Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 4
Objective: To evaluate the feasible, effective procedures in the traumatic cataract extraction,through23-gauge (G)Pars Plana Vitrectomy (PPV) and one-step removal of posterior segment intraocular foreign bodies (IOFBs) via scleral tunnel incision.
Methods: This is a retrospective case-series study, 30 eyes of 30 patients with penetrating corneal injury with traumatic cataract and posterior segment IOFBs from January 2015 to January 2021 at the People’s No.1 Hospital of Chenzhou and the Changsha Aier Eye Hospital were enrolled. After traumatic cataract extraction and 23G PPV treatments, intravitreal foreign body tweezers were used to extend the anterior chamber into the vitreous cavity from the 12-point scleral tunnel incision and the posterior segment foreign body was clamped. The routine follow-up as 1,2 weeks and 1,3,6 and 12 months after surgery. The Best Corrected Visual Acuity (BCVA), Intraocular Pressure (IOP) and retinal conditions were recorded.
Results: Among the 30 patients, 29 were male and 1 female, the follow-up time is (9.57 ± 1.94) months. 17 cases were intravitreal foreign bodies, 11 cases were extra retinal macular foreign bodies and 2 cases were intraretinal macular foreign bodies. All posterior segment IOFBs were one-step removed through the scleral tunnel incision, without the need for the delayed removal or the need for 23-gauge scleral puncture through enlarged the incision. The final BCVA improved for 25 eyes (83.33%), the BCVA unchanged for 4 eyes (13.33%), and the BCVA decreased by 1 eye (3.33%) (t final vs. OP at vitreous=0.0372 **p<0.01; t final vs. OP at retinal=0.0627 *p<0.05). No scleral puncture associated complications. One patient had Retinal Detachment (RD).
Conclusion: The Traumatic cataract extraction, 23-gauge PPV and one-step removal of the posterior segment IOFBs via a mini-puncture scleral tunnel incision, are feasible and effective in treating the posterior segment IOFBs combined with traumatic cataract, which benefits to reduce scleral complications and improve the BCVAs.
Intraocular foreign bodies (IOFBs); Pars plana vitrectomy (PPV); Phacoemulsification; Scleral tunnel incision; Penetrating ocular trauma
23-G: 23-gauge; PPV: Pars Plana Vitrectomy; IFOBs: Intraocular Foreign Bodies; BCVA: Best Corrected Visual Acuity; IOP: Intraocular Pressure; RD: Retinal Detachment; CT: Computer Tomography; ANOVA: Analysis of Variance; CCC: Continuous Curvilinear Capsulorhexis; NLP: No Light Perception; IOLs: Intraocular Lens; PFCL: Per Fluorocarbon Liquid.
Ocular trauma is the leading cause of blindness of single eye and is more serious in developing countries. The posterior segment Intraocular Foreign Bodies (IOFBs) are the relatively usual and critical injury, especially in young and middle-aged male physical workers. In addition to the initial destructions caused by foreign bodies, it can also cause serious complications such as rust, retinal detachment and endophthalmitis [1,2]. The visual prognosis depends on the location and size of IOFBs, the damaged integrity of eyeball or whether it has caused complications and obtained the timely and effective treatments [2,3].
Removal of IOFBs is one of the most challenging operations. The purpose of this operation is to remove IOFBs from the eyeball through a minimally invasive channel and to treat lesions caused by the trajectory of foreign bodies in the eye. Pars Plana Vitrectomy (PPV) is currently the standard procedure for the treating lesions in the posterior segment of the eye. In case of IOFBs, PPV can well unveil IOFBs, accurately detect retinal configuration, helps for the direct intraocular laser of retinal holes. How to remove IOFBs with the minimal damage to avoid the iatrogenic destroy is the ambition of oculists [4,5].
Until to now, 20 G vitreous cutting puncture may cause sclera pierce complication; 23 G minimally invasive vitreous cutting technique can protect the stab owing to the application of the cannula, greatly reducing the incidence of prick-related complications [6]. Some oculist remove the posterior segment IOFBs through an in-situ enlarged sclera channel, but this incision may cause lower intraocular pressure, vitreous hemorrhage, entrapment of the surrounding vitreous gelatins into the wound, retinal holes, suprachoroidal hemorrhage, “saw tooth” margin dislocation, retinal detachment [7,8].
