
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2021)
Background: FGM/C can lead to a number of health complications, such as pain during intercourse or childbirth, psychological problems, and postpartum complications. This study seeks to describe and assess Swedish healthcare for women subjected to FGM/C.
Methods: This aim encompasses three research foci: (1) to inventory Swedish regional healthcare guidelines and policies for care for women who have undergone FGM/C, (2) to map healthcare consumption among women who have undergone FGM/C, and (3) to map the type of care measures and treatment they have been offered in the Swedish healthcare system. A questionnaire was sent to healthcare regional managers and a database study was conducted.
Results: The inventory of the healthcare regions' guidelines shows that five of 21 had no guidelines. The number of women who have been subjected to FGM/C and sought care has increased steadily between 2012 and 2018. Women who have been subjected to FGM/C seek care mostly in connection with pregnancy and childbirth.
Conclusion: The types of care that should be offered to women who have been subjected to FGM/C vary depending on individual needs. Care may include surgical procedures in the form of defibulation, clitoral reconstruction, or removal of cysts, as well as psychosexual care. Existing treatment options in surgical care, together with psychosexual treatment, are the care measures that seem to be helpful for some women who have undergone FGM/C, but not for all. Communication and treatment are of great importance in order to be able to offer care to women who have undergone FGM/C.
FGM/C; Healthcare; Diagnose code; Guidelines; Care seeking
FGM/C: Female Genital Mutilation/Cutting.
The fifth goal of Agenda 2030 on gender equality and the elimination of all harmful practices against children calls for an end to female genital mutilation/cutting (FGM/C) [1]. Several intergovernmental organizations have promoted the abolition of FGM/C, including the African Union, the European Union, and the Organization of Islamic Cooperation. Three UN General Assembly resolutions have also addressed the matter [2]. Although FGM/C is illegal in all EU member states [3], it still occurs among some groups residing in those countries. In addition, some women and girls have been subjected to FGM/C in their country of origin [4]. Migration in recent decades has spread the practice of FGM has spread to European and other Western countries [5]. The European Parliament has estimated that 500,000 women have been subjected to FGM, and an additional 180,000 girls are at risk of being subjected to FGM [6] some argue even argue that this is an underestimate of the scope of the problem [7]. FGM/C can lead to a number of health complications, such as pain during intercourse or childbirth, psychological problems, and postpartum complications [8]. Clinical studies show that women who have undergone FGM/C are four times more likely to suffer from complications during childbirth [9]. According to UNICEF [10], FGM/C is a serious health problem for women and girls due to the medical risks of the procedure. FGM/C covers a variety of procedures, from a stitching/incision of the clitoris to full infibulation [11]. The health consequences are largely related to the way the practice is performed and the scope of the procedure [12,13]. Common complications associated with FGM/C can be grouped into three categories: Physical, sexual, and psychological. These complications include both immediate and long-term impacts, including complications during childbirth [14,15]. Female genital mutilation is one facet of violence against women, and its health consequences may be similar to those that affect victims of violence.
Immediate complications are those that occur within ten days after the procedure and include heavy bleeding, anemia, urinary tract infection, tetanus, sepsis, and shock. Long-term complications include abnormal scarring such as fibrosis or keloids, cysts or fistulas, recurrent urinary tract infections, difficulty emptying the bladder, painful intercourse, and infertility. Complications can also cause problems during childbirth [14] for example, infibulated women are at an increased risk of anal sphincter rupture during childbirth [15,16]. A study from six African countries shows that the risk of newborn perinatal death increases by 22 percent among women who have been subjected to FGM/C [17]. The psychosocial consequences of FGM/C are various [18-21]. Different studies have found varying rates of post-traumatic stress disorder (PTSD) and affective disorders such as anxiety and phobias, ranging from no incidence up to 58 percent in women who have undergone FGM/C. Previous studies from Sudan and Somalia show negative effects on self-esteem and self-identity in women subjected to FGM/C [20,21]. In recent years, and since the HIV/AIDS pandemic, an increased likelihood of HIV transmission has been added to the long list of complications associated with FGM/C. Traditional doctors who perform FGM/C may not be aware of the dangers of using unsterilized instruments or that bleeding during intercourse increases the risk of transmission [22]. The Swedish National Board of Health and Welfare [23] estimates that approximately 38,000 women and girls in Sweden may have undergone some form of genital mutilation in their countries of origin. Of these, an estimated 7,000 are under 18 years of age. Approximately 19,000 girls are part of the at-risk population. In Sweden, most women who have been subjected to FGM/C are originally from Somalia, Eritrea, Ethiopia, Egypt, or The Gambia [24].
