
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2021)
Background: The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an emerging infection causing a widely spread pandemic of Coronavirus disease 2019 (COVID-19). The current COVID-2019 pandemic is prompting fear of falling sick, dying, helplessness and stigma so urgent and timely understanding of mental health status is needed to help the community. The aim of our study is to assess the psychological impact of COVID-19 pandemic on medical students in Sudan.
Materials and methods: A cross-sectional descriptive research was done among medical student in Sudan during COVID 19 pandemic in August 2020. DASS-21 scales were used to determine the level of depression, anxiety and stress among medical students through an online questionnaire; their responses were taken relatable to 21 items of DASS scale. The data was analyzed by means of SPPS version 25.0.
Results: The mean (SD) age of our study participants was 21.8 (2.4) with female to male ratio of 2.1. Most of the participants were residing during the time of the study in middle stats of Sudan (50.8%) and 83% were staying with their families. Interestingly, more than 40.5% of the study participants were free of depression while more than 13% had extremely severe depression. On the other hand, only 4.4% had extremely severe stress. However, anxiety ranked the higher numbers with 23% had extremely severe anxiety. Adjusted linear regression model revealed that lower levels in the medical school and open colleges during the lock down period were associated with more anxiety (p value 0.01,0.006 respectively), while having a family member working in the medical field is associated with less stress (p-value 0.02).
Conclusion: Our study provides good idea about the magnitude of the psychological burden upon medical students during the COVID-19 pandemic and showed many factors that can influence mental health so as to emphasize the need to adopt new strategies to improve psychological services. In addition, it's important to support high-risk groups especially those with preexisting mental illness to offer advanced psychological interventions. So our study can be used to construct and formulate a psychological intervention and implement mental health strategies directed toward vulnerable groups during the COVID-19 epidemic.
COVID-19; Psychological impact; DASS 21; Epidemic
At the end of 2019, a novel coronavirus (COVID-19) was identified as the cause of a severe acute respiratory syndrome (SARS cov-2) cases in Wuhan, a city in the Hubei Province of China [1]. It has started to spread resulting in an epidemic throughout China, then evolving into a full blown pandemic throughout the world [2]. It was declared as a public health emergency of an international concern by the World Health Organization (WHO) on January 30, 2020 [3]. Case counts of COVID-19 globally exceeded 19 million. COVID-19 continued to spread, eventually reaching Africa and Sudan [4]. The total number of COVID-19 cases in Sudan were 13535 with the first case of COVID-19 pandemic in Sudan identified on 13.3.2020 while deaths were 836 since the first case which died was of a 50 years old man and most of the cases were in Khartoum state followed by Gazera State and this is according to the latest report generated from federal ministry of health, Khartoum, Sudan [4]. In Sudan, as elsewhere in Africa, the COVID-19 crisis has unfolded relatively slowly. This is due to the country’s comparative isolation from world travel and the fact that most Sudanese live in rural areas where social distancing is an established practice, but as the virus now appears to be sweeping through Sudan [5]. Sudan is currently struggling with many obstacles as a result of the ensuing pandemic and measures that adopted urgently to control the spread including statewide lockdown, dealing with a collapsing health system and suspension of tuition in schools and universities so stopping the educational process [6]. People in lockdown also are struggling different situations but more importantly, they struggle to cope psychosocially with the circumstances created by the COVID-19 pandemic. Fear, worry and stress are normal responses to perceived or real threats and at times when we are faced with uncertainty or the unknown. So it is normal and understandable that people are experiencing fear in the context of the COVID-19 pandemic [6]. So, this pandemic not only a life-threatening but it imposes a huge psychosocial trauma. Mental health is fundamental to our collective and individual ability as humans to think, express emotions, interact, earn a living and enjoy life. On this basis, the promotion, protection and restoration of mental health can be regarded as a vital concern of individuals, communities and societies throughout the world [7]. The most affected populations with mental health unfortunately were students due to concerns about their future and uncertainty of how to continue the educational process. The leads of education could mitigate this negative effect by updating their students regarding their future, upcoming courses and even the whole educational process. Unfortunately this was not the case in Sudan due to unavailability or un-readiness of the electronic education during the beginning of the pandemic, and then the students would continuously worry so that their mental health is greatly affected. Mental disorders during pandemic was one of the most important issues, the things guide a lot of people to take in consideration and to flash light upon it by numerous paper and survey to detect the action of community, and we as medical student tend to take it from medical students perspective [8]. There is sparse literature about psychological impact of this emergic pandemic upon students so studies were needed to be done due to lack of previous similar studies. Our study provides a good idea about the magnitude of the psychological burden during COVID-19 pandemic upon medical students and showed many factors that can play a role in student's mental health so as to emphasize the need to adopt new strategies to improve psychological services. In addition to identify high-risk groups in order to offer advanced psychological interventions to help them, so the finding of our study can help in implementation of advanced mental health strategies directed toward vulnerable groups to improve their mental health during the COVID-19 epidemic.
