Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 5
Aim: To report on the impact of Dry Eye Disease (DED) on social, mental, and financial well-being, and the use of virtual consultations to assess DED during the covid-19 pandemic.
Materials and methods: An exploratory retrospective review of 35 charts. Telephone consultations for patients with DED conducted during the first lock-down period in Ontario in 2020 were reviewed.
Results: The most commonly reported DED symptoms were ocular dryness, visual disturbances, and burning sensation. The most common dry eye management practices were artificial tears, warm compresses, and omega-3 supplements. 20.0% of charts documented worsening of DED symptoms since the onset of the pandemic and 17.1% reported the lockdown had negatively affected their ability to perform DED management practices. 42.8% of patients reported an inability to enjoy their daily activities due to DED symptoms. 52.0% reported feeling either depressed, anxious, or both with 26.9% of patients accepting a referral to a social worker for counselling support. More than a quarter of the charts recorded financial challenges associated with the cost of therapy, and more than a fifth of patients reported that financial challenges were a direct barrier to accessing therapy.
Conclusion: Patients living with DED reported that their symptoms negatively affected their daily activities including mental health and financial challenges that in turn impacted treatment practices. These challenges may have been exacerbated during the COVID-19 pandemic. Telephone consultations may be an effective modality to assess DED symptom severity, the impact of symptoms on daily functioning, and the need for counselling and support.
Dry eye disease; COVID-19; Virtual care; Quality of life; Patient adherence
Dry Eye Disease (DED) is a multifactorial disease of the ocular surface characterized by loss of homeostasis of the tear film. Tear film instability and hyperosmolarity leads to ocular surface inflammation and damage [1], resulting in symptoms including burning and gritty sensation, photophobia, foreign body sensation, excess tearing, visual disturbances, and difficulty performing visual tasks [2]. DED is a chronic and incurable disease, affecting an estimated six million Canadian adults [3]. DED is known to negatively affect quality of life, work productivity [4], sleep [5], emotional well-being [2,6,7] and other everyday activities [8]. Moreover, the negative impact of DED on daily living has been associated with mental health challenges such as depression and anxiety [9].
The COVID-19 pandemic has affected access to healthcare in Canada with devastating effects on healthcare systems globally. Canada’s pre-existing health care system was challenged with lengthy wait times [10] prior to the pandemic. Long wait times have been further exacerbated by the COVID-19 pandemic when lockdown periods resulted in cancelled or postponed appointments and delays in delivering care. In 2020, national wait times were longest for referral to ophthalmology compared to any other specialist referral with an average wait of 34.1 weeks [11].
Since the onset of the COVID-19 pandemic, many physicians have turned to virtual appointments as a solution in which physicians meet with patients via telemedicine modalities including phone and video chat. In Canada, virtual health care visits with primary care physicians and specialists jumped from 4% to 60% at the onset of the COVID-19 pandemic [10]. There is existing literature presenting the use of virtual care for ophthalmic conditions such as glaucoma [12,13]. During the Ontario COVID-19 lockdown period starting March 2020, nonurgent patient visits to the clinic were cancelled.
The objectives of this study are as follows: To report on
1) The impact of DED on patients’ social, mental, and financial well-being during the COVID-19 pandemic and,
2) The experience of using virtual consultations to assess patients with DED during the COVID-19 pandemic.
Study design
A retrospective chart-review study was conducted from one cornea specialist practice at the Ivey Eye Institute (IEI), Schulich School of Medicine, Western University, London, Ontario, Canada. All data from patient charts were fully anonymized before they were accessed for use in the study, and authors did not have access to information that could identify individual participants during or after data collection. Charts were reviewed from August 1, 2020 to September 31, 2020. Patients had been referred by their optometrist or ophthalmologist for evaluation of dry eye disease. Only patients with adequate Visual Acuity (VA>20/30) and normal Intraocular Pressure (IOP<22 mmHg), as documented by referring eye care providers, were selected for virtual consultations.
Consultations were provided virtually over the phone using a structured questionnaire based on questions routinely asked in-person, and using validated questionnaires that are typically self-administered by patients during in-person consultations. The virtual consultation was divided into two parts; the first part was administered by a clinical assistant to obtain medical and ocular histories, document symptoms, current treatment, and Canadian Dry Eye Assessment (CDEA) and Dry Eye Questionnaire-5 (DEQ-5) scores in the same way that an ophthalmic technician would gather this information in a clinic setting. The second part of the DED consultation was conducted by telephone with the cornea specialist.
