Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Research Article - (2017) Volume 7, Issue 2
Introduction: Acute Gastroenteritis (AGE) is a leading cause of illness and death amongst children in developing countries. Electrolyte disturbances play an important role in the associated morbidity and mortality. Aims and objectives: (1) To study the electrolyte changes in moderate and severe dehydration in AGE in children. (2) To study the incidence and clinical features of Hyponatremic dehydration. Materials and methods: A cross-sectional type of observational study of 200 children admitted with AGE with moderate to severe dehydration was conducted at M R Bangur hospital, Kolkata. The cases were divided into two groups, one with Hyponatremia and the other with Isonatremia and the clinical features were compared. Basic crosstabulation and frequency distributions were prepared. Chi-square test and Fisher's Exact test were used to test the association between different variables. Z-test and t-test were used to test the significant differences. P ≤ 0.05 was considered statistically significant. Results: AGE constituted 18% of the total admissions. 22% had Hyponatremia, 71.5% had Isonatremia and 6.5% had Hypernatremia. Out of 30 children who were suffering from Hyponatremic dehydration and had ORS before admission, 83.3% were given diluted ORS. Clinical features significantly associated with Hyponatremia were increased frequency of diarrhea, absence of thirst, tachycardia, abdominal distension and severe dehydration. Conclusion: Hyponatremic dehydration is the second most common type of dehydration next to Isonatremic dehydration, but it is more common in children who took diluted ORS. Hyponatremic dehydration may be suspected from the history and clinical features. Increased awareness regarding ORS preparation may help in preventing Hyponatremia in AGE. What is already known: Isonatremic dehydration is the most common electrolyte abnormality found in AGE. What this study adds: Hyponatremic dehydration is the most common electrolyte abnormality found in those suffering from AGE, who have taken inappropriately diluted Oral Rehydration Solution (ORS).
Keywords: Acute gastroenteritis, Oral rehydration solution, Diarrhea
Diarrhea is a leading cause of illness and death in children of developing countries, where an estimated 1300 million episodes and 3.2 million deaths occur in under-5 children. About 80% of deaths due to diarrhea occur in the first 2 years of life [1]. WHO estimated that worldwide, 1 child dies of diarrhea every 6 seconds [2]. In India, at least 1.5 million under-5 children die every year due to acute diarrhea [3].
The high incidence of diarrheal diseases in developing countries is related to under-nutrition, increased vulnerability to infections, poor education, socio-economic status and the unfortunate trend of early breast milk substitutes. Decreasing trend of exclusive breast feeding and faulty practices of bottle-feeding play an important role. The main cause of death in acute diarrhea is dehydration, which results from the loss of fluid and electrolytes in diarrheal stools.
The clinical manifestations of acute diarrhea are related to the severity of water deficit and the type of electrolyte disturbances. Often laboratory facilities are not available or, even if available, there is a considerable time lag in obtaining the results. Consequently, clinical recognition of water and electrolyte disturbances becomes important, particularly Hyponatremic dehydration, due to its serious neurological consequences.
A study conducted in 2010 in Dhaka Shishu hospital showed that electrolyte disturbances in AGE was associated with increased morbidity, with hyponatremic dehydration in 15% cases [4].
No recent studies exist regarding the electrolyte disturbances occurring in a child suffering from AGE. Also, there are no specific studies describing the clinical features associated with Hyponatremic dehydration, and the clues to differentiating it from Isonatremic dehydration.
In the present study, an attempt has been made to outline the spectrum of electrolyte disturbances in children suffering from AGE with moderate to severe dehydration and to correlate those parameters with clinical status.
This was a Hospital based cross-sectional type of observational study located at M R Bangur Hospital, Kolkata. 200 Children admitted in the Pediatrics ward of M R Bangur Hospital, suffering from AGE, were studied.
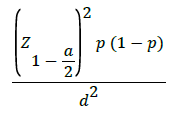
The power of the study is 80%, 5% probability of Type I error with significance level at p<0.05. Sample size was calculated by the following formula:
Inclusion criteria
1. Passage of watery stools 3 or more times per day (including dysentery).
2. Duration of illness less than 2 weeks at the time of admission.
3. Age group <10 years (excluding neonates).
4. Signs suggestive of moderate to severe dehydration.
Exclusion criteria
1. Signs suggestive of no/mild dehydration.
2. Persistent diarrhea (>2 weeks).
3. Other cause of dehydration.
The number of children admitted with AGE during the period of study was 657.18% of the total admissions. 200 patients were randomly selected. Detailed history, examination and investigations were recorded in specially designed Proforma. A note of ORS intake before coming to the hospital was also made. Preparation of the ORS was asked in detail.
Written informed consent was taken from the parent/caretaker prior to the study. Ethical approval for the study was taken from our regional ethical committee.
Before starting any rehydration measures, 2 ml of blood was drawn to estimate the serum electrolyte levels.
Statistical Analysis was performed with help of Epi Info (TM) 3.5.3 which is a trademark of the Centers for Disease Control and Prevention (CDC).
