Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Research Article - (2019)Volume 9, Issue 1
Background: Neonatal sepsis is a systemic inflammatory response syndrome in the presence of or as a result of suspected or proven infection in a neonate. It is a leading cause of neonatal morbidity and mortality, particularly in developing countries. The clinical outcomes of neonatal sepsis vary in different hospitals with different setups.
Methods: Hospital-based prospective cross-sectional study was conducted on 306 neonates at the Neonatal Intensive Care Unit (NICU) of Wollega university teaching and Referral Hospital for two months from June 1 to August 30, 2018. The collected data was analyzed using SPSS version 20 windows. Tools like a review of secondary data, interview and observation were employed to collect the data
Results: Among 306 neonates included in this study, 133 (43.46%) were males and 92.5% had the weight of 2.5 kg-4 kg. Among the total study 306 neonates, 231 (75.5%) were diagnosed as early onset neonatal sepsis and 75 (24.5%) were diagnosed with late-onset neonatal sepsis. Majority of the patients, 294 (96.08%) were diagnosed with empirically and 96 (31.37%) neonates were born from mother with urinary tract infection during delivery. About two thirds (66.66%) of the neonates were delivered through the vagina and all neonates were administered the combination of ampicillin and gentamicin as a first line. Majority of the patients were admitted and stayed in the hospital for less than five days accounting 234 (76.48%). Majority of the patients with 276 (90.19%) were recovered and discharged. During the study period, a total of 12 (3.92%) mortality was recorded.
Conclusion: Empirical treatment was the mainstay for management of neonatal sepsis in this setup. Even though the majority of the neonates were improved and discharged, still there is a higher rate of death. Health policy makers should have to focus on the prevention of risk factors rather than treating the underline disease.
Neonatal sepsis; Pediatrics; Clinical outcome; Nekemte
CNS: Central Nervous System; EOS: Early Onset Sepsis; GP: General Practitioners; HIV: Human Immune Deficiency Virus; LBW: Low Birth Weight; LOS: Late Onset Sepsis; MoH: Ministry of Health (Ethiopia); NBW: Normal Birth Weight; NICU: Neonatal Intensive Care Units; NNS: Neonatal sepsis; UTI: Urinary Tract Infections; WBC: White Blood Cell; WHO: World Health Organization; WURTH: Wollega University Teaching and Referral Hospital
According to the international pediatric sepsis consensus conference of 2005, neonatal sepsis is defined as systemic inflammatory response syndrome in the presence of or as a result of suspected or proven infection in a neonate. Infection could be of bacterial, viral, fungal, or rickettsia origin [1]. Neonatal sepsis encompasses various systemic infections of the newborn, such as septicemia, meningitis, pneumonia, arthritis, osteomyelitis etc. [2,3]. Bacterial sepsis is considered to be an important cause of neonatal mortality (deaths) in the first month of life [4,5]. The world health organization estimated that there are approximately five million neonatal deaths per year of which 98% occur in developing countries [6,7]. The number of children dying from sepsis in the world has almost doubled in the past 20 years [8].
Neonatal sepsis may be classified according to the time of onset of the disease: Early Onset Sepsis (EOS) is (0-7 days) and Late-Onset Sepsis (LOS) is (8-28 days) [9,10]. The distinction has clinical relevance, as EOS disease is mainly due to bacteria acquired before and during delivery, and LOS disease to bacteria acquired after delivery (nosocomial or community sources) [11]. A few papers distinguish between very early onset sepsis (within 24 hours), EOS (24 hours to seven days), and LOS (more than seven days) sepsis [12,13].
The normal fetus is sterile until shortly before birth as the placenta and amniotic sac are highly effective barriers to infections. At birth, the newborn loses the protection afforded to it in the uterus and gets exposed to the microbial world [14]. Bacterial organisms causing neonatal sepsis may differ among countries, however, in most developing countries, Gram-negative bacteria remain the major source of infection [15,16]. Bacterial organisms causing neonatal sepsis have developed increased drug resistance to commonly used antibiotics, making its management a challenge for both the public and private health sectors [5,14]. This may be due to the fact that antimicrobial therapy in most developing countries is mainly empirical due to a relative lack of appropriate laboratory facilities for culture and sensitivity of bacteria in several health facilities [17].