This study aims to describe and assess Swedish healthcare for women who have undergone FGM/C. This aim encompasses three research foci: (1) to inventory Swedish regional healthcare guidelines and policies for care for women who have undergone FGM/C, (2) to map healthcare consumption among women who have undergone FGM/C, and (3) to map the type of care measures and treatment they have been offered in the Swedish healthcare system.
The study addressed these three foci using data from a self- administered electronic questionnaire addressed to regional healthcare coordinators and managers and from the Swedish Patient Register (PR) and Medical Birth Register (MBR) for the 2012-2018 period.
Inventory of regional healthcare guidelines and policies for the care of FGM/C
Study population: Sweden has a total of 21 healthcare regions (counties). All coordinators and managers in these counties participated in this study. Furthermore, the healthcare regions’ webpages were also reviewed to look for policies, guidelines, or written routines.
Data collection: A cross-sectional descriptive study was conducted based on a self-administered electronic questionnaire addressed to regional healthcare coordinators and managers. The main question was whether the healthcare region has any policies, guidelines, or written routines for measures or treatment offered to women who had undergone FGM/C. If the initial contact did not result in a reply, they were then contacted by telephone or e-mail a second time.
Data analysis: The participants’ answers were tabulated in an Excel file to arrive at an initial descriptive analysis. All documents from all regional webpages, as well as written routines, care programs, care guidelines, action plans, and care process programs were carefully read and analyzed for key features such as diagnostic codes, defibulation, mental health, sexual counseling, etc. The data received were divided into two main categories: regional (aimed at all healthcares in the region) and local (aimed at one or more special activities within the region).
Healthcare consumption among women who have undergone FGM/C and the type of care measures and treatment they were offered
Register: The PR was established in 1964 and has included nationwide information at the individual level on all completed inpatient care sessions since 1987 and specialized outpatient care visits since 2001. All private and public care providers within the specialized outpatient and inpatient care system are obligated to report information to the PR.
In addition to administrative information such as care facility, patients’ personal data, date of intake and discharge, and form of discharge, the database also reports the patient diagnosis associated with the care visit and the measures taken. All diagnoses with clinical relevance at the time of care must be reported using the codes in the International Statistical Classification of Diseases and Related Health Problems (ICD10). The treatment measures taken, such as surgery, are reported using a system of codes and classification of care measures. By combining the ICD10 diagnostic codes and the treatment codes, it is thus possible to see which diagnoses patients received cared for and what treatment they received during the time they were in care. The database also contains information on certain care measures that are specific to violence and abuse.
The Medical Birth Register (MBR) has existed since 1973 and contains information about pregnancies resulting in childbirth in Sweden. The information is reported by the maternity care provider. The register includes information about women who have given birth, their pregnancy, childbirth, information about the newborns, and any diagnoses the mother and child may have. Examples of information in the register include previous pregnancies, method of delivery, and child's condition at birth about 200 variables in all. Diagnoses are coded according to ICD10, and treatment codes are also used in the MBR.
Data collection: A database study was conducted to map the number of women living with FGM/C who received care in the Swedish healthcare system between 2012 and 2018 and to map the type of treatment they received. Data were obtained from the PR and the MBR on the number of care visits and type of care received, at outpatient care, inpatient specialist or obstetric care. Two ICD-10-SE codes that can be related to genital mutilation were used as the main or secondary diagnosis:
• O34.7A Care for expectant mother for abnormality of the vulva and perineum in the form of previous FGM/C
• Z91.7 FGM/C in the patient’s medical history
The new ICD10 diagnostic code Z91.7 was introduced by the WHO on January 1, 2015, and is intended to be used for women who were genitally mutilated and who seek care that is not related to pregnancy. All outpatient and inpatient care occasions where one of the main or secondary diagnoses is O34.7A or Z91.7 were retrieved from PR and MBR.