In light of the many disruptions to daily routines during the lockdown period, such as increased screen time from working from home, patients were asked whether their DED symptoms had changed during the lockdown and whether the lockdown was affecting their ability to engage in DED self-care.
Patient population
All patients were referred by a physician or optometrist with an established diagnosis of DED. Patients were selected for virtual care appointments based on normal intraocular pressure and visual acuity, as reported by the referring physician or optometrist or ophthalmologist. A total of 35 patients had a virtual appointment booked. Six patients attended only the first part of the consultation. The data from first part of the consultation were included in the chart review.
Data analysis
Results are presented as a percentage of total responses collected for each question, as well as mean values of total responses. Dry Eye Disease Management score (DEDM) is a composite score created to capture overall DED management practices using five indicators: use of artificial tears, use of tear gel, use of omega-3 supplements, use of warm compresses to the eyes, and use of eyelid cleansing. DEDM scores were tabulated by adding one point for each of the practices, leading to a scale from 0 to 5, where 5 indicates using all five management practices and 0 indicates using none the management practices. Spearman’s Rho tests were used to compare percentage values. Jeffrey’s Amazing Statistics Program (JASP) (v0.14.1) was used to conduct statistical analysis and results were considered statistically significant if P<0.05.
Participant demographics
All charts (n=35) recorded age, sex, general health history, including previously diagnosed sjorgren’s syndrome, co-morbidities and systemic medications. All charts also documented ocular health history, dry eye history, ocular topical medications and other DED treatments, and frequency of optometric care. A total 35 patients completed the first part of the consultation interview with the clinical assistant. While not all patients answered every question, all completed questions were analyzed in the chart review as a proportion of those that did answer the question. On average, patients reported experiencing DED symptoms for 6.14 years prior to ophthalmology consultation and visiting their optometrist 1.61 times per year regarding DED are shown in Table 1. A fifth of charts documented patients with a pre-existing diagnosis of sjogren’s syndrome. 78.13% of charts documented a DEQ-5 score equal to or greater than 12, suggesting sjogren’s related DED and warranting further work-up. 21.21% of charts documented severe DED symptoms and 48.48% had moderate DED symptoms according to CDEA scores equal to or greater than 31 (Table 1).
| Participant demographics | N | % or Mean |
|---|---|---|
| Total participants | 35 | |
| Years living with DED symptoms (mean) | 6.14 years | |
| Visits to doctor for DED complaints yearly | 35 | |
| Mean | 1.61 ± 1.37 | |
| More than once per year | 14 | 40.00% |
| Previous sjogren’s diagnosis | 35 | |
| Yes | 7 | 20% |
| No | 28 | 80% |
| Dry Eye Questionnaire (DEQ-5) Score | 32 | |
| Mean | 13.875 | |
| Sjogren’s (DEQ-5>12) | 25 | 78.13% |
| Canadian Dry Eye Assessment (CDEA) Score | 33 | |
| Mean | 23.7 | |
| Mild (CDEA 5-20) | 10 | 30.30% |
| Moderate (CDEA 21-30) | 16 | 48.48% |
| Severe (CDEA 31-48) | 7 | 21.21% |
Table 1: Participants demographics with DED symptoms before and after consultation of optometrist.
DED symptoms and management practices
The three most bothersome DED symptoms were documented for each patient. Results are shown in Figure 1. The worst symptoms experienced were ocular dryness (37.14%), blurred/fluctuating vision (20.00%), and burning/stinging (14.29%) (Figures 1a-1c).