The major causes of neonatal sepsis are disruption of amniotic membranes, infection upon passing through the birth canal, exposure to infected blood at delivery and trans-placental transmission of infection are some of the major causes of neonatal septicemia [18,19]. Neonatal conditions such as preterm, Low Birth Weight (LBW), male sex and twin gestation appear to be risk factors too [20,21]. Surviving infants can have significant neurological sequelae as a consequence of Central Nervous System (CNS) involvement, septic shock or hypoxemia secondary to severe parenchymal lung disease [22]. If diagnosed early and treated aggressively with antibiotics and good supportive care, it may be possible to save most cases of neonatal sepsis [6,23].
Neonatal sepsis is an important cause of morbidity and mortality among neonates in developing countries accounting for 30%-50% of total deaths each year [24]. In Ethiopia, previous studies showed that pneumonia, sepsis, meningitis were common causes of admissions and deaths in pediatrics hospitals [25,26]. The incidence of neonatal sepsis ranged from 4.2-11 per 100 live-born babies and the leading etiologic agents were gram-negative bacteria in the same hospital [27]. Neonatal mortality was very high when compared with the national data of Ethiopia [28]. Neonatal mortality was found to be 214 out of 4888 live births with a rate of 43.8 per 1000 live births [28].
The clinical outcomes of neonatal sepsis vary in different hospitals with different setups. Early diagnosis and treatment are required to save the life of our future generation [4,29]. This may require expertise to identify the common risk factors, the antimicrobial use pattern and the clinical outcomes of neonatal sepsis. Therefore, the study was aimed to fill the gap in knowledge about the risk factors, the antimicrobial use pattern and the clinical outcomes of neonatal sepsis.
Study area and study design
The study was conducted in Neonatal Intensive Care Unit (NICU) of Wollega university teaching and Referral Hospital (WUTRH) found in Oromia regional state, Nekemte town 331 km away from Addis Ababa, the capital of Ethiopia. The hospital has a total of 159 health care professional staffs and 96 supportive staffs. Neonatal Intensive Care Unit (NICU) was arranged under the pediatric ward as one department and contain 20 beds and 18 professional staff members. More than thousands of neonates admitted at NICUs annually to get medical services. A cross-sectional study was conducted at NICU of WUTRH for two months from June 1 to August 30, 2018.
Source population
All pediatric patients enrolled in WUTRH from June 1 to August 30, 2018.
Study population
All neonate patients who were admitted to NICU of WUTRH suspected or diagnosed for neonatal sepsis during the study period and fulfill the inclusion criteria.
Eligibility criteria
Inclusion criteria: All neonates with neonatal sepsis admitted to neonatal intensive care units during the study period from June 1 to August 30, 2018.
Exclusion criteria:
• Neonates discharged out of the study period
• Neonates who died without taking any treatment
• Neonates with incomplete patient chart information
Study variables
Dependent variables: Clinical outcome
Independent variables: age, sex, weight, diagnosis, type of sepsis, comorbid diseases, birth weight, gestational age, mode of delivery, mother condition: fever, urinary tract infections, and duration of labor.
Sample size determination and sampling technique
The sample size (n) was calculated by taking culture-proven neonatal sepsis approximately 23.9% in the previous study in Ethiopia [27]. The expected margin of error (w) was 0.05 and the confidence interval (zα/2) taken was 95%. Using the simple population proportion formula
P=An estimate of the proportion of outpatients with 23.9%
Z=the standard normal value at (1-q)% confidence level and is mostly 5% i.e. with 95% Confidence level
d=the margin of sample error tolerated=5%
n=(1.96)2 × 0.239(0.761)/(0.05)2=278
n=278
Contingency for the unknown circumstance (non-response rate) was taken to be 10%
278+278(10%)
n=306
Systematic random sampling was used to collect the necessary data.
Data collection tools and procedures
A semi-structured data collection format containing the variables to be measured was designed, developed and utilized by the principal investigator. Before starting actual data collection, small scale data collection was done on the questionnaires for having full required information of the study and to maintain the quality of the study. A random and detailed review of the medical charts of 306 neonates admitted at the neonatal intensive care units was made during the period of two months by using data collection checklist format prepared to accomplish this research. The data was collected until the patient was discharged or died. Data collection was done by two pharmacy internship students and one BSc nurse working in the neonatal intensive care unit of the Hospital. Different tools like a review of secondary data, interview and observation were employed to collect the data using developed semi-structured questionnaires.