In this study, 30 cases of corneal penetrating trauma with traumatic cataract and posterior segment IOFB were treated by traumatic cataract extraction, 23 G PPV and one-step removal of the posterior segment IOFBs by way of scleral tunnel incision. The safety, effectiveness and reproducibility of this procedure will be discussed.
General data
Project design: This is a retrospective case clinic trail. The clinical data of 30 patients (30 eyes) with penetrating corneal injury combined with traumatic cataract and posterior segment IOFBs in the Department of Ophthalmology of the First People’s Hospital of Chenzhou and the Changsha Aier Eye Hospital from January 2015 to January 2021 were collected. There were 29 males and 1 female. The age ranged from 16 to 68 years, with the average age of (40.0 ± 6.15) years. In all cases, routine examination of visual acuity, non-contact intraocular pressure, indirect ophthalmoscopes and B-ultrasound were performed before operation to be affirmation; Computer Tomography (CT) examination of the eyes were performed before operation, and it was certain that there were foreign bodies located in the posterior segment of the eye. Preoperative vision are variation from No Light Perception (NLP) ~ 0.1 (Snellen optotype).
Inclusion and exclusion criteria: All the study subjects were enrolled during January 2015 to January 2021 who met the inclusion criteria were of the same ethnicity (Chinese, Han, aged between 16 and 68 years). Patients with corneal penetrating trauma with traumatic cataract and posterior segment IOFB by routine and ophthalmic image test were selected from amongst subjects who visited the inpatient hospitalization for therapy.
We excluded patients less than 14 years of age or more than 70 years old; those with histories of ocular surgery and injury within 3 months; those with ocular diseases such as ocular infection, allergy, and nasolacrimal disease. Patients whose outcome measures could not be determined were excluded.
Medical ethics: This study followed the principium of the Declaration of Helsinki, and this protocol was approved by the Institutional Review Board of the Ethnic Committee of the First People’s Hospital of Chenzhou, Hengyan Medical School, University of South China (ID:2015KYYJ003) informed consent was achieved to the recruiters after an discussion of the purpose and probability on sequences of the clinic trail.
Surgical procedure and medicine treatments
These operations are performed under general or local anesthesia according to patients’ condition. Surgeries were performed by the same surgeon group (Zhu JDM.D, Zhiyuan Li M.D). Suture the unhealed corneal penetration wound first; make a conjunctiva flap based on the dome at 12 o’clock, make a 3.2 mm wide scleral tunnel incision 1 mm posterior from the limbus, and the inner mouth of the stepped incision is located 0.5-1 mm at the transparent cornea; make a 1 mm clear limbus incision at 2 o’clock or 10 o’clock. Inject an viscoelastic intermedium into the anterior chamber, perform a 5 mm Continuous Curvilinear Capsulorhexis (CCC) or partial capsulorhexis or bite an anterior capsular flushes off with a 23-gauge vitreous cutter according to the damage of the anterior capsular of the lens, try to keep the peripheral capsule stable to facilitate the second-stage IOL implantation. Dry hydro dissection was performed and phacoemulsification was used to remove the party nucleus and erase the residues lens cortex. For patients with soft nucleus, lens bite removal is possible. Using a 23 G vitreous cutter to bite a posterior capsule out restricted to 4 mm according to the posterior lens capsule injury. Perform a standard supra temporal 23 G scleral puncture and set the perfusion head below the temporal; then perform vitrectomy to clear blood, make certain that the position of the foreign body in the cavity and detect the situation of the retina; grasp the timing of foreign body removal according to the intraoperative situation, broaden the scleral tunnel incision according to the magnitude of the foreign body as least as possible, insert the vitreous foreign body forceps directly extend into the vitreous cavity through the scleral tunnel incision, grab the foreign body under direct light guidance, and remove the foreign body at the posterior segment bypass the anterior chamber canal through one step procedure. In some surgeries, after the main vitrectomy and removal of the vitreous surrounding the IOFBs, Perfluorocarbon Liquid (PFCL) was injected over the macula. Finally, complete vitrectomy (perfluorocarbon liquid replacement, direct retinal laser photocoagulation, gas-liquid exchange, silicone oil or gas filling) have been taken according to the situation of retinal injury to make the retinal reposition. For those suppurtive endophthalmitis, try to remove the vitreous body, and inject 1.0 mg/0.1 mL vancomycin, 2.25 mg/0.1 mL ceftazidime, and 1.0 mg/0.1 ml dexamethasone mixture into the vitreous cavity after surgery (Figure 1).
