
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2021)Volume 11, Issue 4
Background: This study aims to examine the influence of BCG status and TB prevalence on variances among countries regarding the new Multisystem Inflammatory Syndrome in Children (MIS-C).
Material and methods: We chose all countries which report MIS-C till 23/6/2020. The number of MIS-C cases for each 10 million inhabitants has been examined among 3 categories of countries classified according to BCG program status. TB prevalence, MIS-C no./10 million (M) population and COVID-19 deaths/M are taken as markers. Receiver Operation Characteristic-(ROC) curve, with some relative indicators such as (sensitivity and specificity rates), estimation area of the trade-off between sensitivity and specificity, and cutoff points were used with different studied markers for discriminating different three pairs of countries (which have different BCG practices).
Results: BCG vaccination and high TB prevalence were found significantly associated with decreased MIS-C no. and COVID-19 deaths.
Conclusion: Findings might explain variances of MIS-C incidence and COVID-19 mortality among countries worldwide. Further studies to confirm this relationship and to confirm possible similar relations in Kawasaki Disease (KD) in previous epidemics are recommended. Ovarian Cancer (EOC) in early stage is difficult to diagnose. Serum indicators for stage I-II of epithelial ovarian cancer which confined to pelvic cavity were found through retrospective analysis, possible early detection methods might be found.
Methods: 165 patients were diagnosed as epithelial ovarian cancer at stage I-II from January 1st, 2015 to December 31st, 2019. Data was collected including age, pathological type, serum D-dimer (D-D), Neutrophil to Lymphocyte ratio (N/L), the platelet to Lymphocyte ratio (P/L), Cancer Antigen 125 (CA125), Human Epididymis Protein 4 (HE4) and diameter of the ovarian mass by ultrasound.
Results: D-D, CA125, HE4, ROMA, diameter, pathological type and age were significantly different in the different stage, age showed independent effect after logistical regression (P<0.05). D-D, CA125, HE4, ROMA, diameter, age and stage were significantly different in the different pathological type, and diameter showed significant independent influence on different pathological type after binary logistic regression (P<0.05).
Conclusion: CA125, HE4, ROMA, diameter of tumor, D-dimer and age were found significantly different between stage I and stage II, with age shows good effect on the diagnosis for stage II and diameter of tumor shows diagnostic value for non-serous ovarian cancer. Combined diagnosis may improve the diagnosis rate of early ovarian cancer.
COVID-19; SARS-CoV-2; Kawasaki disease; Toxic shock syndrome; SARS-CoV-2; Severe acute respiratory syndrome coronavirus
During April 2020, reports emerged from the United Kingdom of presentations in children similar to incomplete Kawasaki Disease (KD) or Toxic Shock Syndrome (TSS) [1]. In Italy, approximately 10 suspected Kawasaki-like disease cases have been recorded since 1st January 2020, eight of which were reclassified as new pediatric inflammatory multisystem syndrome temporally associated with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection in children (PIMS-TS) or Multisystem Inflammatory Syndrome in Children (MIS-C) or pediatric hyperinflammatory syndrome or pediatric hyperinflammatory shock which is a hyperinflammatory syndrome with multiorgan involvement have some features similar to those of Kawasaki disease and TSS [2]. MIS-C cases have also been reported since then in USA and countries in Europe. Classical KD with concurrent COVID-19 also has been reported [3].
The case definition of MIS-C was regarded by some experts as quite broad and overlaps with Kawasaki disease [4]. On the contrary, other experts are concerned that current diagnostic criteria may not capture the true scope of the problem [5]. Furthermore, cross immune heterogeneity was suggested between BCG and certain viral diseases since BCG induces trained immunity through expressing heterologous antigens of different pathogens which have been developed and tested since 1991 [6]. Different studies have already shown statistical associations of BCG vaccinations and TB prevalence status with reduced severity of COVID-19 disease [7-10]. These studies suggest that BCG and natural latent TB infection induce heterogeneous immunity against SARS-CoV2.
Studies are lacking regarding a possible role of BCG or possible latent TB protective effects on the incidence of MIS-C or KD including KDSS.
