Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2020)Volume 11, Issue 4
A 57-year-old male patient operated 5 years before for cataract, arrives in our emergency service complaining of sudden decrease of the visual acuity of the left eye. Slit lamp examination reveals aphakia, iridodonesis and nonreflective semi-mydriatic pupil. Volk ® lens examination of the fundus shows dislocation of the entire bag-IOL complex into the vitreous. Our approach was: pars plana posterior vitrectomy, IOL-capsular bag complex extraction and implantation of an iris-claw artificial IOL with good anatomical and functional results. Iris-Claw artificial IOL’s are in the authors’ opinion a good and less invasive method for treating afakia of any cause.
Aphakia; Iris-claw; Mydriasis; Trauma
Dislocation into the vitreous cavity of an implant previously implanted in the capsular bag is not very common. There are several causes that can lead to this: capsular pseudoexfoliation [1,2] long after cataract surgery [3,4] retinitis pigmentosa [5] and trauma.
Herein we aim to present the case of a patient who underwent cataract surgery with no post-operative complications, and who displays in-the-bag IOL complex dislocation into the vitreous, subsequent to ocular trauma.
A 57-year-old male patient operated 5 years before for cataract, arrives in our emergency service complaining of sudden decrease of the visual acuity of the left eye. Slit lamp examination reveals aphakia, iridodonesis and non-reflective semi-mydriatic pupil, with a visual acuity of 1.2 logMAR. Volk ® lens examination of the fundus shows dislocation of the entire bag-IOL complex into the vitreous (Figure 1).
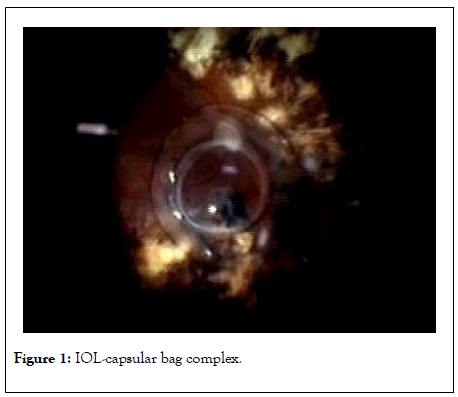
Figure 1: IOL-capsular bag complex.
The author followed the tenets of the Helsinki Declaration. The patient was informed about the risks and benefits of the surgery, and a formal consent was obtained in writing after thorough explanation of the procedure. Consent to publish the case and images related to it was also gathered.
Local retro-bulbar anaesthesia is performed and then surgery starts with the insertion of 23 Ga trocars 3.5 mm off the limbus-being an aphakic eye. We perform posterior vitrectomy at 5000 cuts/ min until the bag-IOL complex is detached from the vitreous and moves easily on the retinal surface. The capsular bag-IOL complex is raised in the anterior chamber (Figure 2) using a forceps. A 5.4 mm corneal incision is performed (the optical diameter of an Artisan implant), through which the capsular bag-IOL complex is extracted (Figure 3), and the new 24D implant will be implanted, based on previous biometry. Explantation and implantation are performed while the infusion is closed and the vascoelastic substance is present in the anterior chamber. The vascoelastic substance is injected in order to protect the corneal endothelium, as well as to preserve the optimal depth of the anterior chamber when the infusion is closed.
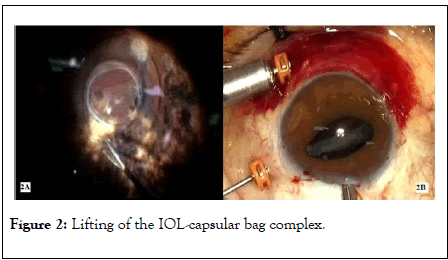
Figure 2: Lifting of the IOL-capsular bag complex.
