Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2023)Volume 14, Issue 6
Purpose: Ocular surface disorders due to various causes heal up if the limbal stem cells are adequate and healthy in case of deficiency disorders manifest. To evaluate stem cell therapy in various ocular surface disorders.
Materials and methods: Study of patients with ocular surface disorders undergoing stem cell therapy in tertiary care hospitals from 2006 to 2021.
Results: Forty cases of ocular surface disorders underwent stem cell therapy from various sources. Amniotic membrane transplantation was done in Stevens Johnson syndrome (4 cases). Ocular surface stability improved in all cases with visual improvement in a case of partial stem cell deficiency from counting fingers at 2 meters to 6/36 at the end of one year. Amniotic membrane transplantation and autologous serum instillation in shield corneal ulcer with dry eye syndrome (4 cases) improved the ocular surface stability and vision from counting fingers at two meters to 6/24. Autologous circumferential barrage fashioned limbal stem cell transplantation in progressive pterygium (26 cases) and ocular surface limbal dysplasia (1 case) was most successful. Probably this procedure supplemented new stem cells in the area of partial deficiency which prevented further conjunctivalization. But homologous limbal stem cell transplantation in a case of bilateral calcareous degeneration did not work well. Surface instillation of cord blood in non-healing corneal ulcer (4 cases) probably supplemented embryonic stem cells and hastened healing.
Conclusion: Stem cell therapy from various sources in ocular surface disorders has a promising future.
Stem cell therapy; Ocular surface disorder; Limbal stem cell; Cord blood therapy
The term stem cell was proposed for scientific use by a Russian Scientist Alexander Maksimov in 1908 at the congress of Haematological society in Berlin. He postulated the existence of hematopoietic stem cells which was later discovered in human cord blood in 1978.
These are unspecified cells that have two defining properties such as the ability to differentiate into other cells and the ability to self-regenerate. They can theoretically divide without limit to replenish other cells as long as the person or animal is alive. These are present in all self-renewing tissues like skin, mucous membrane, bone marrow and regenerative systems etc. with a small population of the total tissue from 0.5% to less than 10% of the total cell population. All cells except stem cells have a limited life span and are destined to die [1].
Sources
Embryonic Stem Cells (ESC) are available in donated embryo cultured for about six months in a petri dish, cord blood, amniotic fluid and umbilical cord tissue. Adult stem cells are present in developing tooth bud of third molar, bone marrow and peripheral blood.
The stem cells for the cornea are located in the palisade of Vogt at the limbus. They act as a barrier to conjunctival epithelial cells and prevent them from migrating on to the corneal surface. Beside this, it is postulated that stem cells are present in the conjunctiva, ciliary body and retina [2].
In certain pathological conditions, however, the limbal stem cells may be destroyed partially or completely resulting in stem cell deficiency with its characteristic clinical features. These include conjunctivalization of the cornea with vascularization, appearance of goblet cells and an irregular unstable epithelium. The stem cell deficiency can be managed with auto or allo transplantation of these cells; with latter option systemic immune suppression is required.
A prospective non-comparative clinical study on stem cell therapy in various ocular surface disorders has been undertaken to evaluate for future management.
The study was conducted in the Department of Ophthalmology, in two tertiary eye care centres from January 2006 to December 2021. Forty cases of ocular surface disorders have been included for prospective therapeutic clinical trial of stem cell therapy from various sources.
The aim of therapy was not only to restore vision but to replenish limbal stem cells and maintain a stable ocular surface. The sources were freshly collected amniotic membrane, cord blood, autologous serum, auto and allo limbal conjunctiva. Fresh amniotic membrane was collected with aseptic measures from elective Caesarean section cases with informed consent from the donor and recipient. It was preserved in Ringer’s lactate solution with gentamycin injection (80 mg/2 ml) at 40°C. On the next day the amniotic membrane was thawed in the operation theatre to room temperature and was dissected from the chorion and transplanted on the ocular surface with epithelial side up by on lay method with 10-0 interrupted sutures. Intermittent incisions were given on it for better aeration. The stitches were removed after four weeks.
Autologous limbal conjunctiva was retrieved from the same or other eye of the patient and transplanted in the same sitting. The size was from 2-3 clock hours from upper limbal conjunctiva. Homologous limbal conjunctiva was retrieved from the healthy eye of a living related donor (mother) of the patient having same O+ve blood group. Anchoring 10-0 nylon interrupted sutures were given. These were removed after four weeks.