Study population: The population consists of all women with a valid social security number or coordination number who sought care in the 2012-2018 period. That means even those who were not permanent residents in Sweden were also included. Childbirth at the maternity clinic is an inpatient event that must be reported to both the PR and the MBR. Therefore, both registries include women who were diagnosed with O34.7A or Z91.7 in connection with childbirth. The variable for healthcare region was coded based on the hospital where the individual received their first care contact in the year.
Data analysis: Data obtained were analyzed using the statistical software EPI Info version 3.5.1 (CDC Atlanta, Georgia, USA). Absolute numbers and simple percentages were used to describe categorical variables. The background variables to which we had access were age, country of birth, and number of contacts with healthcare.
Inventory of regional guidelines and policies
Out of all 21 healthcare regions in Sweden, six have regional guidelines, nine have local policy documents and one has both regional and local policy guidelines. Five regions have no guidelines.
The differences between the regions' guidelines and the content of the policy documents are relatively large. The scope of information varies from a few pages to approximately 30 pages. Of the 16 healthcare regions that have some type of guideline, all but one has recommendations for treatment. The recommendations may include suggestions on how the care staff can ask questions, creating awareness that patients may perceive certain words or situations as problematic, the role of interpreters, and other cultural factors that may be important in the treatment of the patient group. Some also have checklists for different aspects of care. Only 25% of the guidelines contained information on diagnostic codes Z91.7 and 034.7A. The vast majority of regions that have guidelines have a description of the general symptoms or problems that can occur with FGM/C, such as urinary tract problems, sexual dysfunction, infertility, pain, and psychological effects. The local policy documents are primarily produced for midwifery clinics, obstetrics, and maternity care.
Of the regions that have guidelines, most (13 of 16) have recommendations for informing patients of the option of defibulation. Less than half of such guidelines are aimed exclusively at pregnant women. According to WHO recommendations, defibulation surgery should be offered not only to pregnant women before or during childbirth or in case of obstetric complications but also in case of urological complications.
Regional guidelines and policies often lack recommendations regarding sexual counseling: The national website 1177.se does offer information about FGM/C, including where to seek care. There is also information available on the national website about a special clinic in a hospital in Stockholm for "circumcised" girls and women. Information is also available about symptoms and complications and the type of treatment available, such as labial opening surgery. The websites umo.se and youmo.se also provide information about sex, health, and relationships for the 13-25 age groups. Information on FGM/C is available in English, Somali, Arabic, Tigrinya, and Farsi. There is also information on where to turn for support and help. The National Handbook of Child Healthcare is a service of Sweden's regional governments that is available online. This handbook offers pediatric healthcare providers with detailed guidelines on children and FGM/C.
Healthcare consumption among women who have been subjected to FGM/C
A total of 10,266 care visits were recorded for women with diagnostic codes O34.7A and Z91.7 during the 2012-2018 period. For this patient group, 17,112 care measures were recorded in the PR during the same period. The corresponding number in the MBR is 6,567 care measures.
In total, the database study showed that there were 4,877 women diagnosed with FGM/C who sought care at outpatient care, inpatient specialist care or obstetric care during 2012-2018. The number of women who have been subjected to FGM/C and sought care has increased steadily between 2012 and 2018 (Table 1). A significant increase have been observed in 2014-2015 which could be due to the introduction of code Z91.7, and care staff may also have become better at recorded treatment codes. Another explanation may be that women who had been subjected to FGM/C were more likely to seek care than before.
| Year | Total | ||||||
|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 4877 |
| 388 | 441 | 468 | 730 | 849 | 891 | 1110 | |
Table 1: Number of females diagnosed with FGM/C during 2012-2018.
According to information in the PR and the MBR, 97 percent of women who had been subjected to FGM/C and were registered with a diagnostic code were originally from an African country, and 87 percent were between 18 and 39 years old. In 2018, 52 girls aged 0-17 who were subjected to FGM/C sought care and received a diagnosis. Ten girls born in Sweden sought care and received a diagnosis associated with genital mutilation during 2012-2018.
Figure 1 shows the number of women who have been subjected to FGM/C and sought care at outpatient care, inpatient specialist care or obstetric care, receiving a main or secondary diagnosis of O34.7A or Z91.7, during 2012–2018, by age. Categories where the number was less than ten are marked with an asterisk. The figure shows that most women who sought care were between 18 and 39 years old. It also shows that the number of girls under 17 who receive a diagnostic code associated with FGM/C increased during 2012-2018.