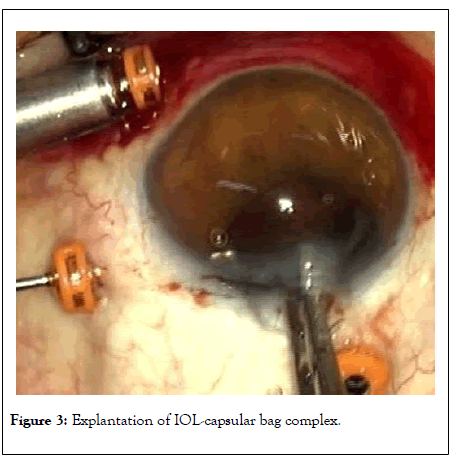
Figure 3: Explantation of IOL-capsular bag complex.
Artisan IOL implantation requires the pupil to be as small as possible, which is why we start by injecting myotic substances into the anterior chamber. It is implanted using a forceps (Figure 4) and positioned on the horizontal axis so as to allow for irisclaws. The implant is positioned on the posterior surface of the iris by inserting it (pressing it) into the implant claws (Figure 5) with the help of an instrument produced by the manufacturing company. In this case, peripheral iridectomy was not necessary, because of the preoperative posttraumatic semi-mydriasis. The corneal wound is sutured in X with a 9-0 thread (Figure 6). In the end, 0.1 ml of cefuroxime solution is injected in the chamber for the prophylaxis of endophthalmitis, the trocars are removed and ocular tonus is restored through BSS hydro-suture.
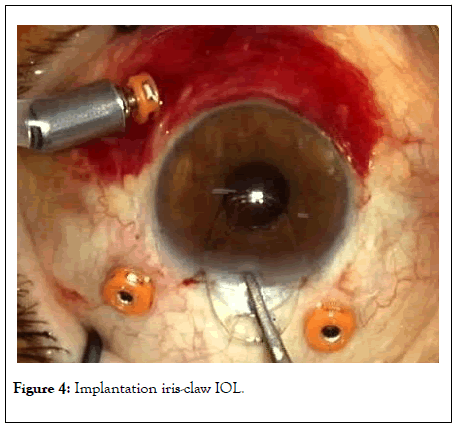
Figure 4: Implantation iris-claw IOL.
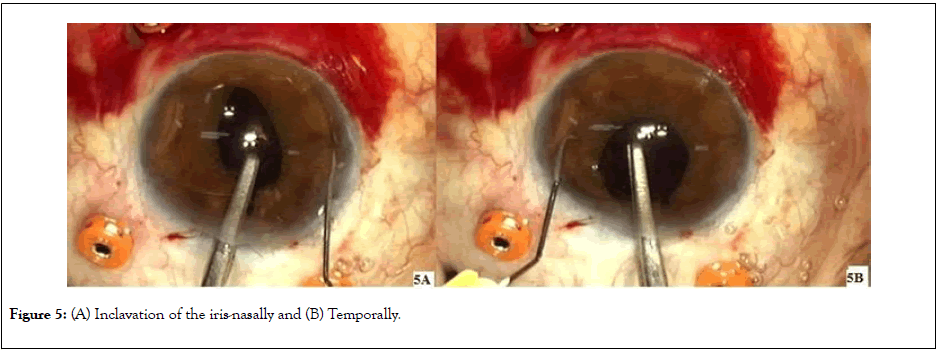
Figure 5: (A) Inclavation of the iris-nasally and (B) Temporally.
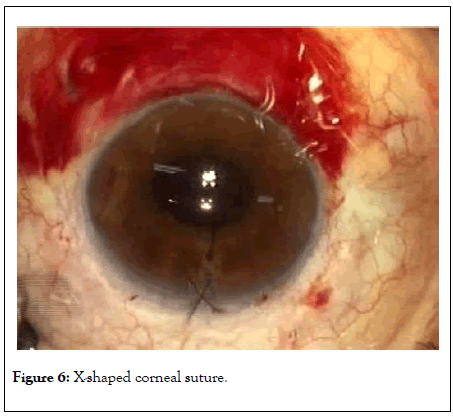
Figure 6: X-shaped corneal suture.
