Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Case Report - (2021)Volume 11, Issue 9
Managing acute appendicitis during current COVID-19 pandemic is proving to be quite challenging. The gold standard treatment for acute appendicitis is appendectomy; however, exceptional situation related to COVID-19 has led us to reconsider medical treatment alone as an alternative in selected patients. We present a case of 10 years old boy, who was diagnosed with COVID-19 and acute appendicitis. This report illustrates the possible challenges of determining if COVID-19 is the cause of acute appendicitis or it is merely a co-incidence that a case of acute appendicitis got tested positive for COVID-19.
SARS-CoV-2 infection; Acute Appendicitis
Acute appendicitis has a lifetime prevalence of 7%. Appendectomy is the gold standard of care for patients with acute appendicitis, but many studies have evaluated conservative management for the same [1]. Non-operative treatment for acute appendicitis has obvious benefits, including the avoidance of risks associated with surgery, as well as the complications of anesthesia, infection and bleeding, the elimination of the long-term complications of abdominal surgery, such as bowel obstruction and chronic wound pain [2].
The compromised multi-organ functions due to COVID-19 and the cytokine storms that result in systemic inflammatory response syndrome (SIRS) and multiple organ dysfunctions eventually lead to death [3,4]. We present a case of successful conservative management of acute appendicitis in a COVID-19 patient to understand the disease in perspective of SARS-CoV-2 infection with emphasis on the challenges of such a choice and its role in selected cases.
A 10 year old boy presented with lower abdominal pain, fever, loss of appetite and nausea for one day. On examination, patient had tenderness on the right side of the abdomen. Abdominal sonogram done on day 2 of pain did not reveal any pathology. Patient got admitted and his pain kept worsening in spite of I.V. antibiotics. He started having diarrhea 3-4 times a day. In view of fever, RT PCR for SARS-CoV-2 was done which turned out to be positive, though patient did not have any respiratory symptoms (Figure 1).
Figure 1: X-ray chest showing normal study.
Blood investigations revealed WBC counts as 9.35x 103 / cuL with neutrophilia. Both ferritin (642ng/ml) and CRP were raised suggestive of active corona infection. On day 3, tenderness was still localized to right iliac fossa. Alvarado score was assessed to be 7/10 and CT scan abdomen revealed acute appendicitis with possibility of localized perforation and minimal collection in the paracolic gutters (Figure 2). It also revealed mild hepatosplenomegaly and mesenteric lymphadenopathy.
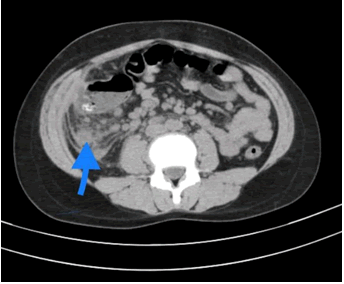
Figure 2: 1st CECT Abdomen showing sub hepatic collection.
In view of COVID-19 positive status and with great volume of data reporting multifold increase in morbidity and mortality in operated cases having SARS-CoV-2 infection, plan was devised to closely monitor the patient and put him on expectant management with inj Meropenem and inj vancomycin.
The patient had stable vitals and no signs of generalized peritonitis. Initial two days, there was not much change in the abdominal findings while general condition of the patient remained stable. On day 3, the patient was considered for surgical intervention in view of status quo with his abdominal examination still revealing localized tenderness in right iliac fossa, CECT abdomen was repeated (Figure 3). Decision was taken to continue the conservative management as CT showed decreased peri-appendiceal collection as compared to 1st scan.
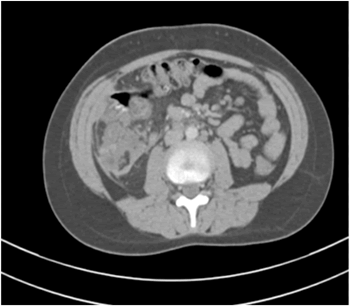
Figure 3: Follow up CECT Abdomen showing decreased RIF collection and inflamed appendix.
The patient also felt symptomatically better as fever subsided, pain decreased and appetite returned. He was put on oral medications and repeat COVID-19 test on day 14 came as negative. Patient was discharged on 14th day in stable condition with an advice to follow in surgery OPD.
