moderately and severely malnourished) was 124 (61%). Twenty-three subjects 28 (13.8%) were stayed well-nourished, fifty-two subjects 63 (31%) improved, and 38 subjects (18.7%) declined in nutritional status defined by the SGA category between admission and discharge, described in Table 2.
| SGA at admission | SGA at discharge | Total number (%) | ||
|---|---|---|---|---|
| Normal number (%) | Moderate number (%) | Severe number (%) | ||
| Normal | 28 (13.8%) | 17 (8.4%) | 5 (2.5%) | 50 (24.7%) |
| Moderate | 45 (22.3) | 64 (31.4%) | 16 (7.8%) | 125 (61.5%) |
| Severe | 6 (2.9%) | 17 (8.4%) | 5 (2.5%) | 28 (13.8%) |
| Total | 79 (39%) | 98 (48.2%) | 26 (12.8%) | 203 (100%) |
Table 2: The nutritional status of patients between admission and discharge in MKCSH, Mettu, Ethiopia, 2021.
78 (38.4%) of patients lose their weight during hospital admission. Weight loss was observed in 14 (6.9%) of 79 (38.9%) normally nourished patients, 43 (21.2%) of 98 moderately malnourished, and 20(9.8%) of 26 severely malnourished patients.
Overall, 38 (18.7%) of patients during admission to the hospital experienced a decline in nutritional status between admission and discharge. Specifically, 17 of 41 (8.4%) experienced a decline in nutritional status who were admitted as SGA A and discharged SGA B; 5 of 50 (24.7%) experienced a decline in nutritional status who admitted as SGA A and discharged SGA C, and 16 (7.9%) experienced a decline in nutritional status patients admitted as SGA B to discharged SGA C were experienced a decline in nutritional status.
Nutritional status and hospital length of stay
The median length of hospital stay in our study was 10 (8-12) days. The longer mean length of hospital stay was recorded on a patient admitted normally nourished and discharge severely malnourished patients (13 days) (Table 3).
| Outcome variables | Change groups | N | Mean | Std. deviation | Std. error mean | p-value |
|---|---|---|---|---|---|---|
| Length stay | Group N | 29 | 8.17 | 1.100 | 0.206 | |
| Improved | 63 | 9.27 | 2.078 | 0.288 | 0.016 | |
| Declined | 38 | 12.10 | 1.557 | 0.280 | 0.001 |
Table 3: Independent sample t-test for nutrition change groups in MKCSH, Mettu, Ethiopia, 2021.
Significant differences in the length of hospital stay were observed between the three nutrition change groups. The declined nutritional status groups were significantly longer mean length of stay (12 days) (p<0.001) compared with a patients improved in nutritional status (9 days) (Table 4).
| Admission SGA | Discharge SGA | Patients number | P-value | OR | 95%, CI |
| Normal | Normal | 28 (13.8%) | 0.012 | 1.0 | |
| Normal | Moderate | 17 (8.4%) | 0.001 | 4.813 | 1.9 2, 12.00 |
| Normal | Severe | 5 (2.5%) | 0.246 | 0.385 | 0.077, 1.93 |
| Moderate | Normal | 44 (21.7%) | 0.034 | 3.812 | 1.01, 13.12 |
| Moderate | Moderate | 65 (32%) | 0.004 | 4.84 | 1.67, 13.97 |
| Moderate | Severe | 16 (7.9%) | 0.999 | 0.000 | 0.000 |
| Severe | Normal | 6 (2.9%) | 0.802 | 0.847 | 0.232, 3.09 |
| Severe | Moderate | 17 (8.4%) | 0.582 | 0.555 | 0.57, 5.14 |
| Severe | Severe | 5 (2.5%) | 0.999 | 0.000 | 0.000 |
Table 4: Multivariate Odds Ratio (OR) and 95%, CI for the risk of complication during hospital stay by nine group nutritional status category between admission and discharge, in MKCSH, Mettu, Ethiopia, 2021.
Nutritional status and complication
The crude odds ratios for the risk of complications in declined (OR=2.274, 95% CI, 1.052, 4.915) compared with improved (OR=1.158, 95% CI 0.463, 2.895) patients, and chi-square test explores significant differences in the occurrence of complications seen at p-value=0.006. Patient’s those there nutritional status decline were experiences a high percentage of complications as compared improved nutritional status.