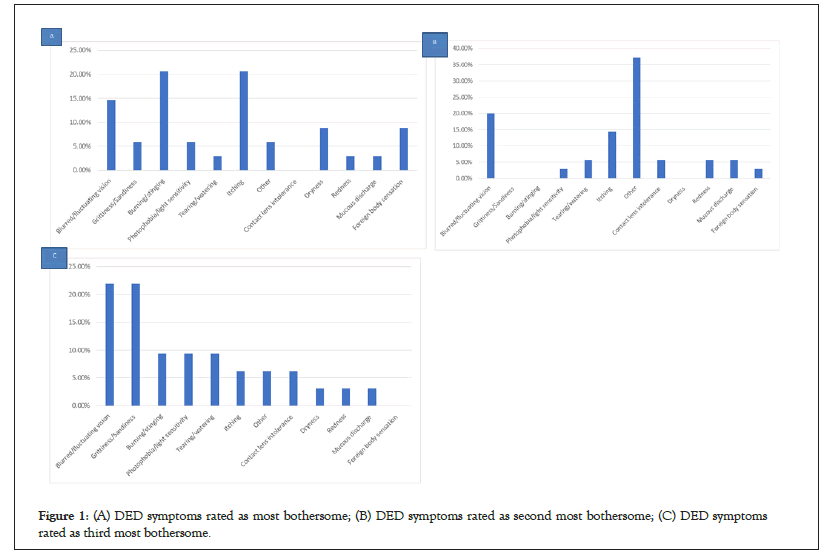
Figure 1: (A) DED symptoms rated as most bothersome; (B) DED symptoms rated as second most bothersome; (C) DED symptoms rated as third most bothersome.
The most common management practices among patients were artificial tear use (82.86%), warm compresses (71.43%), and omega-3 supplements (42.86%) are shown in Table 2. However, among artificial tear users, 52.17% of charts documented the reported use to be less than three times per day. Among omega-3 users, 30.77% of charts documented taking less than the recommended daily dose of 2000 mg (Table 2).
| DED management practices | N | % or Mean |
|---|---|---|
| Artificial tears | 35 | 82.86% |
| Tear gel or ointment | 35 | 34.29% |
| Eyelid cleansing daily | 35 | 31.43% |
| Warm compresses | 35 | 71.43% |
| Omega-3 supplements | 35 | 42.86% |
| Mean amount taken per day (mg) | 2215.71 mg ± 1001.41 | |
| % of patients taking omega-3 who take less than the | 30.77% | |
| Recommended daily dose (<2000 mg) | ||
| Most common usage frequency of artificial tears (per day) | 29 | |
| 3 times | 7 | 24.14% |
| 2 times | 5 | 17.24% |
| Occasional | 4 | 13.79% |
| Most common brands of artificial tears used | 29 | |
| Systane | 16 | 55.17% |
| Refresh | 5 | 17.24% |
| Other | 5 | 17.24% |
| Most common brands of ointment or gel used | 11 | |
| Systane | 5 | 45.46% |
| Ocunox | 2 | 18.18% |
| Other | 2 | 18.18% |
Table 2: Most common DED management practices among patients.
Spearman’s Rho analysis revealed that there was no significant correlation between DEDM scores and DEQ-5 scores are shown in Table 3. However, there were significant correlations between number of artificial tears used per day and DEQ-5 score (P=0.009), between number of artificial tears per day and DEDM scores (P<0.001), and between number of artificial tears used per day and number of visits to eyecare provider per year (P=0.008) (Table 3).
| Variables | CDEA Score | DEQ-5 Score | DEDM Score | Number Of Visits Per Year | Years with Symptoms | Number of Artificial Tears Per Day |
|---|---|---|---|---|---|---|
| CDEA Score | - | - | - | - | - | - |
| DEQ-5 Score | Rho=0.527 | - | - | - | - | - |
| p=0.002* | ||||||
| DEDM Score | Rho=0.192 | Rho=0.320 | - | - | - | - |
| p=0.285 | p=0.070 | |||||
| Number of Visits Per Year | Rho= 0.176 | Rho= 0.122 | Rho= 0.221 | - | - | - |
| p=0.327 | p= 0.499 | p= 0.217 | - | |||
| Years with Symptoms | Rho= 0.245 | Rho= 0.350 | Rho= 0.173 | Rho= -0.076 | - | - |
| p= 0.170 | p= 0.046 | p= 0.335 | p= 0.673 | - | - | |
| Number of Artificial Tears Per Day | Rho= 0.183 | Rho= 0.449 | Rho= 0.704 | Rho= 0.453 | Rho= 0.110 | - |
| p= 0.309 | p= 0.009* | p= <0.001* | p= 0.008* | p= 0.542 | - |
Note: *P<0.05
Table 3: Spearman’s Rho analysis showing no correlation between DEDM scores and DEQ-5 scores.