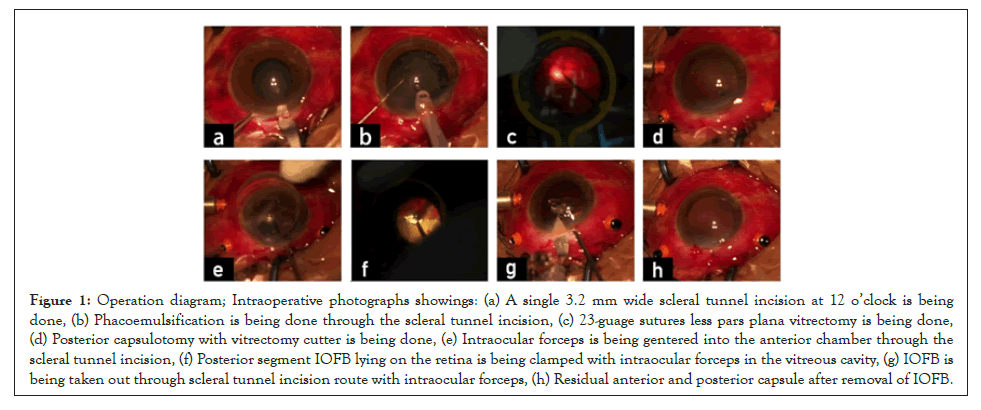
Figure 1: Operation diagram; Intraoperative photographs showings: (a) A single 3.2 mm wide scleral tunnel incision at 12 o’clock is being done, (b) Phacoemulsification is being done through the scleral tunnel incision, (c) 23-guage sutures less pars plana vitrectomy is being done, (d) Posterior capsulotomy with vitrectomy cutter is being done, (e) Intraocular forceps is being gentered into the anterior chamber through the scleral tunnel incision, (f) Posterior segment IOFB lying on the retina is being clamped with intraocular forceps in the vitreous cavity, (g) IOFB is being taken out through scleral tunnel incision route with intraocular forceps, (h) Residual anterior and posterior capsule after removal of IOFB.
Postoperative routine examinations and follow-up
Revisit regularly within 1 week, 2 weeks, and 1,3,6, and 12 months after surgery. Follow-up scheduled time was 12 months, with the average of (9.57 ± 1.94) months. Observe and record the Best Corrected Visual Acuity (BCVA), Intraocular Pressure (IOP) and retinal conditions of the eye and elect silicone oil removal and the second-stage intraocular lens suspension according to the fundus condition.
Intraoperative conditions
17 (56.67%) cases were intravitreal foreign bodies, 11 (36.67%) cases were extraretinal macular foreign bodies, and 2 (26.67%) cases were intraretinal macular foreign bodies. Eight (26.67%) cases with retinal holes, three (10%) had retinal detachment, and four (13.33%) with suppurative endophthalmitis. In this group of patients, 11 (36.67%) patients underwent primary corneal debridement and suture combined with lens vitreous surgery; 19 (63.33%) patients underwent corneal debridement and suture in first stage, and then underwent second-stage vitreoretinal surgeries 5-7 days after maiden injury to remove foreign bodies. All patients had undertaken the successfully remove of the foreign body at the posterior segment of the eye through a one-step scleral tunnel incision, without the need for foreign body delayed removal, or without the need for 23-gauge scleral puncture to broaden the incision. The surgery success rate arounds 100%. During the operation, 8 (26.67%) cases were treated with perfluorocarbon liquid, 18 (60%) cases were treated with intraocular laser photocoagulation, 7 (23.33%) cases were temped with silicone oil, and 2 (6.67%) cases were temped with disinfection air.
Surgical outcomes
17 (56.67%) patients underwent the second-stage intraocular lens implantation; 15 (50%) cases with IOL implantation into the ciliary sulcus and 2 (6.67%) cases with IOL suspension. Eventually, visual acuity improved for 25 (83.33%) eyes, visual sight within same range for 4 (13.33%) eyes (Figures 2 and 3).
