Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2022)Volume 13, Issue 3
Purpose: To report a case of non-pulmonary sarcoidosis involving cornea and cranial nerve VIII
Case: A 25-year-old lady initially presented with flu-like symptoms, erythema nodosum and polyarthritis of minor joints. She later developed abdominal lymphadenopathy and splenomegaly. Spleen biopsy revealed granulomatous inflammation. There was a chronic ocular inflammation due to interstitial keratitis, which responded partially to topical corticosteroid and tacrolimus. Corneal infiltrations healed with the aid of immunomodulatory agents. Later, she developed neurosensory hearing loss due to inflammation of Cranial Nerve (CN) VIII. All her symptoms except neurosarcoidosis has improved with systemic azathioprine, and then oral methotrexate and subcutaneous anti TNF alpha.
Conclusion: Interstitial keratitis and involvement of CN VIII are rare manifestations of sarcoidosis. This clinical picture resembles Cogan's syndrome. Ocular manifestations of a systemic autoimmune disease are best managed by appropriate immunodulatory therapy.
Systemic sarcoidosis; Cogan's syndrome; Interstitial keratitis; Cranial nerve VIII involvement
Sarcoidosis is a chronic multisystemic inflammatory disease characterized by non-caseating granuloma. It commonly involves the lung, lymph nodes, skin, musculoskeletal system and with less frequency eyes, liver, heart and brain [1]. Ocular involvement occurs in 25% of cases [2]. Protean manifestations of ocular sarcoidosis come from granuloma formation in orbit, conjunctiva, choroid, optic nerve and sclera. The most common ocular manifestation is uveitis, reported in 30%-70% of cases with eye involvement. Corneal involvement has been rarely reported in the form of interstitial keratitis, peripheral ulcerative keratitis, superficial punctate keratitis, calcific band keratopathy, keratoconjunctivitis sicca and exposure keratopathy [3]. Neurosarcoidosis can appear with other forms of sarcoidosis. It can present with cranial nerve involvement, which in descending order of frequency includes facial (VII), optic (II), trigeminal (V) and vestibulocochlear (VIII) nerves [2, 4]. Cogan's syndrome is an inflammatory condition with unknown etiology hallmarked by interstitial keratitis and vestibuloauditory symptoms. Herein, we report a young lady with unusual manifestations of sarcoidosis mimicking Cogan's syndrome.
A 25-year-old lady was referred to an ophthalmology center due to red-eye. She mentioned a history of fever, night sweats, small joints polyarthritis and erythema nodosum six months prior to the presentation, which completely improved with low dose oral prednisone for several days and Non-Steroidal Anti- Inflammatory Drugs (NSAIDS). She mentioned a recent recurrence of arthralgia. Slit-lamp examination in both eyes showed a conjunctival injection and white-colored infiltration in the corneal stroma with feathery borders and deep stromal vascularization in the superior third of cornea of both eyes along with lipid deposition in between (Figure 1a-1b). There were cells of 1+ grade in anterior chamber. Retina and optic nerve examination were unremarkable. She had elevated levels of Erythrocyte Sedimentation Rate (ESR), C-reactive protein (CRP) and Lactate Dehydrogenase (LDH) and leukocytosis. The level of angiotensin converting enzyme (ACE) and liver function tests were within normal limits.
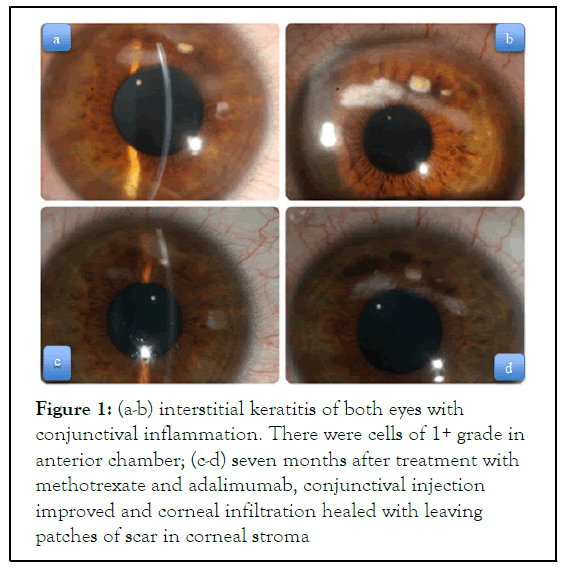
Figure 1: (a-b) interstitial keratitis of both eyes with conjunctival inflammation. There were cells of 1+ grade in anterior chamber; (c-d) seven months after treatment with methotrexate and adalimumab, conjunctival injection improved and corneal infiltration healed with leaving patches of scar in corneal stroma
Chest and abdominal CT scan revealed left pleural effusion and multiple small-sized (up to 7mm) paraaortic and abdominal lymphadenopathy (LAP), while no mediastinal LAP or parenchymal lesion was detected. There was no peripheral LAP as well. It is noteworthy that at the first bout of disease, all laboratory tests except ESR, which was 72 mm/hr, and chest CT scan, were unremarkable. In abdominal ultrasonography, she was found to have splenomegaly with multiple hypoechogeneic regions with a maximum diameter of 15 mm.