This study is the first in the aspect of looking for MIS-C incidence relation to TB prevalence status in different countries classified according to BCG vaccination status and will address a possible cause of disparities raised regarding variances in the incidence of MIS-C and COVID-19 deaths rates among countries. Furthermore, we also discuss the possible relation of KD with previous pandemics according to various TB prevalence and BCG status of some countries.
Materials
It was not appropriate or possible to involve patients or the public in this work given that we used general practice level summated data and related publically published morbidity and mortality statistics. Patients were not involved.
Data regarding MIS-C cases collected till 23/6/2020. Cases outside this date are not included. The total number of countries was 15 countries. 13 countries were listed by European Centre for Disease Prevention and Control (ECDC) rapid risk assessment report on May 15, 2020 as the only countries in the world which have been reported MIS-C cases, both Russia and Peru reported MIS-C cases on June 17 and June 22 respectively were included in the study. These data are publically available. List of references for this data is included in the supplementary file.
We checked Google for any possible cases up to 23/6/2020. We look for any data, whether population-based, cross-sectional studies, surveillances, and news. The check included all countries across the world besides checking already included 15 countries for any extra reported or missed cases. We checked also: PubMed and Wikipedia.
We consider COVID-19 deaths/million (M) as it is in 2/7/2020 considering a lag time of 10 days between the day of case report and death. COVID-19 mortality, data TB prevalence data, and population data were obtained from publically published data. BCG data were obtained from publically available WHO data and various references. The attached appendices show further details and further references for all data. Total countries were 15 (Table 1). We put studied countries into three different groups.
| Group's combination | Parameters | Area | Std. Error | Asymp. Sig. |
Asymp. 95% C.I. | |
|---|---|---|---|---|---|---|
| IXII | MIS cases/10 M pop. | 0.583 | 0.175 | 0.683 | 0.241 | 0.926 |
| COVID-19 deaths/M. | 0.417 | 0.173 | 0.683 | 0.078 | 0.755 | |
| TB prevalence | 0.833 | 0.133 | 0.102 | 0.572 | 1.094 | |
| IXIII | MIS cases/10 M pop. | 0 | 0 | 0.034 | 0 | 0 |
| COVID-19 deaths/M. | 0.083 | 0.115 | 0.077 | 0 | 0.309 | |
| TB Prevalence | 0.833 | 0.17 | 0.157 | 0.5 | 1.167 | |
| IIXIII | MIS cases/10 M pop. | 0.094 | 0.095 | 0.027 | 0 | 0.28 |
| COVID-19 Deaths/M. | 0.188 | 0.135 | 0.089 | 0 | 0.452 | |
| TB Prevalence | 0.75 | 0.217 | 0.174 | 0.326 | 1.174 | |
Note: (*) S: Significant at P<0.05; NS: Non Significant at P>0.05, informative reportable p value>0.05 if close to (but does not reach) 0.05 and confirmed by minimum confidence interval (Robert J. Nordness, "Epidemiology and Biostatistics Secrets", MOSBY ELSEVIER, 1600 John F. Kennedy Boulevard, Suite 1800 Philadelphia, PA 19103-2899, P156, 2006); I: No vaccinated at all; II: No currently vaccinated; III: Currently giving vaccination; Asymp: Asymptotic values; Sig: Significant.
Table 1: Relationships among a diseased groups and controlled for all probable combinations of disclusion time test in different parameters.
No vaccination at all and no previous BCG group: USA, Canada, and Italy.
No current vaccination but with previous BCG program Group (countries which ceased BCG vaccinations previously): 9 countries: Austria, France, Germany, Luxembourg, Spain, Sweden, Switzerland, and United Kingdom.
Currently giving mass BCG vaccine group: Greece, Portugal, Peru, and the Russian Federation.
Receiver Operation Characteristic (ROC) curve, as well as some relative indicators such as (sensitivity and specificity rates), and cutoff points, were used for discriminating different three categories of countries (which have different BCG practices). Discrimination of these categories done through studied markers. All statistical operations were performed using the ready-made statistical package SPSS, ver.22.