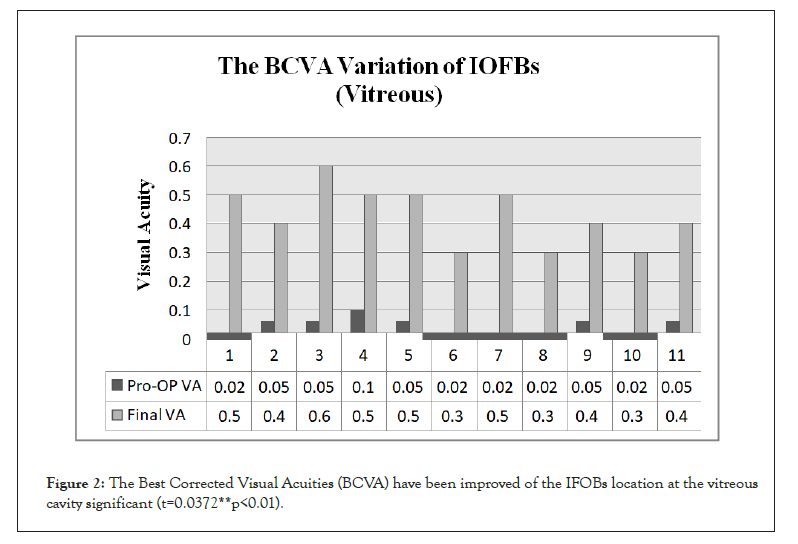
Figure 2: The Best Corrected Visual Acuities (BCVA) have been improved of the IFOBs location at the vitreous cavity significant (t=0.0372**p<0.01).
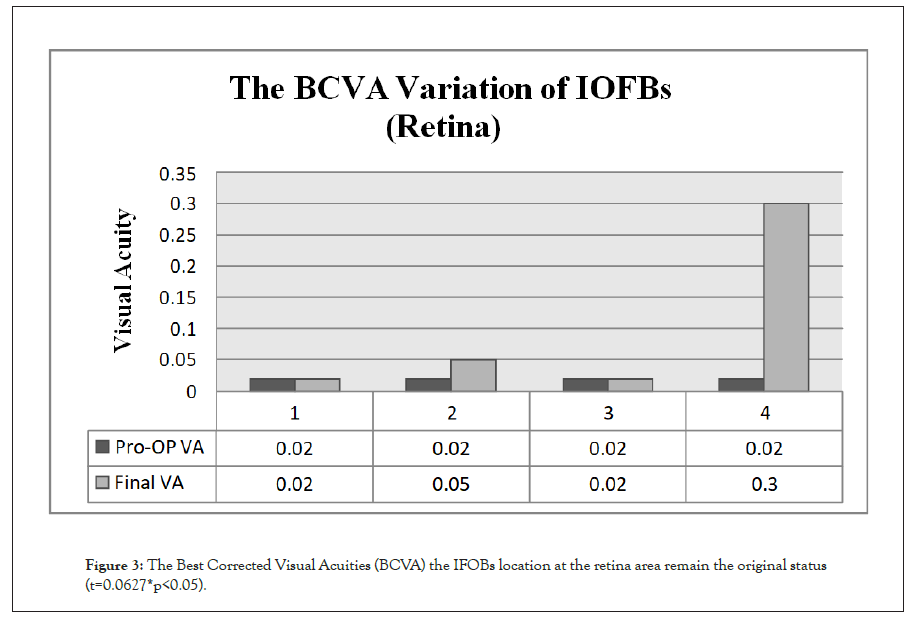
Figure 3: The Best Corrected Visual Acuities (BCVA) the IFOBs location at the retina area remain the original status (t=0.0627*p<0.05).
Complications
8 (26.67%) cases have intraoperative corneal epithelial edema, corneal epithelial curettage. One (3.33%) case with intraocular hemorrhage during surgery. Ten (33.33%) cases of anterior chamber inflammatory reactions after operation were assimilated within 10 days after anterior segment surgery. One (3.33%) case had retinal detachment due to secondary PVR. The operation was performed further to reset the retina. None of the 30 patients had complications related to scleral puncture (Table 1).