Data processing and analysis
The collected data was analysed using SPSS version 20 windows. Once all necessary data was obtained, data were checked for completeness, sorted and categorized accordingly to the needed direction. Then the data were processed, analysed and interpreted inline of the objectives of the study. The final result was compared with the standard criteria and presented using tables, diagrams and various graphs.
Data quality assurance and management
Data quality was assured by careful selection and collection of complete and appropriate data. The clarity and completeness checkup of data collection formats was undertaken before the actual data collection. Data clearing to be done every day, formats with insufficient information were excluded from the study to avoid error. Then collected data was processed and retained cautiously in the line of its objective. A 5% sample pretest was performed on randomly selected patients before the beginning of the study.
Ethical consideration
Ethical clearance was obtained from the Wollega University, Institute of health sciences department of pharmacy. A formal letter was written from Department Pharmacy of Wollega University to WUTRH in order to get permission to conduct the study. Permission for any cooperation was politely asked the staff members of pediatric ward of the hospital. The confidentiality of patients was assured throughout by removing identifiers from data collection tools. The raw data was not made available to anyone and was not used as the determinant of any identity or subjects.
Socio-demographic characteristics of the patients
Among 306 study populations, 133 (43.46%) were males and 173 (56.54%) were females. Regarding maternal education more than half of the 162 (53.9%) attended secondary school followed by 72 (23.5%) college or above. Regarding the weight of the neonates, about 92.5% neonates had the weight of 2.5 kg-4 kg. The age of majority of the neonates 231 (75.5%) was below one week (Table 1).
| Variables | Frequency (n=306) | Percentage (%) | |
|---|---|---|---|
| Sex | Male | 133 | 43.46% |
| Female | 173 | 56.54% | |
| Age (weeks) | <1 | 231 | 75.50% |
| 1-2 | 54 | 17.6 | |
| 2-3 | 19 | 6.2 | |
| 3-4 | 2 | 0.65 | |
| Weight (kg) | <2.5 | 23 | 7.5 |
| 2.5-4 | 283 | 92.5 | |
| Maternal education | None | 24 | 7.8 |
| Primary school | 48 | 15.6 | |
| Secondary school | 162 | 53.9 | |
| College or above | 72 | 23.5 | |
Table 1: Socio-demographic distribution of neonates and maternal education with neonatal sepsis at NICUs, WUTRH, June 1 to August 30, 2018.
Type and mode of assessment of neonatal sepsis
Among the total study 306 neonates, 231 (75.5%) were diagnosed as EONS and 75 (24.5%) were diagnosed LONS. Majority of the patients, 294 (96.08%) were diagnosed empirically while 12 (3.92%) neonates were assessed kinetically or depend on lab result to be neonatal sepsis.
Maternal and neonatal factors related to neonatal sepsis
From the total of the mothers, 96 (31.37%) have Urinary Tract Infection (UTI) and 125 (40.8%) have high-grade fever during delivery. About two thirds (66.66%) of the neonates were delivered through the vagina and 210 (68.62%) neonates were delivered at the hospital. Majority of the mothers have a history of antenatal care with 276 (90.19%). Majority of the mothers have experienced duration of labour between 6-12 hours with 210 (58.33%) followed by 12-24 hours labour comprises 78 (25.49%) (Table 2).
| Variables | Frequency (n=306) | Percentage (%) | ||
|---|---|---|---|---|
| History of antenatal care | Yes | 276 | 90.19 | |
| No | 30 | 9.81 | ||
| Duration of labor | <6 hr | 7 | 2.28 | |
| 6-12 hr | 210 | 58.33 | ||
| 12-24 hr | 78 | 25.49 | ||
| >24 hr | 11 | 3.59 | ||
| Mothers condition during delivery | Fever | Yes | 125 | 40.8 |
| No | 181 | 59.15 | ||
| UTI | Yes | 96 | 31.37 | |
| No | 210 | 68.62 | ||
| Gestational age | Pre term (<37 wks) | 36 | 11.76 | |
| Term (37-42 wks) | 252 | 82.35 | ||
| Post-term (>42 wks) | 18 | 5.89 | ||
| Total | 306 | 100 | ||
| Mode of delivery | Vaginal | 202 | 66.66 | |
| Caesarian section | 76 | 25.4 | ||
| Instrumental | 24 | 7.84 | ||
| Place of delivery | Hospital | 210 | 68.62 | |
| Health center | 84 | 27.45 | ||
| Clinic | 6 | 1.96 | ||
| Home | 6 | 1.96 | ||
Table 2: Maternal and neonatal related factors associated with neonatal sepsis at NICUs, WUTRH, and June 1 to August 30, 2018.