Attached supplementary file contains collected data for the study sample in terms of a country no. of MIS-C cases, BCG status, COVID-19 deaths, and TB prevalence and various sources for data collection. Patient and public involvement statement.
Group 1 (countries with no vaccination at all and no previous BCG national programs) showed the highest mean value for COVID-19 deaths/M inhabitant and lowest TB prevalence.
Group 2 No current vaccination (previous vaccination) group showed the highest MIS-C, while other parameters were in between.
Group 3 (countries currently giving BCG vaccine) showed lowest MIS-C no./10 M, lowest COVID-19 mortality, and highest TB prevalence.
Table 1 and Figure 1 show ROC analyses with the estimated area of the trade-off between sensitivity and specificity of markers through plotting sensitivity against a complement specificity outcome. Table 1 also shows a significant level for the testing area under the guideline of fifty percent, with a 95% confidence interval of all probable combinations of pairs of countries and were as follows.
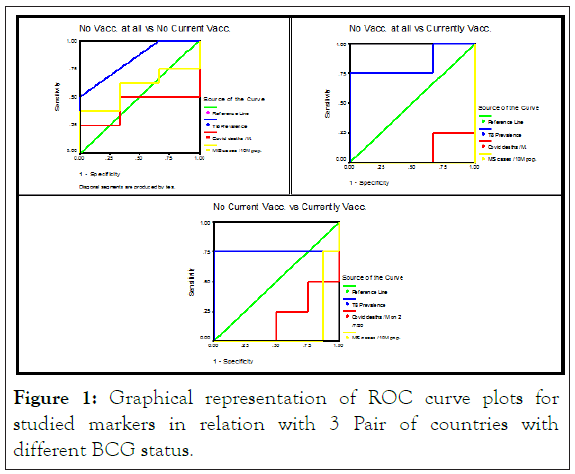
Figure 1: Graphical representation of ROC curve plots for studied markers in relation with 3 Pair of countries with different BCG status.
Pair of countries with no vaccination program at all (x-axis) and no current vaccination program but have previous vaccination program (y-axis).
The common thing in this pair is that both groups had no vaccination programs at this time whether had a previous history of vaccinations or not.
Pair of countries with never gave BCG vaccination program (x-axis) and those with currently giving BCG vaccination (y-axis).
Pair of countries with currently no vaccination (ceased vaccination program) (x-axis) and currently vaccinated (y-axis). The common thing in this pair is having BCG vaccination, whether in the past or at the current time.
Findings
MIS-C no./10 M inhabitants in countries which did never give BCG vaccination vs. countries currently giving vaccine (pair 2) showed area under ROC-curve equal to 0.000 with a symbiotic significant of 0.000 and (95% CI interval of 0.000-0.000) also MIS-C No/10 M inhabitants in countries not currently give BCG vaccination (ceased mass vaccination programs) vs. countries currently give mass vaccination (pair 3) showed area under ROC-curve equal to 0.094 with a symbiotic significant of 0.027 and (95% CI interval of 0.000-0.280).
Important not significant finding is that MIS-C no./10 M inhabitants in countries which had never give BCG vaccination vs. countries not currently giving vaccine (1st pair) showed area under ROC-curve equal to 0.583 with a symbiotic significant of 0.683 and (95% CI interval of 0.074-0.759).
MIS-C no. is a good discriminator in a significant association when countries not currently giving vaccine are in the 3d pair of countries (i.e. with countries currently given BCG vaccine) and not in 1st pair (i.e. with countries did never give national BCG vaccination).
COVID-19 deaths/M inhabitants in countries which had never give BCG vaccination vs. countries currently giving vaccine (pair 2) showed area under ROC-curve equal to 0.083 with a symbiotic informative and reportable value of 0.077 and (95% CI interval of 0.000-0.309 also COVID-19 deaths/M inhabitants in countries not currently giving BCG vaccination vs. countries currently giving vaccine (3d pair) showed area under ROC-curve equal to 0.188 with a symbiotic informative reportable value of 0.089 and (95% CI interval of 0.000-0.452).