| Case | Age | Gender | IOFB Location | Size of IOFB (mm) | Endophthalmitis | Intraoculart amponade | IOL Implantation | Preoperative BCVA | Final visit BCVA | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 40 | Male | Vitreous | 3.5 | No | No | Yes | 0.02 | 0.5 | |||
| 2 | 48 | Male | Vitreous | 4 | No | No | Yes | 0.05 | 0.4 | |||
| 3 | 40 | Male | Retina | 4.5 | No | Silicone oil | Yes | 0.02 | 0.3 | |||
| 4 | 28 | Male | Vitreous | 6 | Yes | Silicone oil | No | No light | No light | |||
| 5 | 56 | Male | Retina | 3.5 | No | Gas | Yes | 0.02 | 0.02 | |||
| 6 | 20 | Male | Vitreous | 7 | No | Gas | No | HM | 0.05 | |||
| 7 | 16 | Male | Retina | 5 | No | Silicone oil | No | CF | 0.1 | |||
| 8 | 60 | Male | Vitreous | 4 | No | No | Yes | 0.05 | 0.6 | |||
| 9 | 33 | Male | Macule | 8 | Yes | Silicone oil | No | Light | No light | |||
| 10 | 45 | Male | Retina | 5 | No | Silicone oil | No | 0.02 | 0.05 | |||
| 11 | 31 | Male | Vitreous | 4 | No | No | Yes | 0.1 | 0.5 | |||
| 12 | 24 | Male | Retina | 6 | No | Silicone oil | No | HM | 0.02 | |||
| 13 | 37 | Male | Vitreous | 3.5 | No | No | Yes | 0.05 | 0.5 | |||
| 14 | 39 | Male | Retina | 5 | No | Silicone oil | No | CF | 0.05 | |||
| 15 | 41 | Male | Vitreous | 4 | No | No | No | CF | 0.4 | |||
| 16 | 68 | Male | Vitreous | 3.5 | No | No | Yes | 0.02 | 0.3 | |||
| 17 | 43 | Male | Retina | 5 | No | Silicone oil | No | CF | 0.05 | |||
| 18 | 49 | Female | Vitreous | 3.5 | No | No | Yes | CF | 0.3 | |||
| 19 | 57 | Male | Macule | 4 | No | Silicone oil | No | HM | CF | |||
| 20 | 26 | Male | Retina | 5 | Yes | Silicone oil | No | HM | HM | |||
| 21 | 32 | Male | Vitreous | 4.5 | No | No | Yes | 0.02 | 0.5 | |||
| 22 | 54 | Male | Vitreous | 6 | No | Gas | Yes | CF | 0.2 | |||
| 23 | 42 | Male | Vitreous | 5.5 | No | Gas | Yes | CF | 0.3 | |||
| 24 | 25 | Male | Vitreous | 5 | Yes | No | Yes | 0.02 | 0.3 | |||
| 25 | 34 | Male | Retina | 4 | No | Silicone oil | No | 0.02 | 0.02 | |||
| 26 | 29 | Male | Vitreous | 4.5 | No | No | Yes | 0.05 | 0.4 | |||
| 27 | 62 | Male | Retina | 6.5 | No | Silicone oil | No | HM | 0.05 | |||
| 28 | 50 | Male | Vitreous | 3.5 | No | No | Yes | 0.02 | 0.3 | |||
| 29 | 44 | Male | Retina | 4 | No | Silicone oil | Yes | CF | 0.2 | |||
| 30 | 32 | Male | Vitreous | 3.5 | No | No | Yes | 0.05 | 0.4 | |||
Note: IOFB: Intraocular Foreign Body; IOL: Intraocular Lens; BCVA: Snellen Best Corrected Visual Acuity; HM: Hand Movement; CF: Finger Count
Table 1: Pre and post-operative characteristics of the cases.
The best corrected visual acuity can be improved by the one-step removal of posterior segment intraocular foreign bodies via scleral tunnel incision procedure: 62% of these patients can achieve the final BCVA more than 0.3, 24% of these patients can achieve the final BCVA more than 0.5 whose IOFBs fall at the vitreous cavity, only 14% of these patients with the final BCVA less than 0.3 whose IOFBs fall at the vitreous cavity (Figure 4).