Impact of DED on daily activities, mental health and finances
42.80% of charts documented patients reporting an inability to enjoy their daily activities due to DED symptoms are shown in Table 4. The top three activities impacted by DED were reading (30.43%), spending time at the computer or watching TV (26.08%), and driving (17.39%) (Figures 2a-2c). As part of routine DED consultations, patients were screened for mental health challenges and asked to comment on the severity of their challenges as well whether they wished to be referred to social work team at the hospital for additional support. 48.00% of charts reviewed indicated no mental health difficulties. 52.00% of participants reported feeling either depressed, anxious, or both and 26.92% had accepted a referral to speak with a social worker when offered. More than a quarter of the charts documented patients reporting financial challenges associated with their DED. Similarly, more than a fifth of patients revealed that financial challenges were a barrier to accessing DED therapy (Table 4).
| N | % or Mean | |
|---|---|---|
| Do your dry eye symptoms limit your ability to perform daily activities? | 35 | |
| Yes | 15 | 42.86% |
| No | 20 | 57.14% |
| Emotional hardship caused by dry eye (on scale of 1 to 5) | 27 | |
| 1 | 16 | 59.26% |
| 3 | 6 | 22.22% |
| 2 | 4 | 14.81% |
| Feelings of depression or anxiety due to dry eye | 25 | |
| Depressed | 6 | 24.00% |
| Anxious | 4 | 16.00% |
| Both depressed and anxious | 3 | 12.00% |
| Neither depressed or anxious | 12 | 48.00% |
| Accepted referred to social worker for depression and/or anxiety | 26 | |
| Yes | 7 | 26.92% |
| No | 19 | 73.08% |
| Financial challenge of DED (on a scale of 1-5) | 26 | |
| 1 | 19 | 73.08% |
| 3 | 5 | 19.23% |
| 4 | 2 | 7.69% |
| Cost of DED therapy as a deterrent of therapy | 26 | |
| Yes | 6 | 23.08% |
| No | 20 | 76.92% |
Table 4: Impact of DED on mental, emotional and financial well-being.
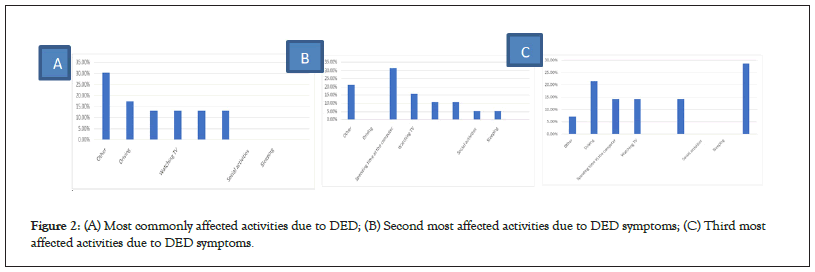
Figure 2: (A) Most commonly affected activities due to DED; (B) Second most affected activities due to DED symptoms; (C) Third most affected activities due to DED symptoms.
Impact of COVID-19 lockdown on DED
One-fifth of charts documented worse DED symptoms during the lockdown period compared to prior to the lockdown period are shown in Table 5. 17.14% of patients reported the lockdown negatively affected their ability to perform their DED self-care routine, 2.00% reported their self-care routine was better during the lockdown, and the remaining indicated no change (Table 5).
| N | % | |
|---|---|---|
| Effect of COVID on DED symptoms | 35 | |
| Negative effect | 7 | 20.00% |
| Positive effect | 1 | 2.86% |
| No effect | 27 | 77.14% |
| Effect of COVID on DED self-care routine | 35 | |
| Negative effect | 6 | 17.14% |
| No effect | 29 | 82.86% |
| Effect of COVID on time spent on computer or other screen | 34 | |
| More time spent | 15 | 44.12% |
| Less time spent | 19 | 55.88% |
Table 5: Impact of covid-19 on DED.