Using this software, basic cross-tabulation and frequency distributions were prepared. Chi-square test was used to test the association between different study variables. Corrected Chi-square test was used in case any one of cell frequency was found less than 5 in the bivariate frequency distribution. Fisher’s Exact Test was used where Chi-square test could not be applied.
Test of proportion (Z-test) was used to test the significant difference between two proportions. t-test was used to test the significant difference between means. p ≤ 0.05 was considered statistically significant.
166 cases (83%) had moderate dehydration whereas 34 cases (17%) had severe dehydration.
22% (44) cases were found to be having Hyponatremic dehydration. 71.5% (143) cases had Isonatremia.
Increased frequency of diarrhea, absence of thirst, abdominal distension, tachycardia and altered sensorium were found to be associated with Hyponatremia.
Out of the 59 patients who were given ORS before admission, most of them (52.5%) were given diluted ORS (Z=2.40; p=0.016) (Table 1).
| Type of ORS before admission | Number | % |
|---|---|---|
| Appropriate | 21 | 35.6 |
| Concentrated | 7 | 11.9 |
| Diluted | 31 | 52.5 |
| Total | 59 | 100.0 |
Table 1: Type of ORS taken before admission (n=59).
Inappropriately diluted ORS consumption appeared to be significantly associated with Hyponatremia (p=0.026) (Figure 1).
Type of ORS taken before admission was plotted against the percentage of children suffering from electrolyte imbalance. Hypernatremia was more prevalent for the patients who were given concentrated ORS before admission (100%) and Hyponatremia was more prevalent for the patients who were given diluted ORS before admission (83.3%). In both cases it was significantly higher (p=0.000001).
Corrected Chi-square (χ2=4.68) test showed that there was significant association between type of ORS taken before admission and Hyponatremia (p=0.026).
Isonatremic dehydration was most common. But, Hyponatremia was more commonly found in children who have had diluted ORS solution.
Hypokalemia was present in 15% (30) cases and 85% (170) cases had Normokalemia.
Average duration of hospital stay in AGE with Hyponatremic dehydration was 5.52 days which is more than those with Isonatremia (3.46 days).
AGE continues to be a common cause of mortality in infants and pre-school children throughout the developing world. The incidence of AGE has varied in different areas of India among hospitalised cases. Srivastava et al. [5] Behera et al. [6] and Ahmed et al. [7] reported an incidence of 12.3%, 11.3% and 14.2% respectively. In the present study, AGE was 18% forming the second largest group of inpatient admissions.
Age distribution
In the present study, AGE with moderate to severe dehydration was almost equal in the 1-5 yrs and >5 yrs age group (44% and 44.5% respectively). 11.5% of the cases were infants. This result differs from those found in studies conducted by Srivastava et al. [5] and Behera et al. [6] which report a higher incidence of AGE in Infants. The difference may be accounted for by the fact that those with mild or no dehydration were not taken into account. There was no significant association between age of the child and type of electrolyte abnormality.
Sex distribution
AGE was more common in boys than girls with the ratio of 1.2:1, a finding which is similar to that reported by Srivastava et al. [5] and Behera et al. [6]. The type of dehydration had no significant association with gender.
Socio-economic status
Most of the children (36%) belonged to Class III Socio-economic group of Modified B J Prasad’s classification [8]. Only 5.5% belonged to Class V Socio-economic group, which is in accordance with the fact that the study was conducted in an urban setting.
ORS intake before admission
Most of the children (70.5%) were not given ORS before admission. Out of the 59 patients who were given ORS before admission, most of them (52.5%) were given diluted ORS before admission. 35.6% were given appropriate ORS before admission. 11.9% were given concentrated ORS. There was significant association between ORS intake and Hyponatremia. Out of 59 children who were given ORS before admission, 30 (68.2%) children had Hyponatremia.
The type of ORS taken was significantly associated with Hyponatremia (p=0.026). Out of 30 children who were suffering from Hyponatremic dehydration and had ORS before admission, 25 (83.3%) were given diluted ORS. All 7 children who had ORS prior to admission and suffered from Hypernatremic dehydration, had concentrated ORS.
Among the 21 children who had appropriate ORS before admission, only 5 had Hyponatremia and none of them had Hypernatremia. Thus, concentration of home-prepared ORS had an important role to play in the electrolyte disturbances occurring in AGE. Diluted ORS often lead to Hyponatremia.
Degree of dehydration
Dehydration is a common clinical feature of AGE in children. 83% (166) of the children had moderate degree of dehydration and 34 children had severe dehydration. Mittal et al. [9] has reported 50.52% of moderate dehydration and 21.95% severe dehydration in their study.
In the present study, Hyponatremia was seen in 35.3% of severely dehydrated and 19.3% of moderately dehydrated group.
Distribution of the level of electrolytes
In the present study, Isonatremic dehydration was the commonest (71.5%), followed by Hyponatremic dehydration (22%) and Hypernatremic dehydration (6.5%). Krishnan et al. [10] and Samadi et al. [11] reported the incidence of Hyponatremic dehydration as 25.3% and 20.8% respectively (Table 2).
| Type of dehydration | Santhana Krishnan | Samadi A.R. | Present Study |
|---|---|---|---|
| Isonatremia | 59.3% | 72.8% | 71.5% |
| Hyponatremia | 25.3% | 20.8% | 22% |
| Hypernatremia | 15.4% | 6.4% | 6.5% |
Table 2: Comparison of types of dehydration in various studies.