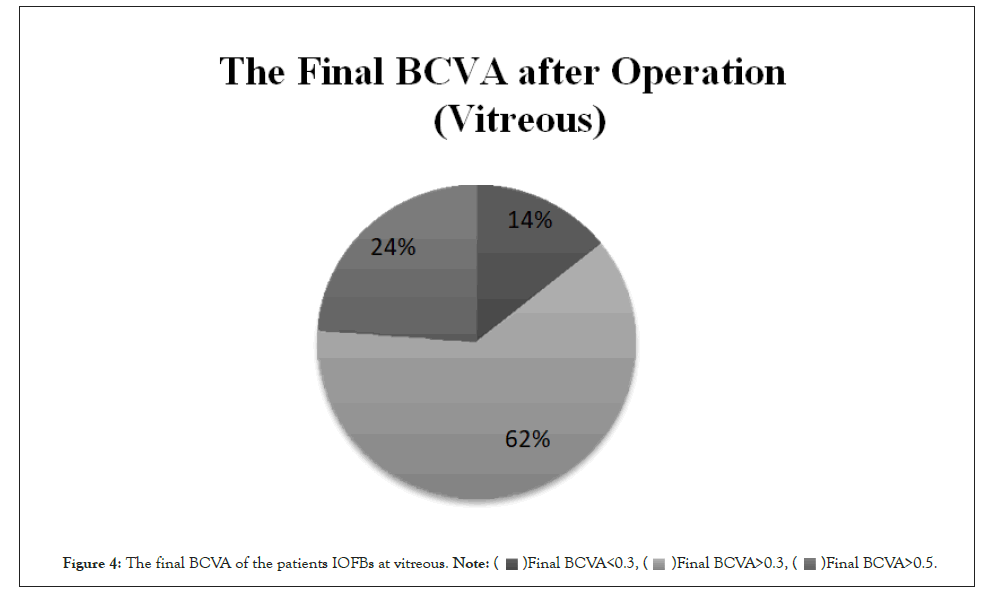
Figure 4: The final BCVA of the patients IOFBs at vitreous.
The best corrected visual acuity can be improved by the onestep removal of posterior segment intraocular foreign bodies via scleral tunnel incision procedure: only 25% of these patients can achieve the final BCVA around 0.3 whose IOFBs at the retina (Figure 5).
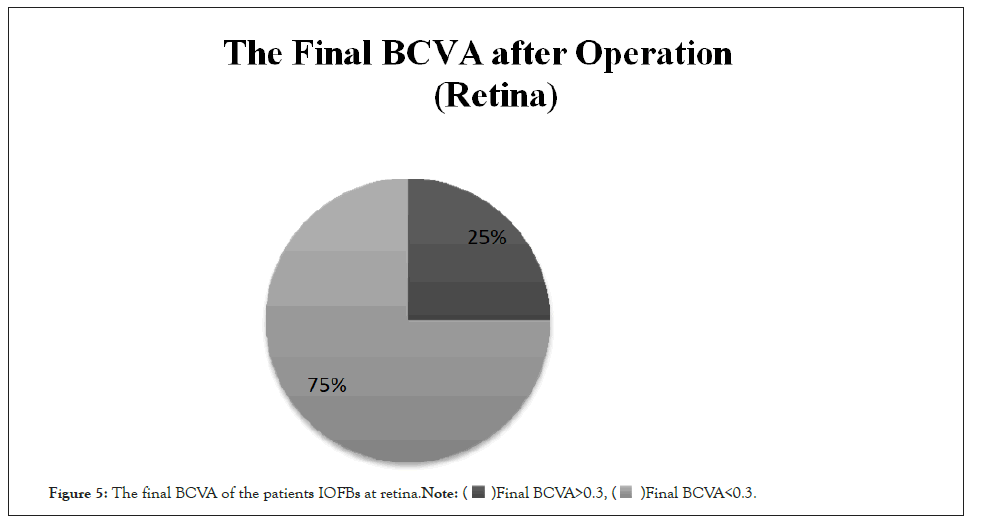
Figure 5: The final BCVA of the patients IOFBs at retina.
Statistical analysis
The majority of variables did not have a normal distribution, thus nonparametric tests were adopted. The clinical BCVA and visual improvement rate were compared with the Analysis of Variance (ANOVA) and for categorical variables using paired t-test. Statistical analyses were performed using SPSS for Windows (version 21.0; SPSS Inc, Chicago, IL, USA). A p values less than 0.05 was considered statistical significant.
The prevalence of IOFBs
The high percentage (35%–54%) of IOFBs is identified as arising from work-related injuries, and the incidence is higher in economical underdeveloped regions [9,10]. In our study, patients were predominantly male, and the younger and middle-aged people were more fragile. The peak age of patients was consistent with these literatures [11,12] that is, young to middle-aged popular.