Important finding was the non-significant association of COVID-19 deaths no./M inhabitants in countries which had never give BCG vaccination vs. countries do not currently give vaccine (1st pair) which showed area under ROC-curve equal to 0.417 with a symbiotic significant of 0.683 and (95% CI interval of 0.078-0.755).
COVID-19 deaths parameter is a good discriminator in a significant association when countries not currently give vaccine are in third pair of countries (i.e. with countries currently given vaccine) and not in 1st pair (i.e. with countries did never give BCG vaccine in their national programs).
Regarding TB prevalence marker or discriminator the areas under curve were informative and reportable and too generating with the leftover markers in all pairs and were 0.833 with 59% CI of 0.572-0.755 in pair one and 0.833 with 95% CI interval of 0.5-0.500 and 0.750 with 95% CI interval of 0.326-1.174 in pairs 2 and 3 respectively. These signifying inverse relations with COVID-19 mortality and MIS-C no. The informative reportable asymptotic values were 0.102, 0.157 and 0.174 for 3 pairs respectively. In Figure 1 TB prevalence marker or discriminator looks to be too generating with the leftover markers in all 3 pairs.
We suggest that TB and/or BCG might have a role in trained immunity modulation as back ground hypothesis for this study.
Limitations of this study include but are not limited to the following. Overlap case definition with Kawasaki disease, retrograde classification of cases, underreporting, under registration, limited no. of countries reported the disease up to 13/6/2020 and a limited number of reported cases. Furthermore, this study is done at an early time of the emergence of this new disease with the existence of continuous reporting of new cases from different countries in the view of increased awareness of the disease. Furthermore, there was no agreed international nor EU case definition for MIS-C neither specific diagnostic code during the study period making the impact of the new syndrome more difficult to be fully assessed.
The statistical negative association between MIS-C and BCG was highly significant between countries that give BCG vaccination versus those not given BCG vaccine. This is a statistical association and not necessarily means causation, although a direct beneficial effect to BCG vaccination is suggested. The suggested mode of protection that might explain this association in countries that continue BCG vaccinations is through accumulative herd immunity. Countries that ceased BCG vaccinations were also suggested to have such immunity to a certain degree. On the other hand, those with no BCG vaccination are the worst among the 3 groups. This negative association was also found between BCG practicing and COVID-19 deaths. In a similar suggestive mode to BCG, TB prevalence (which reflects latent TB status) showed a less significant but informative and reportable association and too generating with the leftover markers. Our findings consolidate literature that suggests an influence of BCG and TB prevalence status in lowering COVID-19 mortality.
In Europe, although the incidence of KD is lower than Asian countries the (KDSS) has a higher incidence in these countries, compared with Asian countries, the real cause for the high incidence of KDSS in western countries is unknown yet. Possibly the decreased prevalence of latent TB which is suggested to cause decreased training for innate immunity essential for response to variety of infections. Lack of BCG vaccination in some countries might add to TB influence on the same way.
The temporal associations of MIS-C emergence in different countries in this pandemic with associated of lack of BCG and low TB prevalence is of major concern.
Relation of KD emergence and outbreaks might be related to concomitant previous new strains emergence and outbreaks.
Controlled clinical trials are required for confirmation of causation of TB prevalence and BCG status to MIS-C or Kawasaki like a spectrum of diseases in general.
I am deeply grateful to Emeritus Professor Abdulkhaleq Abduljabbar Ali Ghalib Al-Naqeeb, Ph.D. in the Philosophy of Statistical Sciences at the Medical & Health Technology College, Baghdad-Iraq, for his assistance and support in data analysis and interpretation of results.
Citation: Raham TF (2021) TB prevalence and BCG Vaccinations Correlation to Multisystem Inflammatory Syndrome in Children. J Clin Trials. 11:465.
Received: 20-Apr-2021 Accepted: 04-May-2021 Published: 11-May-2021 , DOI: 10.35248/2167-0870.21.11.465
Copyright: © 2021 Raham TF. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.