
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Case Report - (2022)
Liposarcoma is one of the most common soft tissue sarcomas and has multiple subtypes, including atypical, welldifferentiated, and dedifferentiated. These tumors most commonly occur in the extremities and the retroperitoneum, and account for 20% of all retroperitoneal tumors. A 53 year-old male presents in the outpatient setting for evaluation and management of bilateral inguinal hernias. This is a case report describing a retroperitoneal liposarcoma presenting with bilateral inguinal hernias containing intraperitoneal fat from mass effect.
Liposarcoma; Retroperitoneum; Bilateral inguinal hernia repair
Retroperitoneal liposarcoma is very rare overall, occurring in 2.5 per one million people. Patients will present from symptoms of mass effect due to the uncontrolled growth in the large potential space of the retroperitoneum, with its median size being around 30 cm.
The mainstay of treatment for this type of tumor is resection to a negative margin. The patient describes bulges in bilateral groins for multiple months. This is a case report describing a retroperitoneal liposarcoma presenting with bilateral inguinal hernias containing intraperitoneal fat from mass effect.
A 53 year-old male presents in the outpatient setting for evaluation and management of bilateral inguinal hernias. He has a past medical history of hypertension and benign prostatic hyperplasia. The patient describes bulges in bilateral groins for multiple months. He had associated abdominal pain and weight gain at this time. He was boarded for robotic assisted bilateral inguinal hernia repair.
Upon intubation, it was noticed that the patient had a protuberant abdomen. When palpated a hard mass was felt. A laparoscope was inserted into the abdomen demonstrating what appeared to be a large retroperitoneal mass (Figure 1).
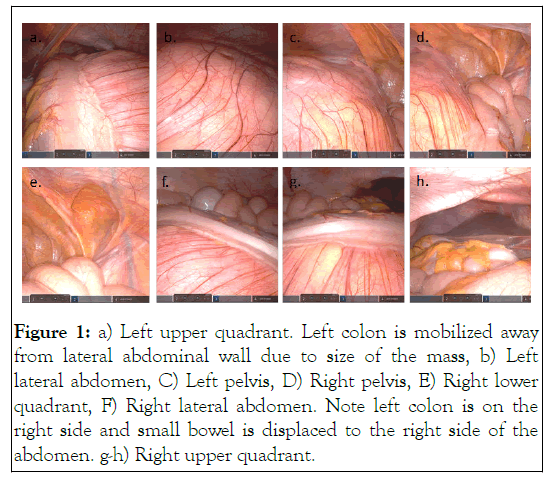
Figure 1: a) Left upper quadrant. Left colon is mobilized away from lateral abdominal wall due to size of the mass, b) Left lateral abdomen, C) Left pelvis, D) Right pelvis, E) Right lower quadrant, F) Right lateral abdomen. Note left colon is on the right side and small bowel is displaced to the right side of the abdomen. g-h) Right upper quadrant.
The patient was closed and sent for a CT scan. The image showed a large homogenous, retroperitoneal mass which had characteristics consistent with a liposarcoma (Figure 2a and 2b) (Hounsfield units-14.4).
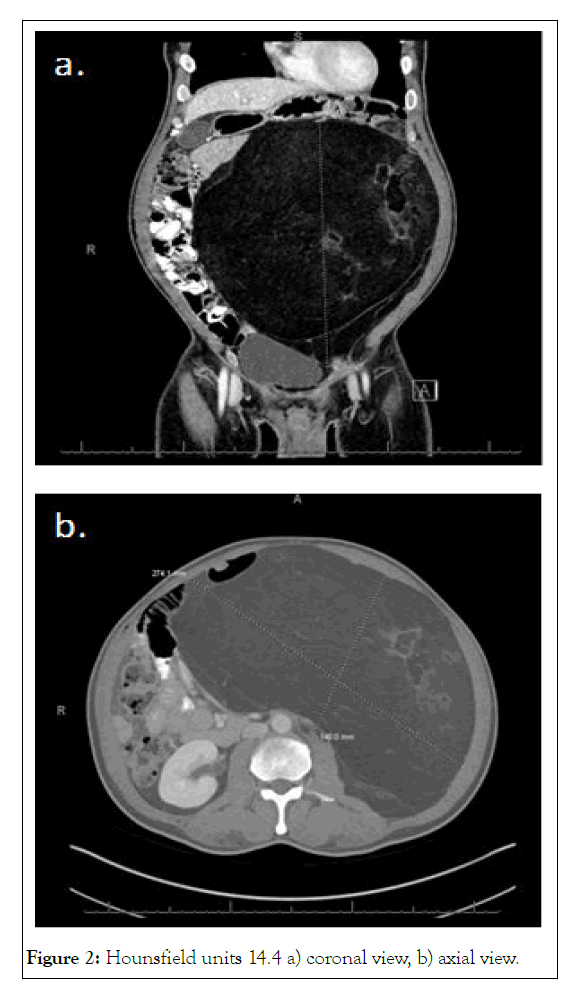
Figure 2: Hounsfield units 14.4 a) coronal view, b) axial view.
The decision was made to proceed with resection. The patient had a bowel prep prior to surgery using GoLytely© and underwent an exploratory laparotomy. A large midline incision was made and the abdomen was entered.
Abdominal fat was present in each inguinal hernia from mass effect of the large retroperitoneal tumor. The retroperitoneum was opened and the largest mass was observed immediately.
It was well-encapsulated circumferentially. Dissection was carried out using a combination of blunt dissection and electrocautery, taking care not to violate the capsule. No local invasion into the retroperitoneal structures was appreciated.