Antimicrobial use pattern in neonates
All neonates were administered the combination of ampicillin and gentamicin as a first line. Majority of the patients received the combination of ampicillin and gentamycin for 3-5 days comprising 186 (60.78%) of the patients (Table 3).
| Antibiotics | Duration of treatment (days) | Total (%) | |||
|---|---|---|---|---|---|
| <3 days | 3-5 days | 5-10 days | >10 days | ||
| Gentamicin | 48 (15.68%) | 186 (60.78%) | 36 (11.76%) | 36 (11.76%) | 306 (100%) |
| Ampicillin | 48 (15.68%) | 186 (60.78%) | 36 (11.76%) | 36 (11.76%) | 306 (100%) |
| Cloxaciliin | 7 (23.3%) | 6 (20.0%) | 10 (33.3%) | 7 (23.3%) | 30 (9.8%) |
| Ceftriaxone | 11 (25.6%) | 13 (30.2%) | 14 (32.6%) | 5 (11.6%) | 43 (14.05%) |
| Vancomycin | 6 (25.0%) | 12 (50.0%) | 6 (25.0%) | - | 24 (7.84%) |
Table 3: Antibiotics prescribed for the treatment neonatal sepsis at NICUs, WUTRH, June 1 to August 30, 2018.
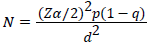
Co-administered drugs along with antibiotics
The most drugs co-administered along with antibiotics for neonatal sepsis was Paracetamol 120 mg suppository PRN comprising 96 (31.37%) followed by Tetracycline ophthalmic ointment with 48 (15.68%) (Figure 1).
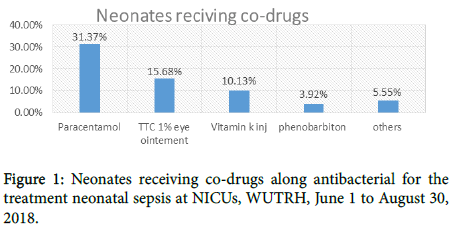
Figure 1: Neonates receiving co-drugs along antibacterial for the treatment neonatal sepsis at NICUs, WUTRH, June 1 to August 30, 2018.
Duration of hospital stay of the patients
Majority of the patients were admitted and stayed in the hospital for less than five days accounting 234 (76.48%) and 72 (23.52) stayed more than six days (Figure 2).
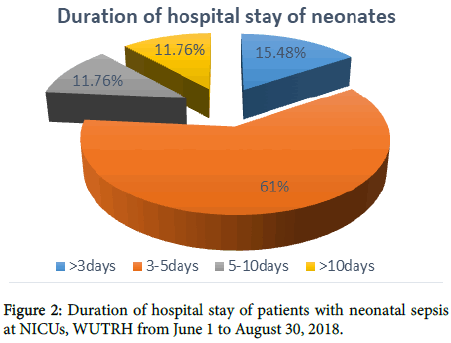
Figure 2. Duration of hospital stay of patients with neonatal sepsis at NICUs, WUTRH from June 1 to August 30, 2018.
Clinical outcomes of neonates
Regarding the outcomes majority of the patients (90.19%) were recovered from their condition with improvement followed by disability 12 (3.92%). A total of 12 (3.92%) mortality was recorded (Figure 3).
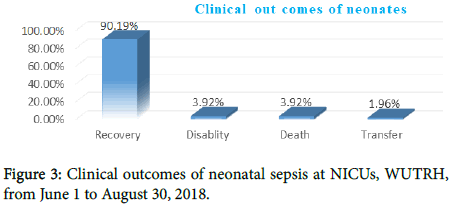
Figure 3: Clinical outcomes of neonatal sepsis at NICUs, WUTRH, from June 1 to August 30, 2018.
