Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2024)Volume 15, Issue 6
Introduction: Toxic Anterior Segment Syndrome (TASS) is a non-infectious anterior chamber reaction caused by ocular surgeries. It usually develops within the first 12-48 hours after surgery. In case of clinical suspicion of TASS, endophthalmitis as a devastating disease should always be excluded. However, the fact that TASS and endophthalmitis can look the same, but the treatment for each is different. Therefore, distinguishing between the two conditions is an important factor in coping with both diseases. It was aimed to describe the features and clinical management that are considered when distinguishing the cause of unexpected inflammatory response after cataract surgery.
Setting: Ege university ophthalmology department, retrospective review of medical records.
Method: A total of 13 patients who developed TASS in our clinic on 3 different days between July 2022 and December 2022 were included in this study. Anterior segment photographs of those 13 patients, the records of ophthalmological examinations of those patients including Best Corrected Visual Acuity (BCVA), ocular pressure, biomicroscopic and fundoscopic examination were collected. Medical data were evaluated retrospectively.
Results: The mean time to onset of clinical symptoms was 27.6 hours. The main complaint was pain in nine patients. The primary symptom in the remainder of the patients was blurred vision. Severe hypopyon was seen in 5 cases. Despite the presence of pain and hypopyon, patients who were treated with topical steroids were closely followed up (every 2 hours) because they were consecutive patients and had relatively acute onset complaints. Inflammation was regressed after an average of 4 hours. No factor causing TASS was found. The BCVA was at the minimum level of 8/10 on the 5th day of surgery.
Conclusion: When distinguishing TASS from endophthalmitis, severe pain, relatively late onset, hyperaemia and the presence of severe hypopyon usually lead ophthalmologists to the clinical diagnosis of endophthalmitis. However, in this study, most of the patients diagnosed with TASS had severe pain, a significant portion of them had hypopyon and the onset of the symptoms is relatively late. Close follow-up immediately after suspicion plays a vital role in clinical diagnosis and management accordingly.
Toxic anterior segment syndrome; Endophthalmitis; Cataract surgery; Hypopyon; Ocular inflammation
Intense inflammation after cataract surgery is a clinical picture that ocular surgeons do not like to observe. We consider two main pathologies, endophthalmitis and toxic anterior segment syndrome, in line with the onset time, main complaints and clinical findings when we encounter this rare condition.
TASS is a non-infectious postoperative inflammation with a good clinical course, most commonly occurring after cataract surgery [1]. It can occur in both sporadic and clustered outbreaks [2]. The incidence after cataract surgery is probably around 1 in 1000. Although its pathophysiology is unclear, TASS represents an inflammatory response to a substance typically used during surgery, such as an endotoxin-containing balanced salt solution, viscoelastic, and intracameral antibiotic [3]. Sometimes a cause cannot be determined.
Acute post-operative endophthalmitis is a serious intraocular inflammatory disorder with a poor visual prognosis that causes infection in the vitreous cavity with direct inoculation of microorganisms. When these two clinical entities with significant inflammation are compared, there are differences in duration of onset, incidence in consecutive patients, and symptoms and signs.
However, the fact that TASS and endophthalmitis can look exactly the same, but the treatment for each is different, is an important problem in ophthalmology practice. Therefore, distinguishing between the two conditions is an important factor in coping with both diseases.
The aim of this study was to describe the features and clinical management that are taken into account when distinguishing the cause of unexpected inflammatory response after cataract surgery.
A total of 13 patients who developed TASS in our clinic on 3 different days between July 2022 and December 2022 were included in this study. Anterior segment photographs of those 13 patients, the records of ophthalmological examinations of those patients including Best Corrected Visual Acuity (BCVA), ocular pressure, biomicroscopic and fundoscopic examination were collected. Medical data were evaluated retrospectively [4].
A total of 13 cases diagnosed with TASS on 3 different days after cataract surgery were presented here. The cohort is composed of 7 male and 6 female patients with an average of 68.84 years ± 11.34 years of age. 3 piece IOL was used in each cataract surgery and no other surgical complication was observed during these surgeries.
The mean time to onset of clinical symptoms was 27.6 hours. All patients had complaints of blurred vision. However, the main complaint was pain in nine patients, while the rest of them complaint of blurred vision primarily. Corneal edema was seen in all cases. One patient, which has macular degeneration preoperatively, presented with vitritis at the time of TASS diagnosis. Severe hypopyon was seen in 5 cases [5]. All patients were admitted to the hospital at the time of their initial complaint and topical steroid administration was initiated. 1 mg/kg methylprednisolone IV was given only to the patient who had vitritis. Each patient was followed up every 2 hours. Despite the presence of pain and hypopyon, patients who were treated with topical steroids were closely followed up because they were consecutive patients and had relatively acute onset complaints. Clinical characterestics of 13 TASS cases [6].
In the follow-ups, the signs of inflammation regressed after an average of 4 hours. As a result of the evaluations, no factor causing TASS was found in the cases. Visual acuity was recovered at the minimum level of 8/10 on the 5th day of surgery except for one patient. The patient with preoperative macular degeneration had a final visual acuity of 0.05, which is equal to the preoperative visual assessment, after complete recovery from TASS. Even the recovery took the longest in the patient with vitritis, in the end no resting complication due to TASS was observed in any case [7].
Figure 1 shows the clinical course of a TASS case with close follow-up intervals. The patient was admitted to the clinic at the post-operative 20th hour with corneal edema and hypopyon and treatment was initiated accordingly (Figure 1A). At the postoperative 24th hour hypopyon regressed (Figure 1B). At the postoperative 40th hour corneal edema and hypopyon regressed totally (Figure 1C).