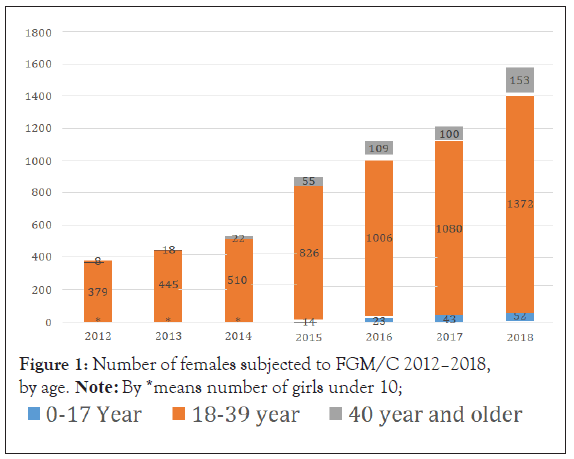
Figure 1: Number of females subjected to FGM/C 2012–2018,
by age. Note: By *means number of girls under 10;
The number of women who were subjected to FGM/C and were given diagnostic codes O34.7A and Z91.7 at outpatient care, inpatient specialist care or obstetric care, respectively, increased every year during the period 2012-2018, for all healthcare regions. Table 2 shows that there was also a year-over-year increase in women seeking healthcare and get a diagnosis compared with the total number of women who sought care during 2012-2018. For the Southern Healthcare Region and the Uppsala/Örebro Healthcare Region, however, we note that the number of women who received diagnoses related to FGM/C did increase in certain years.
| Healthcare region | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|---|---|
| North | 5 | 9 | 10 | 15 | 21 | 30 | 43 |
| Stockholm | 35 | 37 | 39 | 63 | 86 | 90 | 115 |
| South East | 20 | 21 | 21 | 27 | 28 | 36 | 59 |
| South | 9 | 11 | 15 | 18 | 17 | 17 | 17 |
| Upsala/Örebro | 9 | 15 | 15 | 34 | 41 | 44 | 43 |
| West Sweden | 17 | 19 | 26 | 49 | 65 | 63 | 94 |
Table 2: Number of females with diagnoses FGM/C per 100 000 female care seeker in health care regions in Sweden during 2012-2018.
The code Z91.7 began to be used in 2015, and since then the number of women who have been diagnosed has increased. Table 3 shows the number of women who have been subjected to FGM/C and registered according to diagnostic codes O34.7A and Z91.7 per year during 2012-2018.
| Diagnose code | Year | ||||||
|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
| O34.7A | 388 | 469 | 539 | 628 | 786 | 810 | 1002 |
| Z91.7 | - | - | - | 273 | 360 | 414 | 575 |
Table 3: Number of females with diagnoses FGM/C according to diagnose code during 2012-2018.
Type of care measures/treatment offered to women subjected to FGM/C
Table 4 lists the care measures that women and girls received in connection with receiving a diagnostic code O34.7A or Z91.7 at care visits to open or closed specialists. These care interventions can be categorized as obstetric interventions, gynecological interventions, vulvar plastic surgery, and surgery or reconstruction of the vulva or perineum.