The mass weighed ten pounds and six ounces (Figure 3). Multiple small tumors were seen and excised from the retroperitoneal space.
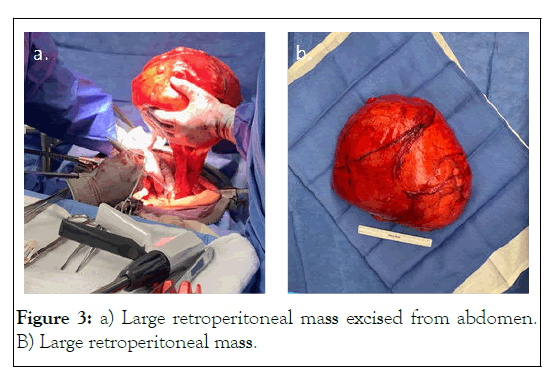
Figure 3: a) Large retroperitoneal mass excised from abdomen. B) Large retroperitoneal mass.
These were similar in character to the large mass. There was one tumor that herniated into the inguinal defect on the left side, which was removed.
Adequate hemostasis was achieved and the abdomen was closed without difficulty. A total of eight specimens were sent for pathologic analysis.
The pathology report described each individual mass as FNCLCC grade 1 well differentiated liposarcoma extending to the surgical margin. The largest tumor measured 28 cm in diameter. The other seven specimens ranged from 4 to 13 cm. The patient had a scaphoid appearing abdomen postoperatively (Figure 4).
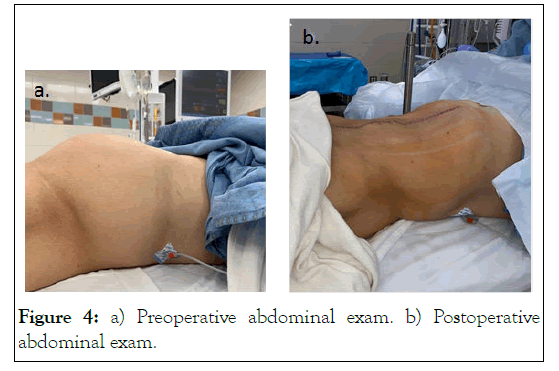
Figure 4: a) Preoperative abdominal exam. b) Postoperative abdominal exam.
Imaging for retroperitoneal liposarcoma includes a CT scan of the chest, abdomen, and pelvis, with metastasis present in up to 50% of these images [1,2]. Well differentiated tumors appear homogenous in nature and similar to surrounding adipose tissue with septations throughout the mass, while the undifferentiated subtype is heterogenous without similarities to surrounding fat [3-7]. MRI may also be a useful adjunct to identify satellite lesions and further demarcate boundaries of the tumor [7]. Surgical planning and intervention may be based on imaging findings alone. Biopsy for liposarcoma is unnecessary unless distal disease is present or it invades vital structures. In this case, biopsy is recommended to direct systemic therapy [5].
The primary treatment of liposarcoma is complete macroscopic resection [8]. Up to 40 percent of patients require contiguous organ removal. The organ most commonly taken is the kidney, followed by the colon [9]. En bloc resection with negative margins confers the greatest opportunity for remission. If there is tumor invasion into important neurovascular structures, the overlying fascial layer of the structure is taken to optimize margins without taking the structure itself [10]. However, these patients have a high rate of recurrent disease. It has been cited that local recurrence occurs in 2/3 of patients with retroperitoneal liposarcoma secondary to difficulty in obtaining adequate margins [2]. Our patient had involvement of the margin of his resection and due to the location of his tumor will likely have a high risk of recurrence. This will make postoperative adjuvant therapy and surveillance an important aspect of his course.
Adjuvant therapy recommendations remain controversial as either chemotherapy or radiation has shown significant survival benefit in well differentiated or dedifferentiated liposarcoma [8]. Adjuvant radiation should be considered in patients with high risk for recurrence, such as in our patient. Placing clips at the margins of resection is helpful for deciding precise locations to radiate, however in our patient; no clips were placed because his tumor involved the entire retroperitoneum. Neoadjuvant radiotherapy has been associated with increased wound complications, particularly in the extremities, as opposed to receiving radiation postoperatively. This is one reason a multidisciplinary approach is imperative in the liposarcoma patient [10]. There have been multiple case reports demonstrating the efficacy of neoadjuvant chemotherapy in treating dedifferentiated liposarcoma of the retroperitoneum [11,12]. Currently, there is no consensus of the role of chemotherapy overall in the treatment of liposarcoma. Further randomized control trials should be completed to evaluate its efficacy. This patient will be followed as an outpatient and presented at tumor board to determine his appropriate next steps in treatment.
Local recurrence is the most common cause of mortality in these patients. Because of this, patients require routine surveillance imaging by CT scan every three to six months for 3 years, then every six months for two years, and annually thereafter. Pathologic grade of tumor is the most important prognostic factor and predictor of local recurrence. Other factors influence the rate of local recurrence including gross residual disease, tumor rupture, high grade and positive margins.
Retroperitoneal liposarcoma is a rare form of cancer that requires a multidisciplinary approach to treatment. Our case is an example of a well differentiated retroperitoneal liposarcoma that was treated with primary resection.
Citation: Lehman HS, Qasawa DOR, Lim DJJ (2022) Retroperitoneal Liposarcoma Presenting as Bilateral Inguinal Hernias. J Clin Trials. S15:005.
Received: 10-Dec-2021 Accepted: 24-Dec-2021 Published: 31-Dec-2021
Copyright: © 2022 Lehman HS, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.