From the total 306 study population 173 (56.54%) neonates were females, which indicate female predominance in developing neonatal sepsis, which is in agreement with the study conducted in tertiary care hospital, India [30]. In this study, 231 (75.5%) and 75 (24.5%) neonates were presented with EOS and LOS respectively. The study showed that EOS was more common than LOS, which is in agreement with previous studies done in Ethiopia [10,26]. Infections in new-born often present with sepsis, with or without focal signs of infection. Focal signs and symptoms in neonates due to localized infections may be clinically imperceptible, and thus difficult to differentiate on an initial presentation from generalized or bloodstream infections [17,21,26]
The outcome of neonates with infections is strongly related to their appropriate diagnosis and management. Diagnosing neonatal infection, however, is a challenge, since clinical signs and symptoms are often nonspecific for a particular infection. As a consequence, deciding whether to treat or not, balancing optimal patients care with aspects such as possible adverse events or antibiotic resistance, may be difficult. Rapid, accurate detection of infected infants remains the most effective means of curbing sepsis-related mortality [12,19,23].
From the total of the mothers, 96 (31.37%) have UTI and 125 (40.8%) have high-grade fever during delivery. Neonates born from mother with UTI during delivery with neonates born from mother without UTI during delivery the probability of developing sepsis increase by in neonates born from mother with UTI during delivery [5,10]. Risk factors knowledge is important in reducing the incidence of neonatal sepsis [20,21,30]. Place of delivery, mode of delivery and mother with UTI during delivery were the most common risk factors for the incidence of neonatal sepsis [10].
Empirical treatment is the mainstay management of neonatal sepsis in most developing countries including Ethiopia. The antimicrobial use pattern in our hospital is mainly empirical. This may increase the development of resistant microbial, which in turn affect future drug selection in the management of neonatal sepsis. All neonates were treated by the combination of “ampicillin+gentamicin” and this result was in line with a number of studies as it was most common in empiric sepsis management [10,26].
Regarding the weight of the neonates about 7.5%, neonates had the weight of <2.5 kg. Newborn infants are especially vulnerable to nosocomial infections because of their intrinsic susceptibility to infection as well as the invasive procedures to which they are subjected. This is particularly high for those born prematurely or of LBW [10,24]. It is largely understood that prolonged rupture of membrane and prolonged labor are the commonly associated risk factors for the occurrence of neonatal sepsis because of the danger of ascending infection [5].
Finally, the outcome of neonates with infections is strongly related to their appropriate diagnosis and management. Diagnosing neonatal infection, however, is a challenge, since 12 (3.92%) died in the hospital. This result is in agreement with the study conducted in Tanzania [21] but in contrary with the study conducted in Nigeria [20]. The higher cases of neonatal mortality in our case could be attributed to the low health care utilization of women while there may be the difference in socio-cultural factors of the area [31]. Additional factors related to neonatal deaths in the present study were associated with small neonates birth size, birthplace, mother education, maternal illness, parity, ANC visit, and delivery without health professionals assistance.
Short surveillance time, a low number of proven infection and incomplete information about patient cards were some of the limitations of the study.
Empirical treatment was the mainstay for management of neonatal sepsis in this setup. Ampicillin and gentamicin combination was administered for all neonates with neonatal sepsis at NICU of WUTRH. Among the total neonate, 75.5% were diagnosed as EONS and the majority of the patients were admitted and stayed to the hospital less than five days. Majority of the patients with 90.19% were recovered and discharged.
Health policy makers should have to focus on the prevention of risk factors rather than treating the underline disease. Additionally, health policymakers should have focused on the expansion of neonatal intensive care unit to the lower facility like primary hospitals and health centers. Empirical regimens for neonatal sepsis must take into consideration the high rates of ampicillin and gentamicin resistance that are now prevalent. Thus, sensitivity testing should be performed.
The antimicrobial use guideline should be developed and updated timely by testing microbial sensitivity. The investigation of coexisting infections by a collection of other clinical samples in addition to blood sample is recommended to reduce the morbidity and mortality of neonates. The findings of the study indicate the need for further strengthening activities aimed at encouraging mothers for regularly attending ANC as well as for delivering their new-borns at health facilities, as these are key factors in reducing the neonatal morbidity and mortality.
We thanks Wollega University institute of health sciences for supporting this research. We would also like to thank the staffs of the NICUs in Wollega university teaching and Referral Hospital, without their cooperation this work would have never been accomplished, their cooperation had an effective role in facilitating this work.
Citation: Fekadu G, Abera T, Tekle T (2019) Clinical Treatment Outcomes of Neonatal Sepsis in Neonatal Intensive Care Unit of Wollega University Teaching and Referral Hospital, Nekemte Town, Western Ethiopia. Pediatr Ther 9:353.
Received: 31-Dec-2018 Accepted: 14-Jan-2019 Published: 18-Jan-2019
Copyright: © 2019 Fekadu G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.