The odds of occurrence of complications by the change nutrition group are shown in Table 5. More complications were found among admitted normally nourished and discharged moderately malnourished patients and patients admitted moderately malnourished and discharged moderately malnourished compared with patients admitted and discharged normally (OR=4.8, 95% CI, 1.9 2,12 and OR=4.8 95% CI, 1.67, 13.9).
| Variable | Bivariate | Multivariate | |||
|---|---|---|---|---|---|
| OR (95%, CI) | p-v | OR (95% CI) | p-v | ||
| Sex | Male | 1 | |||
| Female | 7.33 (2.1, 25.149) | 0.002 | 10.8 (2.87, 40.8) | 0.001 | |
| Ward type | Gynecologic | 1 | |||
| Medical | 0.43 (0.14, 1.3) | 0.14 | 0.57 (0.11, 2.8) | 0.50 | |
| Surgical | 0.91 (0.2984, 2.78) | 0.87 | 0.45 (0.77, 2.69) | 0.38 | |
| SGA at admission | SGA A | 1 | |||
| SGA B+C | 3.92 (1.79, 8.7) | 0.001 | 4.75 (1.8, 12.3) | 0.001 | |
| Age category | 18-32 | 1 | |||
| 33-47 | 2.18 (0.78, 6.18) | 0.143 | 2.8 (0.88, 9.2) | 0.08 | |
| 48-65 | 2.79 (0.99, 7.8) | 0.051 | 3.7 (1.17 , 12.1) | 0.02 | |
| CCI | No CCI | 1 | |||
| Mild | 1.88 (0.5, 7) | 0.34 | 1.8 (0.4, 7.5) | 0.42 | |
| Moderate | 1.76 (0.76, 4.5) | 0.18 | 1.46 (0.47, 4.5) | 0.51 | |
| Sever | 1.72 (0.49, 7.4) | 0.46 | 2.24 (0.8, 1.5) | 0.32 | |
| Presence of cancer | No | 1 | |||
| Yes | 0.0 (0) | 0.999 | |||
| Presence of infection at admission | No | 1 | |||
| Yes | 1.22 (0.57, 2.6 | 0.59 | |||
| Number of medication | 0-3 | 1 | |||
| 4-6 | 0.86 (0.38, 1.9) | 0.72 | |||
| History of surgery | No | 1 | |||
| Yes | 0.9 (0.2, 4.2) | 0.92 | |||
| A surgical procedure in hospital | No | 1 | |||
| Yes | 0.39 (0.18, 0.83) | 0.016 | 0.4 (0.88, 1.8) | 0.25 | |
Table 5: Bivariate analysis and multivariate analysis for predictors of nutritional decline in MKCSH, Mettu, Ethiopia, 2021.
Predictors of nutritional decline
On bivariate analysis, female sex the patient diagnosed the nutrition category at admission SGA B+C (p=0.002), age group of 48-65 (p=0.05), and surgical procedures during admission time (p=0.016) were found significant at 25%. Multivariate analysis found that patients admitted with some compromise of nutritional status at admission (SGA B+C) (p=0.005) and patients increase in age 48-65 (p=0.009) are highly significant for the nutritional decline.
This study shows that in patients hospitalized for greater than seven days in Mettu Karl Compressive Specialized Hospital to assess changes in nutritional status during hospitalization and its associated factor using Subjective Global Assessment (SGA). According to this study, the incident of malnutrition in Mettu Karl Compressive Specialized Hospital at admission was 75%, and 61% at discharge among adult hospitalized patients. About thirty-one (18.7%) of patients declined their nutritional status during hospitalization. Patients whose nutritional statuses declined during hospitalization had a greater proportion of complications (64%) and experienced longer lengths of stay (12 days) than well-nourished patients. In this study the majority of patients experienced gastrointestinal diseases.
This study found a high rate of malnutrition among patients admitted to Mettu Karl Compressive Specialized Hospital. This finding is higher than that of studies conducted in Amhara National Regional State (55.6%) and South Africa (72.8%) in 2006 [15]. This difference in incident could be due to the clinical condition of patient characteristics or the primary disease diagnosis.
SGA was used in this study to investigate changes in nutritional status by the time of discharge. Between admission and discharge, there was a change in nutritional status. Malnutrition has been reduced to 61% at discharge. Even though the results of this study show that the incidence during discharge has decreased, the figure remains higher. This could be due to minor improvements in functional capacity or dietary intake during their hospitalization. According to the Subjective Global Assessment (SGA) in this study, the majority of patients in the admission sample had mild to moderate malnutrition compared to the discharge sample. The findings show that there was a higher incidence of malnutrition in the admission sample, as well as more severe cases of malnutrition at admission. Similar findings were obtained in the Brazilian National Survey, where despite fewer patients diagnosed as malnourished at discharge investigated using SGA, and also in studies conducted in South Africa Tygerberg Hospital, where the incidence of malnutrition at discharge was reduced when SGA was used [16].
A decline in nutritional status was observed in 19% of the participants in this study. This study was supported by Johane P. Allard (19.8%), Carol Braunschweig (31%), and Yildirim (25%), who experienced nutritional decline while hospitalized [17]. In our study, the decline in nutritional status could be attributed to poor hospital food services, patients' lack of food choices, or insufficient food intake. Patients who do not finish their meals should be considered to be at an increased risk of acquiring a significant protein-energy deficit within few days of admission and further decline in nutritional status through hospital stay, according to a 2006 study [18].
