Translational Medicine
Open Access
ISSN: 2161-1025
ISSN: 2161-1025
Case Report - (2023)Volume 13, Issue 2
Prosthesiss dislocation is considered one of rare complications after artificial femoral head arthroplasty. We present a case of the complication related to small head dislocation from the cup. This was a 70-year-old female with acute cerebral infarction patient undergoing three operative treatments after the femoral neck fracture within a short perioperative period. The dislocation was not resolved until the last revision of partial prosthetic components. Prosthetic components dislocation is rarely reported, yet it may cause open reduction once happened in patients. Special attention should be warranted to the implants and the special patients as they might suffer from the recurrent dislocation and be amenable to surgical treatment.
Bipolar components; Dislocation; Hemiarthroplasty (HA); Revision hip arthroplasty
Total Hip Arthroplasty (THA) is one of the most popular orthopedic surgeries, and the most successful surgical interventions of the last century [1,2]. Dislocation of the prosthetic hip is one of the common complications in patients undergoing THA, especially be comorbiding with thromboembolic disease and deep wound infection [3]. Usually dislocation of the prosthetic hip is treated promptly either by close reduction or other surgical means [4]. The prosthetic components dislocation is a medical entity rarely encountered or reported. To our knowledge, dissociation between femoral head and cup is an extremely rare complication of bipolar hemiarthroplasty [4,5]. We report an unusual case of complication related to this condition dislocation of the prosthetic femoral small head from the cup.
A 70-year-old woman presented to the emergency department with 20 days of right hip pain and limitation of motion. The patient had past medical history including chronic cerebral infarction with right limb hemiplegia for one year. Her radiograph of the pelvis showed Garden Ⅳ right femoral neck fracture (Figure 1A). She was admitted and underwent the uneventful cement artificial femoral head replacement. The post operation examination and radiograph were unremarkable (Figure 1B).
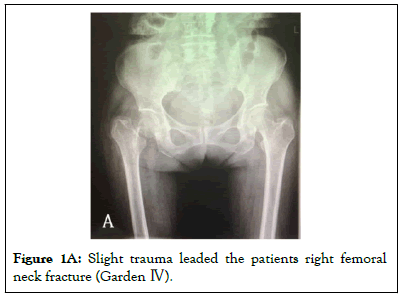
Figure 1a: Slight trauma leaded the patients right femoral neck fracture (Garden Ⅳ).
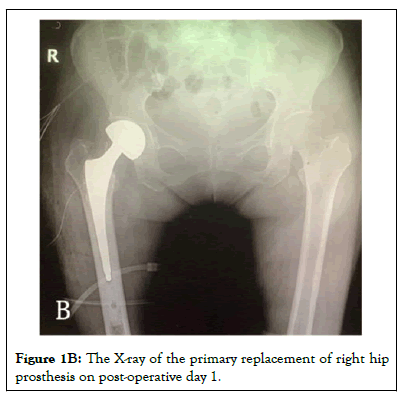
Figure 1b: The X-ray of the primary replacement of right hip prosthesis on post-operative day 1.
The patient was advised to walk with walking aids postoperatively. The patient complained of pain in the right hip on the postoperative day 11 and couldn’t walk again. The radiograph showed the dislocation of the prosthetic head from the cup with the prosthetic cup still in place (Figure 2A). The attempt of closed reduction was unsuccessful and the open reduction was performed. We found the small prosthetic head with the femoral stem dislocated from the cup and the all components were intact. Intraoperatively it was observed that locking mechanism of polyethylene ring was unimpaired. We decided to reassemble the parts as the primary replacement (Figure 2B).
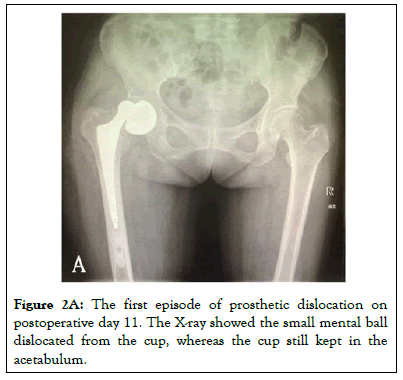
Figure 2a: The first episode of prosthetic dislocation on postoperative day 11. The X-ray showed the small mental ball dislocated from the cup, whereas the cup still kept in the acetabulum.