| Type of measure/treatment | For females with main diagnose code Z91.7 | Type of measure/treatment | For females with main diagnose code O34.7 |
|---|---|---|---|
| Gynecological | Cytologist test, posterior fornix, portion and cervix uteri Vaginal ultrasound examination of the uterus, adnexa and small pelvis | Gynecological | Cytologist test, posterior fornix, portion and cervix uteri Vaginal ultrasound examination of the uterus, adnexa and small pelvis |
| Abdominal ultrasound examination of the uterus, adnexa and small pelvis | Clinical examination of female genitalia Ultrasound examination, small pelvis | ||
| Clinical examination of female genitalia Ultrasound examination, small pelvis | Other minor surgery on female genitals Complete prolapse plastic | ||
| Abdominal gynecological ultrasound examination, other specified Complete prolapse plastic | |||
| Other prolapse surgery | |||
| Obstetric | Obstetric routine ultrasound in the second trimester Obstetric ultrasound | Obstetric | Obstetric ultrasound, weight estimation Complicated pregnancy, control Obstetric ultrasound, otherwise specified Obstetric ultrasound for assessment of fetal position |
| Obstetric ultrasound, vaginal | |||
| Obstetric routine ultrasound in the second trimester Other suture or revision of childbirth injury Cardiotocography (CTG) | |||
| Examination due to decreased fetal movements | |||
| Counselling | Supporting conversation Advisory call- supportive calls | Counselling | Supporting conversation |
| Advisory conversation Information and advice to patient by phone | |||
| Surgery | Other reconstructive surgery on the vagina | Surgery | Other reconstructive surgery on the vagina Incision of the vulva or perineum |
| Other surgery on the vulva or perineum | Excision of local change in vulva or perineum Other reconstruction of the vulva or perineum Other dilation of the birth canal | ||
| Vulva plastic | Surgery vulva plastic | Vulva plastic | Surgery vulva plastic |
Table 4: Care measures/treatment for females exposed to FGM/C during 2012-2018.
Care consumption is low, but rising
Previous reports [23,24] have shown a relatively low consumption of care in light of the number of girls and women in Sweden who are estimated to have been subjected to FGM/C. The reports indicate that there may be an underreporting in the registry. These reports relate this low consumption of care to women subjected to FGM/C not seeking care, seeking care but not reporting their FGM/C status during their contact with the healthcare system, and failure of healthcare providers to ask sufficient questions about the topic. It may also happen due to previous negative experiences with healthcare visits. Reports [23,24] shows that a total of around 2,000 women have been diagnosed with FGM/C and registered in the existing national registers during 2008-2012, most often in connection with pregnancy and childbirth. Results from this study show an increase in women who seek care among the target group for most healthcare regions during 2012-2018.
Still, the number of women seeking care and receiving diagnoses associated with FGM/C may be low compared to the 38,000 girls and women in Sweden who are estimated to have undergone FGM/C. The number of girls aged 0-17 and women over 50 who sought care and received diagnoses associated with FGM/C were low in both the PR and the MBR. This may indicate that these age groups either do not need care, do not have access to care and information about care, are afraid to seek care, or avoid seeking care due to fears of stigmatization. It may also be that women do seek primary or specialist care but are not registered with a FGM/C diagnostic code and therefore are not visible in the statistics. One Norwegian study [25] showed that only one-fifth of women who underwent FGM/C seek care. Women may void care due to infibulated women's low acceptance of defibulation before marriage, since infibulation is considered a sign of virtue and innocence. It may also be due to women’s lack of knowledge about FGM/C and their own bodies, as well as what kind of care is available. Women are unaware that there are care options, such as surgery, specialist clinics, and psychosexual counseling and treatment [26]. Previous negative experiences with healthcare and unclear regulations and routines may be other reasons why women subjected to FGM/C do not seek care when they need it [26,27]. Good care meetings and encountering are also important factors that encourage women subjected to FGM/C to seek care. Care meetings allow healthcare providers to increase their knowledge about and experience with FGM/C [28-31] and establish better communication with women who have undergone FGM/C so that their patients can feel safe [32-34]. This allows providers to ask questions about patients’ FGM/C status in a non-judgmental way and involve women living with FGM/C in their own clinical care [34-36]. Healthcare providers should have the opportunity to offer transcultural and person-centered care and interpreters and written information should be available in the patients’ native language, if needed [35,36].
Care is most often sought in connection with pregnancy and childbirth
This study shows that the care measures and treatments offered to women who have undergone FGM/C most often take place in connection with pregnancy and childbirth. This is probably due to the fact that pregnancy and childbirth reveal an urgent need for care.
An earlier report from The Swedish National Board of Health and Welfare [16] shows that women born in sub-Saharan Africa have worse outcomes than other groups in terms of pregnancy complications, acute cesarean section, and stretch marks after childbirth. The report also shows that their children's Apgar scores are lower, and that perinatal death is more common. The report also draws attention to the high rate of sphincter rupture among women born in sub-Saharan Africa and mentions that it is sometimes associated with a presumably high proportion of women who have been subjected to FGM/C in this population [16].