Fresh cord blood was collected with aseptic measures in elective caesarean section cases soon after the umbilical cord was cut and a pinch of Ethylenediaminetetraacetic Acid (EDTA) powder was mixed in it to preserve the cellular stability. It was preserved at 40°C and instilled into the diseased eye thrice for one day. Autologous serum was collected from the patients. This was instilled on the ocular surface thrice daily for three days in three cycles at a week interval. Post-operative care and evaluation from time to time was done in all cases for one year.
Prospective, non-comparative interventional case series of 40 patients with ocular surface disorders underwent therapeutic stem cell therapy in this study (Table 1).
| Type of disorder | No. of cases |
|---|---|
| Stevens Johnson syndrome | 4 |
| Vernal conjunctivitis with shield corneal ulcer | 4 |
| Ocular limbal dysplasia | 1 |
| Calcareous corneal degeneration | 1 |
| Non-healing corneal ulcer | 4 |
| Pterygium | 26 |
| Total | 40 |
Table 1: Types of disorders and the case series of 40 patients.
The cases included are Stevens Johnson syndrome, vernal conjunctivitis with shield corneal ulcer, ocular limbal dysplasia, calcareous degeneration of cornea, pterygium and non-healing corneal ulcer.
Stevens Johnson syndrome
All the four cases were female in the age group from 11-50 year. Fresh amniotic membrane transplantation was done in all the cases.
Amongst them one female patient aged about 13 years had a preoperative visual acuity of 6/6 in right eye and counting of fingers at two meters in left eye. This eye had partial stem cell deficiency with corneal haziness and dry eye syndrome. The post- operative vision in this eye improved up to 6/24 after one year. All the other cases had substantial clinical improvement with a stable ocular surface such as less congestion, corneal erosion and dryness. However, the visual acuity did not improve further from Perception of Light (PL) and Projection of Rays (PR) in all sectors.
Vernal conjunctivitis with shield corneal ulcer
In this category four males in the age group of 20-30 years were suffering from vernal conjunctivitis with shield corneal ulcer and dry eye syndrome two in left and two in right eyes. After amniotic membrane transplantation and three cycles at weekly interval of autologous serum instillation (thrice daily for 3 days), there was substantial clinical improvement with a stable ocular surface and vision improved from counting fingers at two meters to 6/24 after one year.
Ocular limbal dysplasia
In this category one male aged 35 years, a life convict from jail had superior limbic jelly like dysplasia in left eye. The growth was dissected from the ocular surface and autologous limbal conjunctiva extending two clock hours from the upper limbus of the other eye was transplanted in the same sitting. The histopathological study was found to be benign in nature. After one year there was no recurrence. However low grade superior limbic keratopathy resulted.
Calcareous degeneration of cornea
This was a female case aged about 23 years with bilateral calcareous degeneration of cornea. She had the visual acuity of 6/60 in right eye and counting fingers at 2 metres in left eye. Penetrating keratoplasty was done in left eye. The vision improved to 6/60, but there was recurrence after a year. So, in the next session after de-epithelization, the calcareous matter was removed by a needle and a swab stick soaked in EDTA solution. Then an allograft of limbal conjunctiva with a length of three clock hours from the upper limbus of her mother’s healthy right eye was transplanted into upper limbus of the patient. There was substantial clinical improvement of ocular surface with a visual improvement of 6/60 in that eye. But, there was recurrence after a year.
Pterygium
Twenty-five cases of progressive pterygium and one case of pterygium with cystoid degeneration under-went bare sclera excision with circumferential limbal stem cell transplantation in barrage fashion from the upper limbus of the same eye. The case with cystoid degeneration was found to be benign on histological study. There was no recurrence after one year (100%). But in the case of pterygium with cystoid degeneration, recurrence occurred in the lower side with no spread on to the cornea after three years (Figure 1).
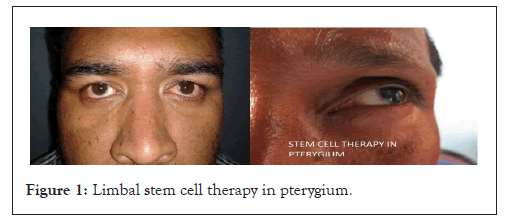
Figure 1: Limbal stem cell therapy in pterygium.