In this study, telephone consultations provided clinically useful information, allowing the cornea specialist to assess and grade patients’ current DED symptoms, impact on activities of daily living and mental health, and success in engaging in DED selfcare activities. In addition, the virtual format allowed patients to disclose challenges requiring additional support to cope with DED. Virtual consultations identified patients warranting further investigations for sjogren’s disease. In terms of treatment, telephone consultations allowed for initiation of optimal DED management, and allowed for triaging patients for subsequent inperson assessment.
DED symptoms and self-care
In this preliminary chart review, patients were referred to a cornea specialist after an average of 6 years of DED symptoms, and almost three quarters of patients had moderate or severe DED symptoms according to CDEA scores. The majority of patients reported using artificial tears and warm compresses, and less than half reported using omega-3 supplements. Among those who used artificial tears, many were using drops less than four times per day despite the severity of symptoms reported. Among those who took omega-3 supplements, approximately one third were taking less than the 2000 mg recommended daily dose. With the information obtained, patients were counselled regarding optimal DED self-management and educated regarding optimal follow-up and future treatment modalities.
The DEDM score is a novel parameter created to capture overall DED management practices employed by patients. This measure allows researchers to understand how many of the five main practices were employed, to get a sense of self-management in totality. The composite score is a novel way to assess the relationships between patient treatment behaviours/practices and disease severity.
A significant correlation was identified between the frequency of artificial tear use and DEQ-5 scores. This was expected as worse symptoms intuitively warrant more tear use per day. In addition, the frequency of artificial tear use was correlated with overall DED management composite scores. Perhaps respondents who use tears more often are also more diligent about other elements of their DED self-care, or have the financial means to engage in more elements of self-care. The frequency of artificial tear use correlated with the number of eye care visits per year, suggesting that more severe DED symptoms may lead to greater healthcare seeking behaviour. Financial means and/or insurance coverage allow patients to afford the cost of both artificial tears and additional eye care appointments. Moreover, seeing an optometrist more frequently may increase the likelihood of adherence to therapy.
DED and financial barriers to therapy
Financial barriers associated with therapy may lead to poor adherence to DED self-care. Nearly a quarter of patients reported that the cost of dry eye therapy was a deterrent to therapy adherence. This is consistent with other studies that reported the cost of DED therapy represented an average annual out of pocket expense of $ 1,089 Canadian Dollar (CAD) per year [14] and $ 678- $ 1,267 United States Dollar (USD) per year [15]. Moreover, this study found patients to be underutilizing artificial tears and omega-3 supplements. Financial barriers promote rationing of artificial tears and other therapeutics, as reported by Michaelov [14]. In addition, financial struggles are likely underreported by patients to eye care providers as previous studies have shown that non-adherence to therapy due to financial reasons is often not disclosed by patients to their health care providers [14]. Furthermore, the COVID-19 pandemic has resulted in financial stressors for a large proportion of the population, as reported in a study that found 40% of US adults experienced COVID-19- related financial stressors from March to August 2020 [16].
In this study population, patients visited their optometrist an average of 1.61 times per year. Interestingly, there was no correlation between frequency of visits and symptom severity. For some patients, insurance coverage may limit visits to once per year. The lack of private insurance coverage may also be a financial barrier to care. Literature demonstrates that lack of government-insured optometric services was found to negatively impact patients’ access to health care services, and ultimately vision health outcomes [17]. However, these would be important relationships to evaluate in a larger study sample.
DED and mental health
In this study, over half of patients reported either anxiety, depression, or both, as a result of DED symptoms. This may be directly associated with symptoms of dry eye, or associated with difficulty performing daily activities due to DED symptoms. This is consistent with literature demonstrating the association between DED and mental health issues including anxiety and depression [6,18].
Over a quarter of patients accepted a referral to a social worker for support regarding living with DED. These findings highlight the importance of inquiring about mental health during DED appointments and may inform the rationale behind incorporating mental health screening into the standard of care for DED. This is essential given the high prevalence of mental health concerns among DED patients [4,7]. Optometrists and ophthalmologists should not only prioritize inquiring about mental health, but also ensure they have the appropriate resources to provide to patients, such as a referral to a social worker, other mental health services, or to primary care providers.
