Autism-Open Access
Open Access
ISSN: 2165-7890
ISSN: 2165-7890
Case Report - (2022)Volume 12, Issue 8
Autism Spectrum Disorder (ASD) is characterized by neurological, psychiatric and medical comorbidities, revealed in childhood, often including intellectual disability. Migraine is a very common neurological disorder, characterized by moderate to severe head pain. It is likely that experiencing severe migraine head pain might lead a young person with ASD to self-injurious behavior, such as striking or banging their heads. Botox for chronic migraine protocol is used to treat patients with frequent migraine episodes. While this protocol is off-label for persons under 18 years, it has been used with good efficacy to treat teenagers with chronic migraine and head pain. Two patients in our headache clinic population were identified as having ASD/intellectual disability, chronic migraine pain and self-injurious behavior. These patients underwent the Botox for chronic migraine protocol every 12 weeks, had significantly decreased migraine and head pain frequency, and subsequent reduction in self-injurious behavior.
Autism; Botox; Migraine; Pain; Self-injurious behavior
ASD: Autism Spectrum Disorder; IVH: Intraventricular Hemorrhage
Migraine is a very common neurological disorder, often starting in childhood/adolescence [1,2]. It can be an episodic disorder or a more difficult, chronic one, leading to significant disability [1]. The burden of chronic migraine in pediatrics falls on the child, the parents, and also on the educational system [3,4]. While there are a number of preventive medications used to reduce the migraine burden, these agents often are ineffective in treating the pediatric chronic migraine population [5].The side effects can interfere with mental functioning and cause other symptoms, and the medication may not be taken in a high enough dose to be effective at reducing migraine frequency and suffering [5-7].
Onabotulinumtoxin A is commonly used for the management of chronic migraine in adults [5]. It has been shown in clinical trials to be effective in reducing migraine frequency/headache days and duration [5]. The mechanism of action is thought to involve the inhibition of pain transmission, the inhibition of migraine-related neuropeptide release, and the direct inhibition of pronociceptive neurochemical release [5-7]. It is currently approved for the treatment of adults (over 18 years) with chronic migraine, defined as >15 headache days/month, pain lasting 4 hours or more, and ineffective trials of other preventive and treatment medications [5].
A number of patients in our Multidisciplinary Pediatric Headache Clinic have been identified as meeting the criteria for undergoing the Botox for chronic migraine treatment protocol. After receiving approval for insurance coverage of the procedure, these patients undergo the standard Botox protocol every 12 weeks, consisting of 155 units of Botox given IM in 31 sites in the face, head and neck areas. Most patients receiving this treatment are 18 year and above, but insurance approval has been obtained to use this treatment protocol for some of our appropriate patients who are less than 18 years old. For most of these patients, Botox has significantly reduced their migraine frequency, well tolerated with few side effects.
Autism Spectrum Disorder (ASD) is a complex neurological condition, affecting behavioral and developmental, as well as psychiatric and medical conditions [1-3]. There are numerous comorbidities associated with ASD, including neurodevelopmental disorders (intellectual disability, communication disorders, sensory perception disorders), common medical disorders (epilepsy, gastrointestinal disorders, sleep disorders) and psychiatric disorders (anxiety, depression, personality disorders) (Figure 1) [1-3]. Patients with ASD often have trouble expressing themselves and their experience of pain, which can manifest as self-injurious behavior. Although there are multiple different approaches to reducing self- injurious behavior in patients with other neurological disorders who experience pain, particularly Lesch-Nyhan syndrome [8- 10], Onabotulinumtoxin A has shown promise in reducing this behavior [11,12]. This agent has not yet been evaluated in patients with ASD who exhibit self-injurious behavior. ASD can affect just a few areas of life or multiple widespread areas of life, significantly impairing function.
