Fungal Genomics & Biology
Open Access
ISSN: 2165-8056
ISSN: 2165-8056
Short Communication - (2021)Volume 11, Issue 4
Fungus is an abundant group of Eukaryotes which are cosmopolitan and inconspicuous as well. But it's intolerable to experience the consequences of harmful or dangerous fungus. The prevailing chronic infection Mucormycosis commonly termed as Black Fungus. Mucormycosis is a ubiquitous infection which is rare and fatal. It is caused by fungal pathogens. By knowing about their environmental niche, one can clearly understand the pathology of these fungi that are considered to be the causative agents of Mycosis.
Mucormycosis; Fungal pathogens; Black fungus; Fungi
Mycoses (singular: mycosis) are basically classified into three categories based on the factor influencing the site of infection. They are: A. Superficial mycoses B. Systemic mycoses and C. Opportunistic mycoses. Where, superficial mycoses are further classified as cutaneous and subcutaneous mycoses. Mucormycosis belongs to the classification opportunistic Mycoses.
Opportunistic mycoses
This type of mycoses is caused by fungal pathogens which are less virulent in nature. These causative agents are found to be normal endogenous commensals but when host’s immune system is triggered or altered, they become pathogenic.
Patients who are likely to get infected are the ones, who develop immune-compromised or immunosuppressed malignancies. It is also believed that the patients who are exposed to radiotherapy or cancer patients were also susceptible to this type of mycoses [1-11].
Taxonomical rank of the most common causative agent Mucor
• Kingdom: Fungi
• Phylum: Glomerulomycota
• Sub phylum: Mucoromycotina
• Class: Zygomycetes
• Order: Mucorales
• Family: Mucoraceae
• Genus: Mucor
The other commonly seen species under the order Mucorales are Rhizopus, Absidia, Lichtheimia, Apophysomyces, Saksenaea, Cunninghamella, Syncephalastrum, Rhizomucor etc.
Iron plays a vital role in growth of the microbial pathogens. Therefore, the causative agents of mycoses require iron as one of their growth factors. This means that increase in iron load increases the effect of invasiveness of mucormycosis. Few predisposing factors of mucormycosis are:
• Final stage of urinary organ illness
• Patients undergoing iron medical aid or deferoxamine (chelates iron)
• Defects in vegetative cell functions (Leukopenia/Neutropenia/ Lymphoma)
• The most significant threatening factor is Diabetic ketoacidosis (DKA). Because during the condition of acidosis, the sequestered proteins present in body fluid releases iron.
Few other risk ailments of mucormycosis are:
• Debilitating disease
• Corticosteroid treatment
• Diabetes mellitus
• Hematological malignancies
• Severe burn and Dialysis.
Rhinocerebral mucormycosis
It is the first commonly found variety of Mucormycosis. By inhaling the fungal spores, infection develops at the site of nasal cavity. Due to the incursive nature of sporangiospores, the infection spreads to all other tissues surrounding the paranasal sinus. Symptoms include facial pain, muzzy vision, periorbital cellulities, edema in eyelids, proptosis of eyes etc. Patients who are prone to hematological malignancies, organ transplant are more susceptible to this infection.
Pulmonary mucormycosis
It is the second commonly found variation of Mucormycosis. Invasion of lungs and surrounding organs can be witnessed. Symptoms may include lesion in trachea, rise in body temperature, ischemic necrosis, clogging of thick mucus and obstruction of airways which may result in lung collapse or invasion of parenchyma surrounding the lungs. Patients who are exposed to Hematopoietic stem-cell transplantation, chemotherapy and lower neutrophil count are susceptible to this infection.
Cutaneous mucormycosis
Infection occurs by direct infusion of fungal spores on the dermis. Capable of invading bones and muscles (disseminated condition). Hyperemia, redness in skin, necrotic eschar and skin indurations are the commonly seen symptoms.