The postoperative visual acuity obtained was: UCVB 20/32 with a +1,-1,5x 75° refraction.
Generally, the artificial IOL is explanted through a standard 2.2 mm corneal incision. To preserve the architecture of such an incision and obtain minimal postoperative astigmatism presupposes partial fragmentation of the implant with special scissors [6,7].
In this case, the surgeon's aim is to implant an artificial iris-claw type lens.
This is a rigid type of lens with a 5.4 mm optic diameter. The incision through which the artificial IOL will be inserted in the anterior chamber is of the same size. Therefore, intraoperatively, it was possible to explant the capsular bag-IOL complex in its entirety, without fragmenting it.
There are several procedures to correct traumatic aphakia. One of these procedures involves the use of an implant sutured to the sclera. The benefits of using this technique are a diminished risk for corneal decompensation, sinechiases and secondary glaucoma due to the positioning of the implant posterior to the iris [8,9]. The technique is much more difficult to perform and requires an experienced surgeon [10].
The technique of positioning foldable 3 piece implants into the sclera may be a good option. The advantage is that it requires a small incision (2.2 mm) [11] and eliminates possible complications that may occur due to suture.
Both techniques of positioning the implant into the sclera, either by suture or by inserting implant haptic, require additional incisions, even if very small. This is why I preferred Artisan implantation, in order to minimize the number of incisions.
The Artisan implant can be positioned in front of the iris or behind the pupil. The positioning of the implant posterior to the iris, as in our case, involves a smaller loss of endothelial cells than in the case of anterior positioning [12].
Posterior implantation of the iris-claw combines the advantages of having an implant inside the posterior chamber, a well performed surgery in a short time and an easy to perform technique [13]. There are studies that show that posterior implantation of the Artisan in eyes with a smaller anterior chamber depth (posterior diameter <24 mm) is safer than in eyes with a larger posterior chamber [14]. In our case we used a +24 D Artisan implant, which shows a hypermetropic eye with a smaller anterior chamber depth (22.7 mm).
The major disadvantage of the Artisan implant is that it requires a large incision (5.4 mm), which is also the optical diameter of the implant. This disadvantage can be remedied by using the Artiflex foldable implant that requires a 2.75-3.2 mm incision. This reduces the postoperative astigmatism resulting from a 5.4 mm incision [15]. Artiflex is mostly used for refractive purpose and the manufacturer does not provide the dioptre needed for our patient.
In order to diminish any post-operative astigmatism we opted for suturing the incision with a 9-0 thread, because of the large 5.4 mm incision. The postoperative refraction of +1-1,5 × 75° shows a good suture, with an X thread that is not very tight [16-18].
Another aspect of this case is traumatic mydriasis. There are several surgical techniques that can reduce a significant traumatic mydriasis. For example, cerclage suture of the iris, artificial iris implantation or, in cases with extreme traumatic mydriasis, even the use of implants that can be sutured to the sclera, which also have the diaphragm and are used in cases of aniridia. In this case it was not necessary to use threads or other devices and techniques to reduce the pupil size, because mydriasis was not significant. Subsequent to Artisan implantation I noticed a slight shrinkage of the pupil through the iris that was well inserted in the implant clamps, pushed from the periphery to the pupil, and thus reducing the pupil diameter.
Citation: Rosca C (2020) Retro Pupillary Iris Claw IOL the Treatment for Traumatic IOL Capsular Bag Complex Dislocation. J Clin Exp Ophthalmol. 11:852. DOI: 10.35248/2155-9570.20.11.852
Received: 23-Jun-2020 Accepted: 07-Jul-2020 Published: 14-Jul-2020 , DOI: 10.35248/2155-9570.20.11.852
Copyright: © 2020 Rosca C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.