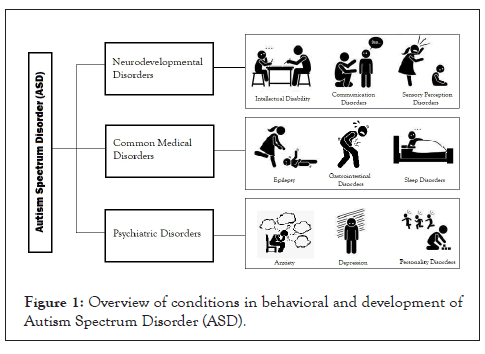
Figure 1: Overview of conditions in behavioral and development of Autism Spectrum Disorder (ASD).
Due to the prevalence of migraine in the general population, it is likely there are many people with ASD who also suffer from migraine, as both are common neurological conditions involving sensory processing impairment [1-3]. Both people with autism and people with migraine share an atypical sensory processing, hypersensitivity or hyposensitivity, related to chemical and anatomical alterations [1-3]. Both groups can share in general environmental sensitivities, such as sensitivity to sound, light, smells, and/or textures (tactile or oral) [1-3].
Two patients with autism/developmental delay, self-injurious behavior and chronic migraine with neuralgia in regular clinic follow up care, in the Multidisciplinary Pediatric Headache program, were identified as among those who might benefit from Botox for chronic migraine. Both patients had been treated with multiple medications which were not effective in managing their chronic headache. Both patients underwent the standard Botox for chronic migraine treatment protocol, every 12 weeks as specified by the protocol. They received 155u, given at 31 sites (5u/site). Results were identified by evaluating the frequency of severe headache and associated symptoms and behavioral observation.
Patient A
Past medical history: Patient A was born at 24 weeks via emergency c-section with prolapsed cord. He is a 25-year-old young male with developmental delay/ASD and a complex medical history, including shunted hydrocephalus related to Intraventricular Hemorrhage (IVH) with obstructive hydrocephalus, numerous shunt interventions, shunt infections, and thrombotic complications. He has a seizure disorder, spastic diplegia, optic nerve atrophy, SIADH and acquired immunodeficiency. He also has chronic migraine and occipital neuralgia. He experienced near-daily severe headaches, which caused nighttime awakening, photophobia, phonophobia and fatigue. He was also engaging in self-injurious behavior (hitting his head repeatedly, and angry outbursts). He has been treated with multiple medication trials to reduce the frequency of his chronic migraines and pain, without success. He is followed by numerous medical providers for his multiple health concerns.
Family history: Patient A lives at home with his adoptive mother, grandfather and brother and supported by home care nurses and patient care attendants.
Social history: Patient A is under guardianship of his adoptive mother, lives at home with family and community support. The family is working with the palliative care team for future life planning.
Physical examination: Patient A is alert, interactive, generally conversant and happy; on focused exam: HEENT/neurologic: shunt visualized beneath scalp and sensitive to touch; disconjugate gaze and afferent pupillary defect on the right, unable to upgaze or converge; mild right-sided facial weakness; left-sided weakness with increased motor tone L>R, hemiplegic gait.
Differential diagnosis: Patient A suffers from chronic migraine and presumptive neuralgia pain in the occiput and around his VP shunt.
Outcome: After undergoing 8 Botox for chronic migraine procedures to date-over the past 2 years, the frequency of headache and pain has reduced from 6 days/week to 1-2 times/month or less. He also demonstrates decreased associated symptoms, increased overall functioning and social engagement and decreased selfinjurious behavior. The improvement is maintained for nearly 12 weeks, starting to wane in the 2-3 weeks prior to the next treatment.
Patient B
Past medical history: Patient B was born at 37 weeks, no complications. She developed normally, until age 12 months, when she began a slow decline in social and developmental advancement, and lack of language skills. She was diagnosed with Autism spectrum disorder/pervasive developmental delay as a toddler and has been under supportive developmental care since then. She is now an 18-year-old young female, with a complex medical history including Chiari 1 malformation with cervical syrinx, surgically corrected in 2009; seizure disorder; sleep disturbance; chronic constipation, abdominal pain, GERD, and feeding difficulties. She has chronic migraine, atypical facial pain and cervicalgia, with pain accompanied by crying out, scratching and hitting the frontal region of the scalp. She has been treated with multiple medications to reduce his migraine frequency and pain. She is followed by numerous medical providers for her many health concerns.