Moreover, poor mental health may be exacerbated by the COVID-19 pandemic. There was a marked increase in the number of Canadians reporting ‘poor or fair’ mental health between March and May 2020, over half of which reported the decline in mental health was directly associated with lockdown measures that resulted in social isolation [19]. In addition, the Canadian Mental Health Association (CMHA) reported Canadians were more likely to believe their mental health had worsened compared to physical health during the pandemic [20]. While this study was not designed to evaluate an association or temporality between mental health, DED, and COVID-19, we acknowledge the possibility that there may be interactions between these variables.
DED symptoms and the COVID-19 pandemic
One-fifth of patients reported the pandemic made their DED symptoms worse, and 17% reported it negatively affected their ability to perform their DED self-care. Only 2% reported their symptoms improved. Nearly half of patients reported spending more time using screens, which may be contributing to the worsening symptoms.
Many non-essential medical visits and procedures were postponed due to provincial public health directives. In many cases, this resulted in a negative impact on health outcomes. Through virtual consultations, the patients in this study were assessed and counselled with respect to optimizing their DED self-care management. Despite the lack of physical exam findings such as VA, IOP, and Systemic Lupus Erythematosus (SLE), virtual appointments may serve as a valuable way to initiate management until in-person visits are possible. Moreover, telephone appointments constitute a form of virtual care that doesn’t involve apps or video chat, making the modality user-friendly for both clinicians and patients. This achieves a similar goal as in person appointments when specialists provide counseling to patients and advice to referring providers.
Other forms of virtual care have been employed in ophthalmology. For example, in glaucoma virtual care, patients have been given handheld tonometers to measure IOP remotely to supplement video chat appointments [21]. Others are using specialized video chat equipment to allow for improved visualization of the eye during virtual appointments. Recommendations for virtual care within the Canadian healthcare system include introducing education on telemedicine for medical students, and training in telemedicine for physicians with regards to delivery of virtual care, performing virtual patient examinations, and incorporating virtual care into their existing medical practices [22].
Limitations
This study had a limited sample size due to the study objectives. Firstly, to provide preliminary exploratory data to examine patient experience with DED during the COVID-19 pandemic, and report on the use of telephone consultations for DED referrals. Further studies are needed to better understand the effect of the COVID-19 pandemic on DED patients, as well as to evaluate the use of telephone, or other virtual care modalities, for DED consultations.
Secondly, there are limitations to the composite scoring used in data analysis to capture how many elements of self-care patients were engaging in. The composite score weighed each self-care practice equally and without regard for variation, for example using one drop of artificial tears per day versus four times per day. In addition, not all therapies, or frequencies of therapies, are necessarily equally effective.
Finally, there are limitations to the virtual care modality itself. There were communication challenges over the telephone with some patients. This was especially evident in elderly patients, patients who were hard of hearing, and patients with language barriers. With regards to ophthalmological considerations, physical exam parameters such as VA, IOP, and SLE are impossible to conduct virtually. Though the most recently documented VA and IOP values were obtained from optometrist and ophthalmologist referral letters, the lack of contemporaneous VA, IOP, and SLEs may represent a limitation to care.
Telephone consultations for patients with DED may be an effective way to assess dry eye disease symptom severity, the impact of symptoms on daily functioning, and the need for counselling and support. In this chart review, patients living with DED reported symptoms that negatively affected their daily activities including mental health and financial challenges, which in turn impact their ability to perform dry eye management activities. These challenges may have been exacerbated during the COVID-19 pandemic lockdown. Despite challenges and limitations, it is evident that simple virtual care via telephone will continue to play an integral role in DED care in the future.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
No funding was received to assist with the preparation of this manuscript.
The manuscript does not contain clinical studies or patient data.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ibrahim P, McKenna CG, Mather R (2022) Virtual Assessment of Patients with Dry Eye Disease during the COVID-19 Pandemic: One Clinician’s Experience. J Cli Exp Ophthalmol.13:928.
Received: 01-Sep-2022, Manuscript No. JCEO-22-16609; Editor assigned: 05-Sep-2022, Pre QC No. JCEO-22-16609 (PQ); Reviewed: 19-Sep-2022, QC No. JCEO-22-16609; Revised: 26-Sep-2022, Manuscript No. JCEO-22-16609 (R); Published: 05-Oct-2022 , DOI: 10.35248/2155-9570.22.13.928
Copyright: © 2022 Ibrahim P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.