The most important factor for IOFBs removal is the precious surgery on the timely therapy [13]. Once the foreign body in the eyeball is diagnosed, it should be removed in no time, especial metal tissue [14] otherwise there may be serious complaints such as endophthalmitis, rust, and retinal detachment.
The surgery strategy
If the corneal injury is critical, the first-stage corneal debridement and suture can be performed well-timed. After the corneal edema has been ameliorated with the intraocular hemorrhage stabilization, the second-stage IOFBs can be removed; if the corneal wound is small-size, without affecting intraocular micromanipulation, it is feasible to remove the IOFBs in one step, including corneal debridement suture, cataract extraction and vitrectomy.
In our series, 19 patients underwent second-stage vitrectomy 5 to 7 days after injury to demolish foreign bodies. At this time, the corneal wounds were not easy to leak, and part of them became transparent, which is safer for the surgery [15]. Eleven of the patients in this group underwent one-stage combined surgery to remove intraocular foreign bodies, traumatic cataracts, and associated vitreous successfully. The optional removal of foreign bodies in the first stage of combined surgery is helpful to reduce the occurrence of complications such as endophthalmitis, but there are also difficulties in clearing vitreous hemorrhage and making the absolute posterior vitreous detachment. Yu, et al. [16] reported that the second-stage surgery performed 8 to 14 days after injury is the rational choice. At this time, the corneal wound would heal to prevent leakage, the intraocular inflammation tend to be stable, the surgical operation is relative easier, and there were few surgery-associated complications [15,16]. Otherwise, Guevara-Villarreal, et al. [17] reported that as the interval between trauma and vitrectomy is postpone, which may lead to the occurrence of severe PVR.
The innovations of our clinical trails
Consider the position, quality and size of the foreign body in the cavity, an intelligent surgical method should be taken to remove the posterior segment IOFBs. For the foreign bodies in the posterior segment of the eye, the widely accepted method is vitrectomy [18]. The currently prevalence 23-gauge minimally invasive vitrectomy surgery is an upgraded version on the formal 20 G vitrectomy [19,20].
The advantage is that the incision is smaller and the surgery time is shorter which reduce the intricacy of vitreous incarceration caused by scleral puncture [21]. However, for the larger foreign bodies in the posterior fragment of the eye, it is validity to expand the ports from the anterior chamber transparence corneal incision to remove the foreign matter compare to the traditional 20 G incision [22]. The scleral flaring is prone to choroid damage, vitreous prolapsed, vitreous haemorrhage, retinal hole, sawtooth edge fragment and retinal detachment [22-25]. Ung, et al. [8] reported that removal of IOFBs is a challenging as IOFBs can be frequently dropped on the macula, causing iatrogenic retinal breaks. In this group of cases, a 12-point transparence cornealscleral tunnel incision was used for cataract extraction, and a foreign body was inserted through the sealous tunnel incision and the forceps were inserted through the anterior chamber to the vitreous cavity. This ports as minimum as possible, thereby reducing the iatrogenic damage to the posterior segment of the eye during foreign body eradication.
All cases in this group underwent integrated vitrectomy, which removed the vitreous base and the flats of the ciliary body to lessen the incidence of postoperative PVR and improve the success rate of the salvage procedure; especial for those with endophthalmitis, the microorganisms and toxicity material should be removed entirely. There were no needs to enlarge the incision. Our data shows that the final BCVA has sharp relation with the position of IOFBs with distance to the retinal or macular, the far away the better, the final BCVA data more than 0.3 (interval 62%-75%) or 0.5 (interval 25%-75%).
The ambiguous of an oculist’s surgery determination
The method of removal of the posterior segment IOFBs via scleral tunnel incision has its traits. The advantage is that it can avoid the risks of low intraocular pressure, vitreous hemorrhage, intravitreal incarceration, and postoperative retinal detachment due to enlarged scleral [26]. The disadvantage is that it is only suitable for patients with traumatic cataract, and the removal of the posterior segment IOFBs through the scleral tunnel incision may sabotage or sacrifice the integrity of the lens capsule [27].
According to the condition of traumatic cataract to select the treatment method, we can use cataract phacoemulsification or 23-gauge vitrectomy for lens. Try to keep the anterior capsule around the lens and remove the circular posterior capsule with a diameter of about 4.5 mm to facilitate the implementation of the IOL. In this group of cases, 25 (83.33%) eyes had to be taken the second-stage IOL implantation, of which 23 (76.66%) eyes received IOL implantation into the ciliary sulcus, and 2 (6.67%) eyes treat with IOL suspension. The final visual acuity has been improved by 25 (83.33%) eyes. There were no complications of scleral puncture.