Family history: Patient B lives at home with her parents and brother, with additional community and family supports.
Social history: Patient B is under the guardianship of her mother, lives at home with her family.
Physical examination: Patient B is alert, interactive; on focused exam: HEENT/neurological: full range of motion in her neck, increased tone in the trapezius ridge bilaterally; unable to converge, horizontal gaze intact; symmetric movement of extremities; Deep tendon reflexes are 2/4+ bilaterally.
Differential diagnosis: Patient B suffers from chronic migraine and chronic atypical facial pain/trigeminal neuralgia.
Outcome: Prior to treatment with Botox for chronic migraine protocol, B suffered from near-daily migraine pain, irritability and self-injurious behavior. She has undergone 13 Botox for chronic migraine every 12 weeks since 2017. Over time, her behavior and irritability have improved; she is free from irritability and self-injury for nearly 12 weeks, with symptom escalation in the 1-2 weeks prior to her next scheduled procedure.
The challenges of caring for a young person with ASD and developmental delays are well known and documented [1-3]. In addition to monitoring their physical health and well-being, there is the challenge of interpreting negative behaviors for causation, such as self-injurious behaviors [4,13]. Generally, it can take multiple visits with a variety of medical providers to determine what is happening, in conjunction with the insightful observation of their caregivers [8-15]. Then, once the cause of these negative behaviors is postulated, there can be numerous interventions to prevent/stop the behaviors. These will include many medications (assessing for effectiveness, dealing with side effects, ensuring medical compliance), possibly surgery, or procedures [8,9,12,15,16]. The challenges to the patient, family, educators and community supports, medical providers and the society at large cannot be overstated.
For patients with developmental challenges, effectively treating their pain can go far in improving the quality of life for them and for all those around them. The distress that is caused by untreated pain and their inability to really express what is happening is enormous [1-4]. Their frustration at not being understood and the pain itself drives them to self-injurious behaviors [4,10]. For these 2 patients, undergoing Botox for chronic migraine protocol relieved their headache pain, reduced significantly their self-injurious behaviors and their distress, without significant side effects.
Based on the results revealed from these 2 patients, using the Botox for chronic migraine protocol would be a reasonable intervention in patients with ASD/developmental delay with self-injurious behaviors, such as head banging, and probable migraine headache pain.
Botox for chronic migraine is known to reduce chronic migraine episodes in many patients by at least 50%. Less is known about the effect it has in the population of young people with developmental delay. Self-report is difficult and unreliable and often headache pain episodes are identified by observation of behavioral changes and irritability. Our experience with these 2 patients suggests that suffering from chronic headache and pain led to an increase in self-injurious behavior. A reduction in headache pain significantly reduced these behaviors, an unexpected benefit, and decreased the distress felt by the patient and their caregivers. Using Botox for chronic migraine may be a useful intervention for those patients who did not respond to the usual medical management of chronic headache and behavioral challenges.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Karian V, Chang CYH, Schefter ZJ, Lebel A (2022) Can Botox Reduce Self-Injurious Behavior in Young Patients with Chronic Head Pain and Autism/Developmental Delay? Autism Open Access. 12:333.
Received: 27-Jul-2022, Manuscript No. AUO-22-18577; Editor assigned: 01-Aug-2022, Pre QC No. AUO-22-18577 (PQ); Reviewed: 15-Aug-2022, QC No. AUO-22-18577; Revised: 19-Sep-2022, Manuscript No. AUO-22-18577 (R); Published: 26-Sep-2022 , DOI: 10.35248/2165-7890.22.12.333
Copyright: © 2022 Karian V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.