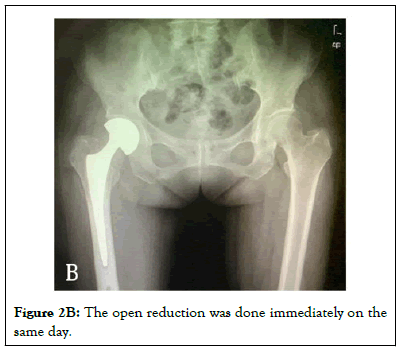
Figure 2b: The open reduction was done immediately on the same day.
The patient tolerated the procedure well and was discharged home uneventfully. On the postoperative day 40, the patient was admitted again due to the similar intro-prothetic dislocation of head and cup which was evidenced with radiographic and intraoperative findings (Figure 3A). The second revision procedure was scheduled. At the beginning we presumed that the refractory intraoprothetic dislocation resulted from an undetectable product defect. The preexisting prosthetic head and cup was exchanged for a new implant from another manufacturer (Figures 3B and 3C). The X-ray showed the small mental ball dislocated from the cup, whereas the cup still kept in the acetabulum. When we tried to relocate it by manual reduction, the cup was dislocated from the acetabulum.
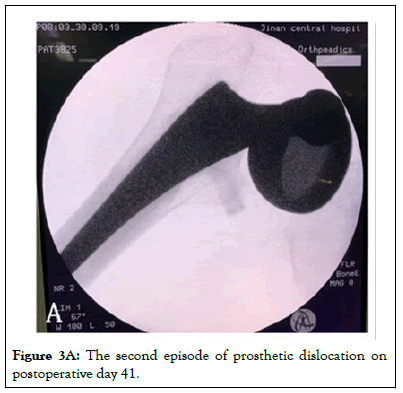
Figure 3a: The second episode of prosthetic dislocation on postoperative day 41.
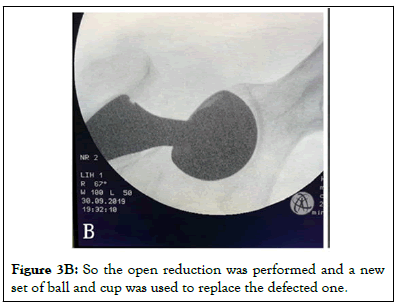
Figure 3b: So the open reduction was performed and a new set of ball and cup was used to replace the defected one.
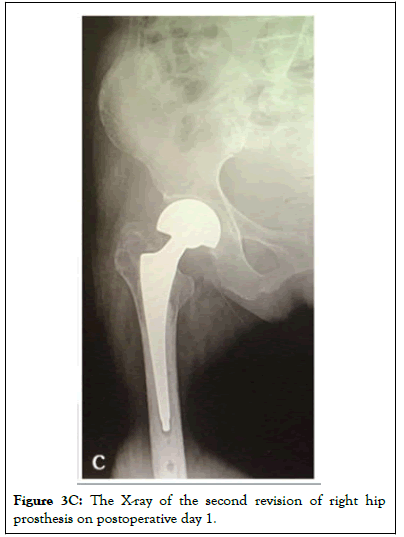
Figure 3c: The X-ray of the second revision of right hip prosthesis on postoperative day 1.
The replaced prosthetic implant was scrutinized after the procedure. It was found the prosthetic head was inserted and locked in the cup well which could not be detached effortlessly under a dry and clean condition. And then a small amount of soap water was added between the prosthetic head and cup to imitate the joint fluid under the condition of which the head and cup were easily separated with an abrupt force at specific angles. The video showed the imitation of prosthetic dislocation using the retrieved implants.
Furthermore, during the patient encounter, the patient recalled that the dislocation happened while she suddenly changed her right hip position. This motion replicated the above mentioned observation of the retrieved implants and verified the assumption that when a sudden force on the small prothestic head and cup is great enough an introprosthetic dislocation may occur. During 2 years clinical surveillance after the 2nd revision procedure, the patient Right Lower Extremity (RLE) function recovered and the implant was stable with no evidence of dislocation (Figure 4).
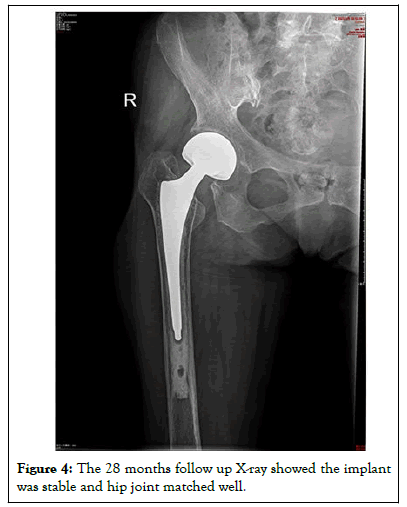
Figure 4: The 28 months follow up X-ray showed the implant was stable and hip joint matched well.