Non healing corneal ulcer
Four cases of non-healing corneal ulcer with standard medical treatment were in the age group of 21-30 years. All were male. Fresh cord blood was collected with aseptic measures, preserved with EDTA powder and instilled thrice for one day. There was substantial clinical improvement of ocular surface which hastened healing (Figure 2).
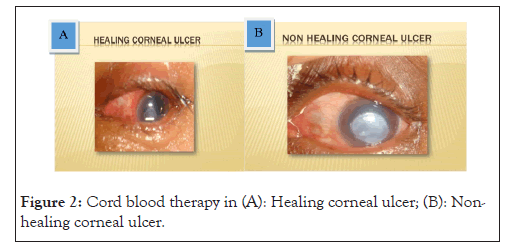
Figure 2: Cord blood therapy in (A): Healing corneal ulcer; (B): Non- healing corneal ulcer.
The management of ocular surface disorders is a challenging task as most of these cases lead to visual disability. Scientists proposed an X, Y, Z hypothesis of corneal epithelial maintenance in which the desquamated cells (Z-component) are continuously replaced not only by the basal cells (X-component) that divide but also by cells that migrate from the periphery (Y-component). Thus, migration occurs centripetally from the limbus and vertically from the basal cell layer. In case of limbal stem cell deficiency this kinetic maintenance of corneal epithelium is hampered leading to various ocular surface disorders [3].
Stem cell therapy in the form of amniotic membrane transplantation, limbal stem cell transplantation, cord blood and autologous serum instillation has been done in this study as a therapeutic clinical trial in various ocular surface disorders.
In this study amniotic membrane transplantation was done in Stevens Johnson syndrome and vernal conjunctivitis with shield corneal ulcer. In all the cases, there was substantial clinical improvement such as diminution of congestion and stabilization of ocular surface. There was visual improvement in one case of partial stem cell deficiency in Stevens Johnson syndrome with visual improvement up to 6/24 from counting fingers at two meters. In the case of vernal conjunctivitis with shield corneal ulcer there was also visual improvement up to 6/24 with substantial clinical improvement.
The first use of the amniotic membrane in ophthalmology was by de-Roth in 1940 who reported partial success in the treatment of conjunctival epithelial defects after symblepharon. Sorsby and Samons in 1946 found that patients with caustic burn of the conjunctiva with corneal involvement could be treated successfully using amniotic membrane. In 1995, Kim and Tseng used amniotic membrane transplantation for ocular surface reconstruction of severely damaged cornea in a rabbit model.
Anderson, et al. [4] studied 17 eyes of 15 patients with partial limbal stem cell deficiency who underwent superficial keratectomy of the conjuctivalized corneal surface followed by amniotic membrane transplantation. Follow up was done for at least a year. All eyes exhibited a stable intact corneal epithelial surface after a mean follow up period of 25.8 months with no eyes developing recurrent erosion or persistent epithelial defect. The mean time for re-epithelialization was 22.8 days. Overall improvement in visual acuity was observed in 92.9% of 14 eyes with potential vision. Pain and photophobia were abolished in 86% of cases and substantially reduced in 14% with all eyes exhibiting decreased vascularization and inflammation at the final follow up.
Amniotic membrane transplantation appears to be a safe and effective method of restoring a stable corneal epithelium in cases of partial limbal stem cell deficiency and can be considered as an alternative to limbal auto graft or allograft.
In patients with total limbal stem cell deficiency, autologous or homologous limbal transplantation are indicated for corneal surface reconstruction. This may be combined or followed with keratoplasty. The current technique was proposed by Kenyon and Tseng, but several modifications have been described. All these procedures aim to remove host’s diseased corneal epithelium and transplant a new source of stem cells. After successful transplantation, the host’s cornea is permanently covered by healthy epithelium. Donor’s tissue can be obtained from the healthy fellow eye (limbal auto graft) in case of unilateral disease or from a living related donor or cadaveric eye (limbal allograft) when both eyes are involved [5].