In the present study, 170 children (85%) had Normokalemia and 30 cases (15%) had Hypokalemia and none of the cases had hyperkalemia. 6 cases of hyponatremia had associated hypokalemia.
In the present study, 173 children (86.5%) had Normochloremia, 25 (12.5%) had Hypochloremia and 2 (1%) had Hyperchloremia. Out of the 25 cases of Hypochloremia, 8 had associated Hyponatremia and 21 children had associated Hypokalemia as well. Purohit noted Hypochloremia in 59% of his cases and he attributed the higher incidence to associated vomiting [12].
Associated symptoms and signs
Loose stool: All children enrolled in the study had presented with complaints of loose stool. Average duration was 2.5 days, ranging from 12 hrs to 6 days. Frequency ranged from 3 to 20 times per day, with average frequency of 9.72 times per day.
Vomiting: 44 (22%) children had associated vomiting. Average duration of vomiting before admission to the hospital was 1.68 days (40.42 hrs) ranging from 12 hours to 4 days. Frequency of vomiting ranged from 2 to 12 times per day with an average of 4.76 times per day. Out of 44 children who had vomiting, 13 cases (29.5%) suffered from Hyponatremia.
Thirst: Increased demand or acceptance by the child as told by the mother was seen in 119 cases (59.5%). 25 out of 44 cases with Hyponatremia had increased thirst (56.8%) whereas 94 out of 143 cases (60.3%) with Isonatremia had increased thirst.
Fever: In the present study, 54% (108) cases had fever. Srivastava et al. [5] reported fever in 40% cases. 56.4% (88/143) with Isonatremia and 54.5% (20/44) with Hyponatremia had fever as a symptom.
Abdominal distension: 22% (44) cases had associated abdominal distension. 81.8% (36/44) of Hyponatremic children had distension of abdomen. 5.1% (8/143) of Isonatremic children had distension of abdomen. Most of the children having Hyponatremia also had associated hypokalemia, which may lead to abdominal distension.
Convulsion: 25% (2) children had convulsion. 2.4% (1/44) of hyponatremic children had history of convulsion. The child had a prolonged duration of stay (8 days). 12.5% (1/13) of Hypernatremic children had convulsion. This child was also having severe dehydration and severe electrolyte disturbance and succumbed within 3 days of admission. None of the cases with Isonatremia had history of convulsion. Caksen et al. [13] reported the incidence of convulsions in 15.3% of patients with hyponatremic dehydration.
Muscle cramps: Out of 200 children, 169 cases were unable to indicate the presence of cramps. Out of 31 cases who were able to indicate the presence of cramps, 12 of them complained of cramps.
Tachycardia: 61% (122) children had tachycardia. 51% (73/143) cases with Isonatremia had tachycardia, whereas 93% (41/44) cases with Hyponatremia had tachycardia.
Tachypnea: 4.19% (6/143) cases without Isonatremia had tachypnea, whereas 22% (10/44) cases with hyponatremia had tachypnea.
Level of sensorium: In the present study, 73.5% (147) children suffering from AGE were alert. Level of consciousness/sensorium was affected in 88.6% (39/44) Hyponatremic cases. 19 were lethargic, 4 were irritable and 1 child was comatose. Whereas AGE with Isonatremia had 135 children (94.4%) who were alert, 4 (2.8%) were irritable, 4 (2.8%) were lethargic. 5 children who were alert had Hyponatremia.
Duration of hospital stay: The mean duration of hospital stay of the patients was 4 days with a range of 2 to 8 days. 75% (9/12) of those with duration of stay >7 days, suffered from Hyponatremia.
Case fatality rate in the present study was 0.005%. The only child who succumbed was a 1 year 6 months old girl who had convulsions, hypernatremia and was severely dehydrated. The child died after 3 days of hospital stay.
The most common electrolyte disturbances associated with AGE with dehydration were Hyponatremia and Hypokalemia. Isonatremic dehydration was the commonest type followed by Hyponatremia. Hyponatremic dehydration may be suspected from history taking and clinical features and can be readily diagnosed by laboratory studies. It is associated with significant morbidity and increased duration of hospital stay. Diluted ORS administration prior to admission appears to play a significant role in the causation of Hyponatremic dehydration (p=0.026).
The clinical impression of the type of dehydration and electrolyte disturbances was fairly consistent with serum electrolyte values. Abdominal distension had a positive correlation with Hyponatremia and Hypokalemia. Routine estimation of serum electrolytes is not necessary. However, it is essential whenever electrolyte imbalance is suspected on clinical grounds and in cases which do not respond satisfactorily with routine fluid and electrolyte therapy.
Promotion of health awareness, breastfeeding, weaning with hygienically prepared foods, demonstration of how to prepare appropriate ORS solution, better female literacy and health education will go a long way in reducing the morbidity and mortality associated with AGE.
The present study was based on a small sample size. A larger study group is recommended to come to a very definite conclusion.