Gastrointestinal mucormycosis
It is rare and inheritable. Intake of pathogen occurs via food intake such as brewed milk, fermented meal, dried bread, contaminated food products etc. Parts of small and large intestine like ileum; caecum, spleen, liver, bowel walls and pancreas are the areas where infection usually occurs at. This type of Mucormycosis is basically found in premature neonates (Necrotizing enterocolitis), undernourished children and diabetic patients.
Disseminated mucormycosis
This type of Mycosis occurs by hematogenic spread of infection from one organ to another organ. The spread of infection is more common in brain followed by evolution of lesions in organs like spleen, heart, liver etc. Patients exposed to high iron load (deferoxamine), undergoing leukemia or undertaking steroids are more vulnerable to this type of Mucormycosis (Figure 1).
Figure 1: Common clinical variations of mucormycosis.
Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scan are taken to visualize images of infectious regions like lungs, sinus etc. 10% KOH wet mount preparation is done to detect the fungal elements like spores, hyphae etc (exudation). Diagnosis is done by examination of the sample-affected tissue (Histological examination) from which, the characteristic features of the fungal culture is clearly visualized under microscope. Grocott-Gomori's Methenamine Silver Staining is done for the clear view of fungal hyphae. Molecular identification is done by PCR amplification and sequencing in which the DNA of the Mucorales is detected (Table1).
| Species | Mucor | Rhizopus | Absidia |
|---|---|---|---|
| Septum | Non-septate mycelium | Non-septate mycelium | Sparsely septate |
| Rhizoids | Absent | Present (nodal) | Present (internodal) |
| Sporangiophore structure | Branched | Unbranched | Branched |
| Columella shape | Globose or spherical shape | Ovoid shape | Pear shape |
Table 1: Characteristics of commonly found mucorales.
Effective treatment/medication for one such fungal infection is rendered by a panel of experts in Microbiology, Ophthalmology, Neurology and other fields related to medicine. Identification of the infection at early stages and administration of antifungal elements may reduce the risk of infection. In few cases, the infected tissue is removed surgically to prevent the further spread of fungus. Medicating the underlying medical issues may also help in treatment. The most commonly used antimycotic medication is Amphotericin B (Figure 2).
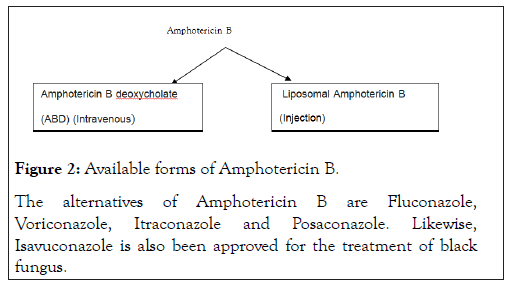
Figure 2:Available forms of Amphotericin B.
The alternatives of Amphotericin B are Fluconazole,Voriconazole, Itraconazole and Posaconazole. Likewise,Isavuconazole is also been approved for the treatment of black fungus.
Mucormycosis is an uncommon infection, but it is emerging along with COVID-19 with high fatality rate. According to the Epidemic Diseases Act 1897 it is considered to be notifiable disease. Black fungus was also pronounced to some period of time during SARS outbreak. It is stated that in order to develop exaggerated inflammatory response against COVID-19, people tend to use cheap steroids which might increase the vulnerability of secondary infections like Mucormycosis and few other respiratory disorders. Therefore uncontrolled diabetes mellitus accompanied with COVID-19 may result in Mucormycosis. Since it is considered as a life-threatening disease, one should avoid direct contact with soil or dust and also minimize the chances of developing skin injuries.
Citation: Tejeswini. The Black Fungus: A Short Review. Fungal Genom Biol. 11:172.
Received: 18-Aug-2021 Accepted: 01-Sep-2021 Published: 08-Sep-2021 , DOI: 10.35248/2165-8056.21.11.173
Copyright: © Tejeswini .This is an open-access ar ticle dis tribut ed under the t erms of the Cr eativ e Commons A ttribution License, whic h permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.