There are three types of femoral Hemiarthroplasty (HA) components: monoblock stem, modular stem with a unipolar head, and modular stem with a bipolar head. Modular stems have the advantage of a free adjustment of femoral offset. Bipolar heads have a risk reduction for reoperation due to acetabular erosion compared with monoblock heads [6-8]. Major clinical findings in hip dislocation are hip pain, deformity, and limited range of motion. Most dislocations are treated with closed reduction and nonsurgical management (immobilization and bracing) that frequently succeed in preventing recurrence [9,10].
Dislocation of the prosthetic hip is a common complication after Total Hip Arthroplasty (THA) or HA. Several risk factors for this complication have been identified over the years. Patient-related risk factors include age older than 80 years [9], female gender, neuromuscular and cognitive disorders [11], patient's noncompliance [12,13], and patients who underwent any prior hip surgery [14]. Surgical-related risk factors for dislocation include surgical approach (posterior more than anterior approach), soft tissue tension, component positioning, impingement, head size, and surgeon experience [15-17].
In our case, the risk factors for dislocation are unrival soft tissue tension and dysfunctional component locking mechanism. We took into account of the patient’s past medical history of cerebral infarction with right limb hemiplegia and old age when the HA rather than THA was chosen as the primary implantation. A posterior surgical approach was used. The bipolar femoral head is stabilized with cement during procedure. The post-operative Xray showed unremarkable position of the prosthetic components. Unfortunately the introprosthetic dislocation occurred twice afterward and the bipolar head had to be exchanged for a new one from another manufacturer.
The dislocation of the bipolar head-cup is rare reported. Once it is happen, the conservative non interventional treatment for dislocation is not recommended [18,19]. The medical literature reports few cases of post-HA complication [5]. The true incidence of the HA complication is unknown. The clinical presentation includes acute dislocation, groin or buttock pain, limited range of motion, shortening of the leg, and external rotation. Dissociation following hemiarthroplasty may occur secondary to trauma, maneuvers of closed reduction after periprosthetic dislocation, or spontaneously. The etiology and type of bipolar components dislocation was described by researchers [5,18,19].
To the best of our knowledge, this is the first reported case of a refractory prosthetic dislocation in one HA patient possibly due to multiple risk factors. The appropriate management of this type of prosthetic hip dislocation is to change the head and cup with the same caliber customized for the specific patient. The medical team should be familiar with features of different implants and patient’s requirement. Optimizing the prosthetic design and quality control may help to prevent such catastrophic complication. In conclusion, the “bottle opener” and the stress on hip various positions and the soft tissue tension and the implant locking design should be considered.
Ethics approval and consent to participate
The Jinan central hospital ethics committee approved to use the data of the patient and the patient consent to participate too.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Competing interests
The authors declare that they have no competing interests.
Funding
Not applicable.
Author’s contributions
Zhenhua Li and Haiying Yu wrote the draft of the manuscript and participated in the follow-up examination of the patient and clinical material. Yuyuan Zeng, Zhen Yang and Yihang You participated in the surgical and medical treatment and followed up the patient. They also have been involved in drafting the manuscript or revising it critically. Tao Zhang performed the surgery, coordinated and helped to draft and finalizes the manuscript. All authors read and approved the final manuscript.
Authors’ information
Tao Zhang is the associate Director of Department of Joint Surgery in Jinan central Hospital.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Li Z, Yu H, Zeng Y, Yang Z, You Y, Zhang T (2023) Recurrent Dislocations of Bipolar Components: A Rare Complication of Bipolar Femoral Head Replacement. Trans Med. 13:289.
Received: 15-May-2023, Manuscript No. TMCR-23-24185; Editor assigned: 18-May-2023, Pre QC No. TMCR-23-24185 (PQ); Reviewed: 01-Jun-2023, QC No. TMCR-23-24185; Revised: 08-Jun-2023, Manuscript No. TMCR-23-24185 (R); Published: 15-Jun-2023 , DOI: 10.35248/2161-1025.23.13.289
Copyright: © 2023 Li Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.