Ever since novel corona virus disease (COVID- 19) has been declared pandemic by WHO, there are umpteen reports from all over the world with its varied presentations [5,6]. Patients with other diseases (acute or chronic) are becoming SARSCoV- 2 positive owing to community transmission or due to their exposure with health care workers while receiving treatment for their illness. The coronaviruses are a common source of upper respiratory, gastrointestinal, and central nervous system infections in humans. SARS-CoV-2 is highly homologous to SARS-CoV, and similar to SARS-CoV, angiotensin converting enzyme 2 (ACE2) is also the cellular entry receptor of SARSCoV- 2. In a recent Stanford study, fever, cough and shortness of breath were the classic symptoms of COVID-19, but there may be gastrointestinal symptoms, such as nausea and diarrhea. Gastrointestinal symptoms were reported by 31.9% of the patients. The majority of that group described the symptoms as mild. Twenty-two percent said they experienced loss of appetite, 22% had nausea and vomiting, and 12% had diarrhoea. This systematic review and meta-analysis of various studies found that approximately 12% of patients with SARS-CoV-2 infection reported gastrointestinal symptoms, including diarrhoea, nausea, and vomiting [7-8]. Since ACE2 is found in the absorptive enterocytes of the ileum and colon, these absorptive enterocytes can be infected by various viruses, including coronavirus, rotavirus, and noroviruses, thereby resulting in diarrhoea. ACE2- expressing intestinal epithelium cells might be at increased risk of attack by SARS-CoV-2 and that ACE2 was highly expressed in proximal and distal enterocytes present in small intestines. Hence, the small intestines can be invaded by SARS-CoV-2 and serve as a route of infection. In fact, the first reported patient with coronavirus disease 2019 (COVID-19) in the US reported gastrointestinal (GI) symptoms of loose bowel movements and abdominal discomfort.
Diagnosing acute appendicitis in corona positive patient is very complicated. There are a good number of patients who present like appendicitis without radiological evidence of inflamed appendix. This presentation is labelled as appendicular syndrome. It is indeed a dilemma to know for sure that pathology found in appendix is due to corona or it is purely co-incidence that appendicitis has developed in a corona positive individual. Obtaining RT-PCR on the stool samples of these patients could have been more informative but remained largely an academic exercise without influencing the management plan. While a lot of studies on gastro-intestinal presentation of corona infection show stool to be positive for SARS-CoV-2 by RT-PCR, this raises the question of inadvertent human to-human transmission via the faecal route despite public health emphasis on droplet transmission and precautions for contact with respiratory secretions. Presence of fecoliths leading to cause being deciphered as obstructive would have led us to not choose conservative management.
While the currently recommended treatment for uncomplicated acute appendicitis is surgical appendectomy, the non-surgical alternative of medical management by antibiotic therapy alone has been widely evaluated by high-quality studies in the literature. While decision for conservative management of patient in need for exploration was done, a very strict and close monitoring was instituted for development of features of peritonitis and worsening of corona related symptomatology [9,10]. Insofar as the limitations of exclusively medical treatment of uncomplicated acute appendicitis is the risk of recurrent appendicitis and failure of conservative management in terms of development of generalized peritonitis, sepsis and death, this treatment option represents an alternative of choice to reduce the intra-hospital overload in this context of health crisis.
Avoidance of surgery in these patients is important because it reduces the risk of exposing the operating room staff, particularly in case of inadvertent release of pneumoperitoneum during laparoscopy, or direct exposure of COVID positive peritoneal fluid. Moreover, post-operative mortality in COVID-19 positive patients seems to be higher than expected, even for elective surgery where morbidity is usually low. This is another reason why a non-surgical alternative is so important in patients with confirmed or suspected COVID-19 infection.
Appendectomy is the gold standard for management of appendicitis but novel corona virus infection has taught us a great deal to modify our practice to fit the new evolved scenario. From being a virus causing respiratory distress, SARS-CoV-2 is now emerging as one casing systemic infection causing myriad pathologies. The presentation of corona positive patients like acute appendicitis as well as corona infection complicating appendicitis has added to our experience in management of this pathology. By close monitoring of these patients and lessons learned from their recovery, we can conclude that corona infection causing appendicitis seems to be an entity that is emerging in these times. Giving such patients a chance to be managed conservatively is a win - win situation as it not only protects the corona infected patients by avoiding the complications that potentially increase multifold when they undergo any surgery but also prevents surgeon and other operation room staff getting exposed to the novel corona virus. There cannot be a very objective method to clearly know whether corona infection is the cause of acute appendicitis or patients presenting with acute appendicitis have coincidently COVID-19 infection in these pandemic times. Once this pandemic will end, getting a positive RT-PCR for corona in patients with acute appendicitis will only clear the picture.
Received: 01-Sep-2021 Accepted: 15-Sep-2021 Published: 22-Sep-2021 , DOI: 10.35248/2161-0665.21.11.396
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.