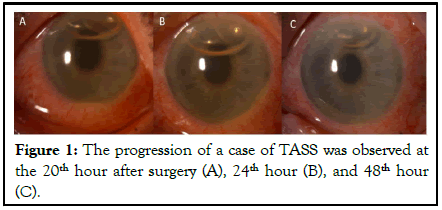
Figure 1: The progression of a case of TASS was observed at the 20th hour after surgery (A), 24th hour (B), and 48th hour (C).
The clinical progression of pre-surgical macular degeneration in a patient is depicted in Figure 2. The patient presented with corneal edema and hypopyon, which were observed at the 24th hour after surgery (Figure 2A). To address these symptoms, the patient received topical corticosteroid treatment, which led to a decrease in edema and hypopyon by the 48th hour (Figure 2B). By the 72nd hour, the edema and hypopyon had resolved completely (Figure 2C) [8].
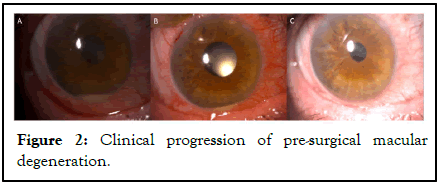
Figure 2: Clinical progression of pre-surgical macular degeneration.
The main distinguishing features between TASS and infectious endophthalmitis, which we refrain from encountering after cataract surgery and cause ocular inflammation, are the onset, speed of symptom progression, pain, and presence or absence of vitiritis. However, both conditions may present with poor visual acuity, corneal inflammation, and significant anterior chamber reaction.
Cases of TASS usually develop within the first 12 hours-48 hours after surgery, while cases of endophthalmitis usually occur between days 3 and 10 post-surgery [5,6]. As an exception, endophthalmitis due to Bacillus cereus may occur within the first 18 hours-24 hours after surgery. Therefore, although early onset of symptoms may lead to the diagnosis of TASS, it is not definitive in terms of diagnosis. In this study, the onset time was between 24 hours-48 hours and was detected in the relatively early period [9].
Although the presence of pain as a symptom is primarily in favour of endophthalmitis, pain may also accompany in TASS cases. In this study, pain was the first symptom in 69.23% of the cases, which was different from what was expected.
As mentioned before, symptoms of endophthalmitis after cataract surgery occur within 1 week in 75% of cases, and hypopyon is present in >80% of them [8]. TASS is characterized by a sterile anterior chamber reaction. Any surgical instrument, sterilization material or solution used during the surgery can trigger this reaction, organic or non-organic. Sometimes the cause cannot be determined. In this study, hypopyon was evident in approximately 40% of the patients and the factor that would trigger inflammation could not be detected in the evaluation.
TASS represents an inflammatory response to a substance that is typically used during surgery, such as a balanced salt solution containing endotoxin, viscoelastic and intra-carneral antibiotics, and thus cases of TASS can develop as an outbreak. In this study, the fact that the patients were seen in clusters on 3 separate days led us in favour of TASS.
Although TASS and endophthalmitis may have similar clinical features, their management is completely different. The priority in endophthalmitis is to control the infection with intensive antimicrobial use. Whereas TASS develops as a sterile inflammatory reaction in the anterior chamber, therefore the main treatment for TASS is topical corticosteroid administration. However, ocular pressure elevation due to topical corticosteroid therapy should always be monitored. In addition, chronic trabeculitis or peripheral anterior synechia formation due to TASS may permanently damage the trabecular meshwork, leading to reduced trabecular outflow and secondary glaucoma. In case of elevated ocular pressure, the use of prostaglandin analogues should be avoided to prevent an inflammatory reaction in the anterior chamber. Topical steroid was started in all of the cases in this study, and additional systemic steroid treatment was added to one patient with mild anterior vitiritis [10].
Although pain and hypopyon in favour of endophthalmitis in these cases cast doubt on us, the primary diagnosis was considered in favour of TASS, due to the time of onset of symptoms and the occurrence of clusters of cases. However, for precautionary purposes, the patients were hospitalized and treated and evaluated according to the clinical course in close follow-up. TASS, which is generally known to have a good prognosis, progressed well in the cases in this study and the inflammatory response regressed without any complications in all patients.
In conclusion, encountering severe inflammation in the postoperative period in cataract surgery is an important source of fear for ocular surgeons. Both TASS and endophthalmitis are undesirable complications, and the similarity of their clinics and the completely different treatment approaches continue to be a challenge for clinicians. For this reason, in such a case, considering the characteristics of the symptoms and signs from multiple perspectives, the patient should be followed closely, and the treatment should be applied.
None.
No funds, grants, or other support were received.
The authors have no relevant financial or non-financial interests to disclose. Author Muhammed Dara Tas declares that he has no conflict of interest. Author Anil Kaplan declares that she has no conflict of interest; author Ozlem Barut Selver declares that she has no conflict of interest.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kaplan A (2024) Unusual Inflammatory Clinical Presentation after Cataract Surgery and that Thought-Provoking Question: Is this Infection or Toxic Anterior Segment Syndrome? J Clin Exp Ophthalmol. 15:992.
Received: 26-Apr-2023, Manuscript No. JCEO-23-23766; Editor assigned: 28-Apr-2023, Pre QC No. JCEO-23-23766 (PQ); Reviewed: 12-May-2023, QC No. JCEO-23-23766; Revised: 22-Jul-2024, Manuscript No. JCEO-23-23766 (R); Published: 29-Oct-2024 , DOI: 10.35248/2155-9570.24.15.992
Copyright: © 2024 Kaplan A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.