Care measures
The WHO recommends three types of care for women living with FGM/C. Defibulation should be offered before or during childbirth; Cognitive Behavioral Therapy (CBT) should be considered for those suffering from anxiety, depression or PTSD; and sexual counseling should be made available as an option to prevent or treat sexual dysfunction. Best practices relating to a fourth area were developed on an informational and educational basis. Health information about defibulation should be given to girls and women living with type III FGM. Caregivers have the responsibility of conveying information that is correct and clear by using language and approaches that the target group can understand. Practitioners who provide care for women and girls living with FGM/C should receive information on different types of FGM/C and their associated short-term and long-term health risks [7].
Most studies on care for women who have been undergone FGM/C concern surgery; defibulation, clitoral reconstruction, and cyst removal. An important question concerns the timing of defibulation before or during childbirth and how it should be performed. In order to be able to offer appropriate care, care providers also need more training on the technical aspects of defibulation and the use of defibulation as a treatment alternative to perineotomi for infibulated women during delivery. However, the lack of research on the timing of defibulation means that it is not possible to give any advice on when the procedure should be performed. Therefore, it is important that the issue of defibulation be discussed with women who have undergone FGM/C so they can be involved in the decision on whether, when, and how defibulation should be performed [37]. This is in line with what previous research suggests: that healthcare professional should ask specific and appropriate questions about defibulation and discuss the issue early in pregnancy so that women have information and the opportunity to discuss their care options. With such information, providers and women can plan for defibulation before or during childbirth, giving patients a better experience of safe and professional care.
Clitoral reconstruction is another operation with the potential to improve the health of women who have undergone FGM/C, especially in terms of sexuality, body image, and self-esteem. If clitoral reconstruction is offered, the women who opt for the surgery should be informed that existing research does not offer clear conclusions about the effects of the procedure. It is important that women be offered psychosexual treatment as an alternative to surgery [38-40].
According to the results of the present study, the forms of care offered in Sweden to women living with FGM/C consists of obstetric procedures, gynecological procedures, vulvar plastic surgery, and other vulvar or perineum reconstructions, which is in accordance with the WHO recommendations. Psychosexual counseling for women subjected to FGM/C should be improved.
Recording of codes needs to be improved
Across the country, the study found a wide range of practices in terms of recording diagnostic codes in patient records. This could be due to a lack of knowledge about the codes and how they should be used. A previous report [24] found that the quality of reporting in the registries (PR and MBR) varied between regions. That report stressed the importance of documentation in the patient record and noted that FGM/C was sometimes not documented in the patient record. Even the present study found areas for improvement in the recording of codes. Healthcare providers do not fully use the available opportunities to report using existing diagnostic codes. Because treatment measures are coded differently in different regions, and even within regions, it is difficult to calculate the number of measures provided with certainty. Among other things, it is unclear whether defibulation operations take place before or in connection with childbirth. The number of surgical procedures, such as defibulation and vulvar reconstruction, should be recorded in a more systematic manner. Such a uniform coding system, including the new code (TLF00 Defibulation-Opening surgery in FGM), that was introduced on January 2019, increases the possibility of reporting care provided to women who have undergone FGM/C. Including information about diagnostic codes in the guidelines could thus increase their usage and thereby increase the reliability of statistics.
Policies, guidelines, healthcare providers training and care measures that offers
One study [41] examining care for women who have been subjected to FGM/C in 30 different countries showed that of these countries, 24 had a national policy on care for women subjected to FGM/C, with 20 of those national policies having been fully or partially implemented. Twenty-four countries offered training on FGM/C for healthcare staff, including 14 Western countries. Systematic training for healthcare professionals is more common in countries where FGM/C is traditionally practiced, however. In terms of access to care services, the study reported two types of surgical care: defibulation and clitoral reconstruction, and two types of counseling, psychological and sexual. Defibulation was offered in 27 countries, but in some countries it was only available at private clinics, and then in connection with pregnancy and childbirth. Clitoral reconstruction was offered in 13 countries, of which 10 were Western countries. Seven of them offered clitoral reconstruction through the public healthcare system. Furthermore, only 13 countries provided specialized psychological and sexual counseling for women who had undergone FGM/C. For example, psychological and sexual counseling is readily available in France, where all relevant nursing education programs concern FGM/C in specific areas. The Netherlands also has good coverage. Nine special centers that offer psychological and sexual counseling for women who have been subjected to genital mutilation. In Sweden, counseling is offered to women who have undergone FGM/C mainly in connection with clitoral reconstruction [41].