Tsubota, et al. [6] performed 73 stem cell transplantation in 42 patients. Three patients did not come for follow up. Thus, they evaluated 70 procedures in 43 eyes of 39 patients (26 male, 13 female) with mean age of 49 ± 23 years. The overall success was corneal epithelization -51% and clear cornea -35%. The patients had a final post-operative visual acuity of 0.02 (1/60). Persistent epithelial defects developed in 60% which subsided with treatment. The overall result of corneal graft-rejection in eyes in which cornea and stem cell were transplanted simultaneously was 40%. Most serious complications after surgery were ocular hypertension in 16 eyes (37%).
Tsai, et al. [7] have studied reconstruction of damaged cornea by transplantation of autologous limbal epithelial cells expanded in vitro on amniotic membrane in 6 patients with partial or total limbal stem cell deficiency due to chemical burn (3 cases), pseudo pterygium after excision of a cyst, congenital pterygium and recurrent chronic inflammation with phlyctenular degeneration (one case each). Four of the patients had undergone surgery like autologous conjunctival transplantation, amniotic membrane transplantation or both procedure in the damaged eye, but failed to improve. After a mean follow up period of 15 ± 2 months, vision improved in 5 of the 6 eyes (83%) that received transplant. There had been no recurrent neovascularization or inflammation in the transplanted areas during the follow up period.
Koizumi, et al. [8] have studied cultivated corneal epithelial transplantation for ocular surface reconstruction in acute phase of Stevens Johnson syndrome in 2 patients. Shortly after the transplantation conjunctival inflammation rapidly subsided. After six months their ocular surface epithelium was stable without defects.
Shimazaki, et al. [9] observed 13 eyes of 13 patients with severe limbal deficiency (Stevens Johnson syndrome-8 eyes, ocular cicatricial pemphigoid-3 eyes and chemical burn-2 eyes) treated by transplantation of allo limbal epithelium cultivated in amniotic membrane on to the ocular surface. After the surgery the epithelium regenerated and covered the ocular surface in 8 eyes (61.5%). However, 3 of 8 eyes developed partial conjunctival invasion and 2 eyes developed epithelial defect. At the last examination corneal epithelization was achieved in 6 eyes (46.2%), 5 had conjunctivalization, one had dermal epithelization and one was not epithelized. Complications were corneal perforation in 4 eyes and infectious keratitis in 2 eyes.
Nishida, et al. [10] reported the result of ocular surface reconstruction in 4 patients having bilateral stem cell deficiency with the use of cultivated autologous oral mucosal epithelial cells in carrier free tissue replacement sheets. Corneal transparency was restored and post-operative visual acuity improved remarkably. During the follow up period the corneal surface remained transparent and there was no serious complication. They have shown that tissue engineered epithelial cell sheets fabricated ex vivo from autologous oral mucosal epithelium are effective for reconstructing the ocular surface and restoring vision in patients with bilateral stem cell deficiency.
Sangwan, et al. [11] had done prospective non-comparative interventional case study in patients with limbal stem cell deficiency due to chemical injury (3 cases) and xeroderma pigmentosum (1 case). Three eyes received living related limbal conjunctival transplantation and one received harvested cadaveric kerato-limbal allograft. Penetrating keratoplasty was done 3-4.5 months later for visual rehabilitation. Duration of follow up after penetrating keratoplasty ranged from 4-11 months. The ocular surface remained stable in all patients. Visual acuity improved in the early post-operative period in all patients but reduced in two cases due to endothelial rejection and secondary glaucoma.
Basu, et al. [12] studied 125 patients, 65 adults and 60 children who developed unilateral limbal stem cell deficiency after suffering from ocular surface burns and underwent simple limbal epithelial transplantation between 2010 and 2014. After a median post-operative follow up of 1.5 years 95 out of 125 eyes (76%) maintained a successful outcome. Two-line improvement of visual acuity was seen in 75.2% and 67% of cases attained 6/18 or better vision. Progressive conjunctivalization occurred in 18.4% cases.
Mahdy, et al. [13] studied a group of 42 eyes of 42 patients with grade I-III primary pterygium who had undergone pterygium excision followed by superotemporal limbal stem cells and conjunctival autograft transplantation in all cases. Within a mean follow up period of 18.26 months (10-28 months), recurrence occurred in two eyes (4.75%). No other significant complications were noted.