Biopsy of the spleen showed granulomatous inflammation. Polymerase Chain Reaction (PCR) of splenic tissue was negative for tuberculosis, as a result, sarcoidosis was put forward as the most probable diagnosis. Histopathologic review of the samples of abdominal lymph node was also in favor of an active granulomatous inflammation. She was suffering from a chronic eye inflammation, with no adequate response to topical corticosteroid and tacrolimus. She was started on a high dose oral prednisone (60 mg/d) with tapering. Oral cyclosporine failed due to hypertrichosis. Azathioprine (100 mg/day) commenced orally with improvement in ocular and systemic symptoms. One year later and four months after tapering off all medications, tinnitus and progressive neurosensory hearing loss in high pitched sounds were detected in audiogram. In addition, the keratitis flared. Brain MRI did not show any mass effect on cerebellopontine angle. This time, due to easier usage, oral methotrexate (17.5 mg/week) was started and four months later adalimumab (40 mg subQ every 2 weeks) was added due to residual inflammatory activity. All manifestations except hearing loss have been stabilized. Oral and local corticosteroids have been tapered off within three months, while the patient was continuing immunomodulatory therapy. The conjunctival injection and corneal infiltration completely resolved with remaining patches of stromal scar (Figures 1c and 1d). During the following two years, all the medications including methotrexate and adalimumab were tapered and the patient remained in remission.
A distinct feature of sarcoidosis is Lofgren's syndrome which presents in younger patients. It usually has an acute course and is characterized by erythema nodosum, bilateral hilar LAP, polyarthritis and fever [5,6]. Manifestation of disease in our patient was mostly compatible with the diagnosis of nonpulmonary sarcoidosis due to lack of hilar LAP and absence of pulmonary parenchymal lesion while eyes and CNS were involved [7-9]. This type of disease has been reported to comprise 5%-9% of patients with sarcoidosis [10]. In addition, our patient did not show a complete triad of Lofgren's syndrome and lacked the sign of bilateral hilar LAP.
Neurosarcoidosis involving CN VIII is a rare presentation. Irreversible audiovestibular dysfunction occurs as a result of vasculitis and subsequent ischemia of cranial nerve. This leads to a progressive neurosensory hearing loss which poorly responds to corticosteroids and other immunosuppressants. Our patient developed signs of CN VIII involvement after premature cessation of immunosuppressant medications. The hearing problem of our patient persisted despite treatment, while all other manifestations of disease such as LAP, arthritis, LDH level improved. Corneal involvement has been rarely reported in patients with sarcoidosis. Differential diagnosis of interstitial keratitis and inner ear problems can be divided into those with infectious or inflammatory etiology. Syphilis, herpes, mumps, TB, HTLV1, Lyme disease and chlamydia are infectious processes, while sarcoidosis, Cogan's syndrome, lupus erythematosus, granulomatous with polyangiitis, relapsing polychondritis, Behcet's disease, lymphoma and Whipple's disease are among inflammatory causes.
Cogan's syndrome is an idiopathic autoimmune disorder that affects young white adults. The presentation can be with fever, splenomegaly, LAP and musculoskeletal complaints. The hallmarks are interstitial keratitis and vestibuloauditory symptoms. Uveitis, scleritis, episcleritis, conjunctivitis are other possible ocular manifestations. Vasculitis can involve large, medium and possibly small vessels. Arthritis, rash and gastrointestinal bleeding have also been reported. No confirmatory test exists for this disease [11]. Cranial CT scan and MRI to evaluate pathology in the path of CN VIII are often normal, but they are necessary to rule out other causes, such as neoplasms and infections [12]. Erythema nodosum which was observed in our patient has not been reported among manifestations of Cogan's syndrome.
The diagnosis of sarcoidosis is mainly based on histopathologic detection of a non-caseating granuloma. However, this is not pathognomonic, and other granulomatous inflammations should be considered. Here, we reported a young lady with possible sarcoidosis with rare manifestations of interstitial keratitis and neurosarcoidosis involving CN VIII. These features imitate Cogan's syndrome. If topical agents are not effective in controlling the ocular inflammation, especially those associated with a systemic autoimmune disease, sufficient systemic immunosuppressive medications should be employed.
The author's declare no conflict of interest
We have no funding for this research and no institutional open access funds available to cover costs of publication
The authors thank the patient for allowing the case to be published
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
Citation: Havashki E, Zarei-Ghanavati M, Kavosi H, Ebrahimi Z, Naybandi S, Ebrahimiadib N (2022) Systemic Sarcoidosis Mimicking Cogan's Syndrome: A case report. J Clin Exp Ophthalmol. 13:912.
Received: 10-Jan-2022, Manuscript No. JCEO-22-15433; Editor assigned: 12-Jan-2022, Pre QC No. JCEO-22-15433 (PQ); Reviewed: 26-Jan-2022, QC No. JCEO-22-15433; Revised: 31-Jan-2022, Manuscript No. JCEO-22-15433 (R); Published: 07-Feb-2022 , DOI: 10.35248/2155-9570.22.13.912
Copyright: © 2022 Havashki E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.