Previous research has shown that in general, healthcare providers lack guidelines for treating patients with FGM/C, regulations and practices are applied inconsistently, care paths are unclear and poorly coordinated, communication between healthcare centers and hospitals is insufficient, and responsibility for different roles in connection with care for women who have undergone FGM/C is diffuse [25,28,30-32,35]. The results of this study show that local policy documents are primarily produced for midwifery clinics, obstetrics practices, and maternity care. It is particularly important that these clinics have guidelines, since childbirth is an occasion when complications due to FGM/C can occur. At the same time, it is not only during childbirth that this patient group may need care or information. As The Swedish National Board of Health and Welfare [24] has pointed out in previous reports, healthcare staff in all areas may need knowledge about FGM/C in order to offer effective preventive care. The results also show that existing guidelines often lack recommendations regarding psychosexual counseling.
Methodological limitations
The inventory was based on material submitted by coordinators or on consultation with those responsible for maintaining information. The inventory therefore reflects only the material received or available on webpages. It is possible that care units may have local guidelines and routines. The study did not search for such guidelines, and they are not included in the inventory.
A major methodological shortcoming had to do with healthcare reporting and registration of codes in the registries. Some healthcare units still use the old code Z90.7, which makes it difficult to obtain exact statistics. Additionally, providers need to use the new treatment code TLF00 (Defibulation-Opening surgery in FGM) to a greater extent in order to improve statistical reliability.
This study excluded the diagnostic code Z90.7, which may have led to an underestimation of the number of women subjected to FGM/C who sought care. The code was excluded because it is also used for groups other than women who have been subjected to some kind of genital mutilation.
Mapping care measures that are directly related to FGM/C before the new code begins to be used can be complicated. Defibulation for women who have been subjected to FGM/C type III could not be coded specifically in the MBR or the PR before January 1, 2019, when the new treatment code for defibulation (TLF00) was introduced. And there are no codes yet that allow researchers to study psychosexual counseling and treatment.
Previous report from The Swedish National Board of Health and Welfare [24] shows that the quality of reporting in the registries varies between different healthcare regions, and they point out the importance of documentation in the patient record. There are different coding routines, coding terminology, database structures, and medical record systems within the different healthcare regions. A lack of documentation can be associated with a lack of knowledge about FGM and time constraints in healthcare units. Most countries fail to systematically record FGM/C in their registries [41]. Diagnostic code Z91.7 is relatively new and will, to some extent, replace Z90.7, which was excluded from this report.
The type of care that should be offered to women who have been subjected to FGM/C may vary depending on individual needs. Care may include surgical procedures in the form of defibulation, clitoral reconstruction, or removal of cysts, as well as psychosexual care. Existing treatment options in surgical care, together with psychosexual treatment, are the care measures that seem to be helpful for some women who have undergone FGM/C, but not for all. Communication and treatment are of great importance in order to be able to offer care to women who have undergone FGM/C.
Only one author
Funding
The study was done in the framework of a governmental report within Swedish national Board of health and welfare.
The authors wish to thank all participants in this study; without their contribution, it would not have been possible to undertake it. They would also like to acknowledge the valuable contribution and comments of their colleagues at the Swedish National Board of Health and Welfare.
Datasets presented in the main manuscript is available in machine- readable format (such as spreadsheets rather than PDFs) whenever possible.
Not applicable. The study was done in the framework of a governmental report within Swedish national Board of health and welfare. The data that has been used in this research study was aggregate data. Aggregate data refers to individual data that are averaged by geographic area, by year, by service agency, or by other means. Therefore there were no need to get the approval of the holders of the records. A local ethics committee ruled that no formal ethics approval was required in this particular case.
There are no conflicts of interest to declare.
Not applicable.
Citation: Akhavan S (2021) Swedish Healthcare for Women Subjected to Female Genital Mutilation/Cutting (FGM/C). J Clin Trials. S12:001.
Received: 10-Aug-2021 Accepted: 24-Aug-2021 Published: 31-Aug-2021 , DOI: 10.35248/2167-0870.21.s12.001
Copyright: © 2021 Akhavan S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.