In this study autologous limbal stem cell transplantation in circumferential barrage fashion was done in one case of limbal dysplasia and 26 cases of pterygium. In the first case there was no recurrence except mild upper limbic keratopathy and in the later cases, there was no recurrence after one year. This probably prevented further conjunctivalization of the cornea. In other forms of pterygium surgery like bare scleral excision, conjunctival transplantation from upper bulbar conjunctiva, there are chances of recurrence. But when limbal conjunctiva is transplanted in circumferential barrage fashion, there is no recurrence. Probably partial limbal stem cell deficiency in the exposed part of inter palpebral fissure may be a causative factor in pterygium. In case of pterygium with cystic degeneration there was recurrence in the adjacent lower part after 3 years with no progression to the corneal surface.
In the case of calcareous corneal degeneration, the allo graft of limbal conjunctiva from mother having same blood group (living related donor) did not work satisfactorily leading to recurrence.
Cord blood stem cells are much more primitive than bone marrow or peripheral blood. These cells have more advantages over those retrieved from bone marrow. It is much easier to get because they are readily obtained from the umbilical cord and placenta at the time of delivery. Harvesting stem cells from bone marrow require a surgical procedure under general anesthesia. Cord blood stem cell can be stored and transplanted back into the donor or to a family member or to an unrelated recipient. Perfect tissue matching is needed in bone marrow transplantation, where as in case of cord blood, even partial matching can be successful. Banked stem cells from cord blood can be more readily available for immediate use than a matched bone marrow. A study found that children who received a cord blood transplant from a closely matched sibling were 59% less likely to develop graft versus host disease than children who received a bone marrow transplant from a closely matched sibling. Cord blood contains stem cells capable of giving rise to epithelial tissue, making it amenable for application in the cornea and skin for wound healing. In case of eye cornea appears to be suitable for routine clinical application.
Harris, et al. [14] have used cord blood stem cells as a viable therapeutic modality for ocular surface disease and as a source of tissue for ocular surface reconstruction. Preliminary laboratory and animal data are supportive of this hypothesis.
Sharma, et al. [15] did a double blind prospective randomized controlled clinical study in 33 eyes of 32 patients with acute ocular chemical burns of grade III, IV and V severity. They were randomized in three groups such as umbilical cord serum (n=12), autologous serum (n=11) and artificial tears drops (n=10) therapy. In addition, all eyes received standard medical treatment. After 3 months, the extent of limbal ischaemia with cord blood serum showed a mean percentage decrease of 73.43 ± 25.51 compared with 35.54 ± 25.60 and 43.71 ± 28.71 with autologous serum and artificial tears respectively (p=0.008). More patients had clear corneas with cord blood serum compared with autologous serum and artificial tears (p=0.048).
Umbilical cord serum therapy is more effective than autologous serum eye drops or artificial tears in ocular surface reconstruction after acute chemical injuries. In our study, fresh cord blood was instilled on the corneal surface thrice for one day in 4 cases of non-healing corneal ulcer. This hastened healing in the follow up period.
Forty cases of ocular surface disorders had undergone stem cell therapy in the form of fresh amniotic membrane transplantation, auto and allo limbal stem cell transplantation from living related donor (mother with the same blood group), autologous serum and fresh cord blood instillation. Out of these amniotic membrane transplantation in Stevens Johnson syndrome and shield corneal ulcer improved the ocular surface stability. Autologous circumferential barrage fashioned limbal stem cell transplantation in pterygium and ocular dysplasia was most fruitful; because probably this procedure supplemented new stem cell population in the area of partial deficiency. It prevented further conjunctivalization. Cord blood instillation in cases of non-healing corneal ulcer supplemented stem cell population and hastened healing. However, this needs further evaluation at other centres.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Das G, Dash PNM (2023) Stem Cell Therapy in Ocular Surface Disorders, Our Experience. J Clin Exp Ophthalmol. 14:965.
Received: 27-Oct-2023, Manuscript No. JCEO-23-27253; Editor assigned: 30-Oct-2023, Pre QC No. JCEO-23-27253 (PQ); Reviewed: 13-Nov-2023, QC No. JCEO-23-27253; Revised: 20-Nov-2023, Manuscript No. JCEO-23-27253 (R); Published: 28-Nov-2023 , DOI: 10.35248/2155-9570.23.14.965
Copyright: © 2023 Das G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.