Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Case Report - (2022)Volume 12, Issue 1
The imperforate hymen is one of the most frequent malformations of the female genital tract. The clinical presentation varies from the asymptomatic form to symptoms caused by the obstructive effect of the hematocolpometra such as primary amenorrhea, abdominal and lumbar pain, constipation, dysuria and urinary retention. We report the case of an adolescent whose only symptoms were acute urinary retention associated with severe pelvic pain. In the presence of symptoms such as abdominal and cycliclumbar pain, pelvic swelling, urinary retention or constipation in a premenarchal adolescent with a discrepant tanner stage pubertal development, the diagnosis of imperforate hymen should be considered. The external genitals were inspected, showing an imperforate, bulging and translucent hymen. Bladder catheterization was performed and 1300 ml urine of sui generis characteristics was drained, with immediate symptomatic relief. On ultrasound, the vagina was distended byanechoic content, which was also filling the whole uterine cavity corresponding to bulky hematocolpos and hematometra. The findings were verified by a gynecologist after testing with anesthesia and hematocolpos was diagnosed. This is a case report of lower abdominal pain as a result of an imperforate hymen causing haematocolpos.
Hematocolpos; Hematometra; Hymen; Bladder; Pelvic
Imperforate hymen is the most common obstructive anomaly of the female reproductive track. Estimates of the frequency of imperforate hymen vary from 1 in 1000 to 1 in 10,000 females. It must be diagnosed at birth by the paediatrician; but imperforate hymen is most often diagnosed in adolescent girls after the age of menarche with otherwise normal development, if it is not diagnosed and be treated it will presents complications at puberty such as blood collection inside the vaginal cavity (hematocolpos), urinary retention, amenorrhoea and pelvic pain or a risk of secondary endometriosis.
The diagnosis of an imperforate hymen is usually made based purely on the physical exam, although transabdominal ultrasonography is sufficient for imperforate hymen diagnosis but MRI provides more details on hymen thickness enabling choice of the appropriate surgical technique a thick hymen needs surgical resection; a thin hymen only needs a vertical incision.
A healthy 13 year-old girl, fully immunized, presented to pediatric emergency with a two weeks history of lower right abdominal pain which has recently worsened and caused urinary retention. There was no history of vomiting or a change in bowel habit. Her birth history and developmental history were unremarkable. On examination, vital signs showed blood pressure 110/70 mm/Hg, Pulse 100 (bpm) regular, breathing 20 per minute, proper capillary filling, temperature 37.5ᵒC, on auscultation good air entry to two lungs, regular heart beats. Her abdomen was soft with mild tenderness suprapubic and in the left iliac fossa without organomegaly. No rash on limbs or other sites on the body and neurologically without side marks.
Laboratory findings showed normal urine dipstick, and a urinary pregnancy test was negative. CRP=2, leukocytes 10000 per microliter without shift to left, hemoglobin 13%, platelets 365000 mcl. Normal PT/PTT coagulation factors. Chemistry normal kidney function Creatinine 0.7, Urea 10 normal electrolyte normal liver function SGOT14, SGPT10 potassium 4, Phosphorus 3.5, Calcium 9.4 normal CPK 53, albumin 4.48, globulin 3 imaging abdominal ultrasound of the spleen, liver, and external bile ducts was normal kidneys was in normal size and posture no evidence of hydronephrosis. Urinary bladder with regular wall with moderate urinary retention.
A small amount of free fluid in the pelvis and a 77 cm structure was demonstrated that causes a mass effect on the bladder refers to hematocolpos (Figure 1). The findings were verified by a gynecologist after testing with anesthesia and hematocolpos was diagnosed. The virginal membrane was opened using X-shaped diameters and there was a great outpouring of blood 700 cc. The girl was hemodynamically stable with no active bleeding and was discharged in a stable state, pain-free after two days of supervision.