The failure to detect hospital malnutrition at admission and discharge, as well as health professionals' lack of awareness of malnutrition, may result in a patient's nutritional status deteriorating. Patients in our study area are traditionally discharged based on clinical improvements. Identifying patients at admission should result in a nutrition care algorithm that includes confirmation of the nutrition risk or malnutrition, as well as monitoring for those who were detected and required treatment and specific nutrition intervention to prevent further nutritional decline. Age, low literacy level, low income, and lack of family support during hospital stay are socio-demographic factors that influence nutritional status. Improvement in nutritional status was seen in 31% of our studies, compared to 17.4%, 31%, and 31% in the other studies. These differences may be characteristics of the patient (length of stay).
The current study looked at the relationship between nutritional status decline and the occurrence of complications and length of hospital stay. The relationship between nutritional status at admission and the occurrence of complications and length of hospital stay has been described, but information on the relationship between decline nutritional status and length of hospital stay is scarce at discharge. In this study, patients with poor nutritional status were more likely (62%) to have complications than patients with normal nutritional status during hospitalization. According to a study by Carol Braunschweig, the odds of a complication were higher for patients who declined nutritionally. Similarly, a study conducted in the United State showed patients who experienced a decline in nutritional status during their admission experience more complications (64%) than the patient's normal nutritional status. Naber et al reported that the incidence of any complication was higher among nutritionally compromised patients compared with well-nourished patients.
A study found that malnourished patients are more likely to develop co-morbid complications. These variations could be due to the number of complications, the organ system affected by a complication, or the severity of the disease. Furthermore, there was a significant difference in nutritional status and the presence of complications, with malnourished patients experiencing more complications than non-malnourished patients. Complications during hospitalization were more likely to occur in patients admitted who were normally nourished and discharged moderately malnourished, according to this study. Furthermore, more complications have been discovered in nutritionally compromised patients who have been admitted and discharged [19].
This study discovered that patients who declined nutritionally had a longer length of stay (12 days) than patients who were admitted and discharged normally by an average of 4 days. This data, which corresponded to a previous study conducted in the United States, looked at adult patients hospitalized for more than 7 days and examined the impact nutritional decline had on clinical outcomes.
Findings revealed that patients admitted with some degree of malnutrition, as well as those who experienced a decline in nutritional status during their admission, had significantly longer hospital stays (by an average of 4 days) than patients both admitted and not admitted with some degree of malnutrition. Findings in an Australian hospital revealed a significantly greater difference of 5 days between the length of stay of malnourished and non-malnourished patients. Similarly, a study found that patients who were identified as malnourished had a significantly longer length of stay than those who were not. The differences in duration could be attributed to patients' clinical conditions (disease category), such as those diagnosed with tuberculosis or undergoing surgery. Patients who were admitted normally nourished and discharged severely malnourished had a longer mean (13.20.5) length of stay, which is lower than the (234.6) length of stay found in a study by Carol Braunschweig. The difference could be the length of treatment.
The predictive factors that contribute to nutritional decline were also evaluated in this study, and we discovered that being of the female sex, being older, and having poor nutritional status at admission were significant contributing factors for the decline in nutritional status during hospitalization, which is consistent with the findings of a study by Johane P. Allard. Findings in Canada show that female gender, age, and medical condition are significant predictors of nutritional decline in surgical patients during hospitalization. Similar to the findings of a study conducted in Spanish public hospitals, age and medical condition were significant contributors to nutritional decline [20]. This finding was made possible by the fact that personal factors such as age, gender, physical, psychological, social, and medical conditions all have a significant nutritional impact on hospital admission.
During hospitalization, approximately 19% of patients' nutritional status deteriorated. A decline in nutritional status was found to be significantly related to a longer length of stay and a higher risk of complication. According to this study, female sex, old age, and poor nutritional status at admission were factors that predicted a decline in nutritional status of the study participant at discharge.
Based on the findings, the following stakeholders were suggested: To establish a protocol for implementing how to screen patients for nutritional status at admission and reassess at discharge in order to reduce patient nutritional status decline and its consequences.. Health care providers should assess patients' nutritional status before discharge to reduce decline in nutritional status and consider re-assessing nutritional status before discharge. Because this study may not provide representative evidence of the Ethiopian heterogeneity population, a large prospective multicenter study should be conducted to confirm the findings of malnutrition at admission and discharge.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Dagne D, Negera E, Debalke R, Alemu S, Zeinu S (2025) Change in Nutritional Status and Its Associated Factors among Adult Patients Admitted to Mettu Karl Compressive Specialized Hospital in Southwest Ethiopia: A Prospective Cohort Study. J Nutr Food Sci. 15:066.
Received: 11-Sep-2023, Manuscript No. JNFS-23-26785; Editor assigned: 13-Sep-2023, Pre QC No. JNFS-23-26785 (PQ); Reviewed: 27-Sep-2023, QC No. JNFS-23-26785; Revised: 14-Jun-2025, Manuscript No. JNFS-23-26785 (R); Published: 21-Jun-2025 , DOI: 10.35248/2155-9600.25.15.066
Copyright: © 2025 Dagne D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.