The useful suggestions for IOFBs
The experience of traumatic cataract extraction through scleral tunnel incision and one-step removal of foreign bodies in the posterior segment of eye:
Safety: According to the status of the foreign body, make a self-closing scleral tunnel incision 1 mm behind the limbus in advance. All the key procedure and affiliated tips are done at the sealed anterior chamber that the natural protective layer benefits for the stability of intraocular chamber to avoid the most severity complication such as expulsive suprachoroidal hemorrhage [28]. Meanwhile, the surgery pouch be avoid of the conjunctive and scleral as minimums as possible which makes the least complications such as scleral staphyloma, delayed endophthalmitis [29].
Validity: For the anterior and posterior capsule ruptured lens, the anterior and posterior capsule can be bitten out by the detailed vitreous head, which do help for the precise micromanipulations at the vertical plane of optical axis and the peripheral anterior capsule should be kept as intact as possible to be feasible for the second-stage IOL implantation which are indispensable for the visual function recovery [30].
Economic: According to the situation of IOFBs, more than 18 (60%) cases were undertaken the first-stage IOL implantation that the visual functions of them can be saved at once, these exertions and benefits to the patients will be statements as the shorter-time hospitalization and less economic burden.
Replicate and short-time smooth learning curve: Although these mini micromanipulations contain both the phacoemulsification and PPV techs, the cumbersome posterior segments trail just as the additional. If the ophthalmologist have mastered the essentials of anterior parts will be reliable to master this mini porch skill.
The limitations of this study: Nevertheless, due to the small number of cases in this study and the terminated follow-up, it is not fundament to conduct the reliability of the conclusion. It may be necessary to collect more cases and prospective clinical case-control study with a longer-term follow-up.
In summary, traumatic cataract extraction, 23-gauge PPV, and one-step removal of posterior segment IOFB through a scleral tunnel incision are feasible and effective strategies in the treatment of posterior segment IOFBs combined with traumatic cataract. During the operation, it is not easy for foreign bodies to fall off and damage the retina, reduce the complications caused by the sclera puncture hole and expansion, and facilitate the secondary IOL implantation into the ciliary sulcus. Scleral tunnel incision has the advantages of incision well-closed and well-designed astigmatism, which helps to the recovery of BCVA.
Fundings
The present study was sponsored by Chenzhou Science and Technology Bureau Fund (grant.No.ZDYF-20200092); the hospital management fund by University of South China (grant. No.2019YJGL04) ;the Outstanding Youth Fund of the First People’s Hospital of Chenzhou City (grant.No.N2019-006).
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors’ contributions
Zhiyuan Li participated in the project design, sample size calculation and revision of the manuscript. Lilian Xie, Jundong Zhu was responsible for the enrolment and follow-up of patients. Yuyu Xie, Haiyan Wang performed the clinic treatment and participated in performing the statistical analysis. All the authors confirm the authenticity of the raw data and read and approved the final manuscript.
Patient consent for publication
Oral consent from the patient whose eye ball trauma with IFOBs at the posterior segment of ocular was obtained prior to publication.
Competing interests
The authors declare that they have no competing interests.
Acknowledgements
We thank the participants of the study. The authors acknowledge the guidance and support provided by Prof. Xiaohe Lu from the Ophthalmology Department, Zhujiang Hosptial of Southern Medical University.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Zhu J, Wang H, Xie L, Xie Y, Li Z (2022) The Reliability of Anterior-Posterior Segment Integrative Surgery via Sclera Tunnel Incision to Intraocular Foreign Bodies. J Clin Exp Ophthalmol. 13:920.
Received: 04-Apr-2022, Manuscript No. JCEO-22-15707; Editor assigned: 06-Apr-2022, Pre QC No. JCEO-22-15707 (PQ); Reviewed: 20-Apr-2022, QC No. JCEO-22-15707; Revised: 26-Apr-2022, Manuscript No. JCEO-22-15707 (R); Published: 05-May-2022 , DOI: 10.35248/2155-9570.22.13.920
Copyright: © 2022 Zhu J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.