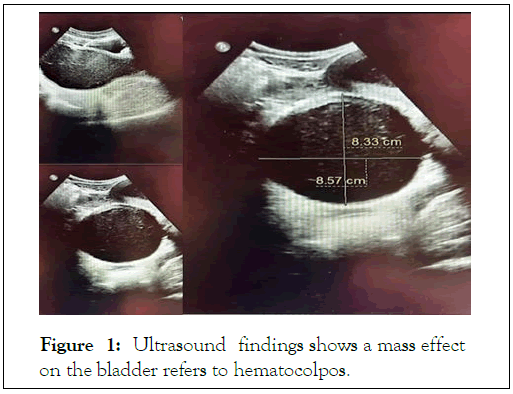
Figure 1: Ultrasound findings shows a mass effect on the bladder refers to hematocolpos.
The imperforate hymen is a clinical reality of undetermined etiology, being the most frequent cause of hydrometrocolpos. It's due to the absence of partial resorption of the hymenial membrane during the embryonic development and failure of it srupture in the perinatal period, the maturity being sporadically [1]. When family cases are reported, however, when they occur in isolation, no mutations or genetic markers were identified [2]. The American Society for Reproductive Medicine classifies mullerian anomalies into 6 groups based on the clinical presentation and prognosis treatment. This classification excludes extra uterine anomalies and although it allows additional descriptions of vaginal, tubal or urinary abnormalities [3], it becomes complex. In order to overcome this limitation the classification of the European Society of Human Reproduction and Embryology (ESHRE) and the European Society for Gynaecological Endoscopy (ESGE) was updated, allowing to classify this anomaly as U0C0V3 (U0-normal uterus, C0-normal cervix and V3-vagina with transverse septum/imperforate hymen) [4,5]. Described as one of the most frequent obstructive lesions of the vagina, the hymen should be evaluated at birth, at which time the new-born may have salient hymenial membrane due to the presence of mucocolpos. At this time, the adolescent may have a history of pelvic or cyclic abdominal pain and hematocolpos [6,7]. The distention caused by theretained catamenial blood may result in compression of the contiguous pelvic structures causing pain in the defecation, low back pain and urinary difficulty being rare, the occurrence of urinary retention. Presentation on the form of urinary retention is not frequent [8]. Treatment can be performed at the time of diagnosis, however it is considered that healing is optimized in tissue under estrogenic stimulation, thus reducing the risk of recurrence [9]. In the absence of complications and hymenial bulging, when the diagnosis is made in the prenatal period, it is recommended to delay the treatment until puberty, one year after the development of the mammary glands with hormonal environment favorable to healing.
CHI has been a known cause of persistent hypoglycemia during infancy due to dysregulated insulin secretion. GIR above 8 mg/kg/minute to maintain euglycemia is typical of this condition. In infants with HH diazoxide, unresponsiveness is an absolute indication for performing genetic studies as reported in our case. Appropriate investigation for intermediary metabolite like serum insulin, cortisol, growth hormone, ketone bodies, Fundus Fluorescein Angiography (FFA), amino acids, lactate, ammonia, bicarbonate, and blood gas analysis are considered as cornerstone for diagnosis and management of Hereditary Hemochromatosis (HH). Screening for genetic mutation ( KCNJ11 & ABCC8 ) and F-DOPA PET scan to rule out congenital causes and insulin secreting tumors has streamlined the management of CHI. Although there are many risk factors for hypoglycemia in neonates commonest were Small for Gestational Age (SGA) and macrosomic infants born to diabetic mother. Early diagnosis and aggressive management is considered highly essential to have better neurodevelopmental outcomes.
Citation: Nasser B, Jerdev M, Nasse H, Nasse W (2022) Hematocolpos-Incidence and Symptoms in Children: A Case Report. Pediatr Ther. 12:404.
Received: 28-Dec-2021, Manuscript No. PTCR-21-15269; Editor assigned: 31-Jan-2022, Pre QC No. PTCR-21-15269 (PQ); Reviewed: 11-Feb-2022, QC No. PTCR-21-15269; Revised: 18-Mar-2022, Manuscript No. PTCR-21-15269 (R); Published: 25-Dec-2021 , DOI: 10.35248/ 2161-0665.22.12.404
Copyright: © 2022 Nasser B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.