This was a cross-sectional design to assess the psychological impact of COVID-19 pandemic in medical students in Sudan. We used an online-based questionnaire distributed through social media apps like WhatsApp, Facebook and Telegram, participants were encouraged to distribute the survey. Physical distribution was not achievable due to the lockdown in Sudan. We shadowed an online data collection technique. The survey was done online by using a common platform, Google survey (Google LLC, Mountain View, California, USA). In order to determine the level of depression, anxiety and stress among medical students, DASS-21 scales were used. It is a 21-item short version instrument specifically designed to determine the three negative emotional states among people which include depression, anxiety and stress. It is proven to be exceptionally reliable with strong internal consistency [9]. Informed consent was taken from all the respondents. The data was analyzed by means of SPPS version 25.0.
The mean (SD) age of our study participants was 21.8 (2.4) with female to male ratio of 2.1. Most of the participants were residing during the time of the study in middle stats of Sudan (50.8%) and 83% were staying with their families. About 79% of the participants had stable monthly income either from their families or by themselves. Regarding the sources of COVID-19 updates, social media was the most used source with more 46% using it followed by news media 26%. More details about participant's demographics and characteristics in Table 1. Interestingly, more than 40.5% of the study participants were free of depression while more than 13 had extremely severe depression. On the other hand only 4.4% had extremely severe stress. However anxiety ranked the higher numbers with 23% had extremely severe anxiety (Figure 1).
| Participant’s Characteristics | |
|---|---|
| Age mean (SD) | 21.8 (2.4) |
| Gender N (%) | |
| Male | 84 (32.3) |
| Females | 176 (67.7) |
| Residence N (%) | |
| North states | 9 (3.7) |
| East states | 101 (41.7) |
| Middle states | 123 (50.8) |
| South states | 1 (0.4) |
| West states | 8 (3.3) |
| Medical school level N (%) | |
| 1st | 60 (23.1) |
| 2nd | 34 (13.1) |
| 3rd | 59 (22.7) |
| 4th | 42 (16.2) |
| final | 65 (25) |
| Living situation N (%) | |
| With family | 216 (83) |
| Away from family | 44 (17) |
| Family/individual income N (%) | |
| Steady income | 206 (79.2) |
| Unstable income | 54 (20.8) |
| Participants who have Family member/members working in the medical field N (%) | 97 (37.3) |
| Participants who have family member/friends contacted COVID-19 cases N (%) | 36.9 |
| Participants who preceded medical schools during lock down period N (%) | 25 (9.6) |
| Participants who were diagnosed with psychological disorders N (%) | 60 (23.1) |
| Sources of COVID-19 updates N (%) | |
| Social media | 121 (46) |
| News media | 24 (9) |
| Both social and news media | 105 (40) |
| Don’t follow updates | 10 (3) |
Table 1: Participant’s characteristics.
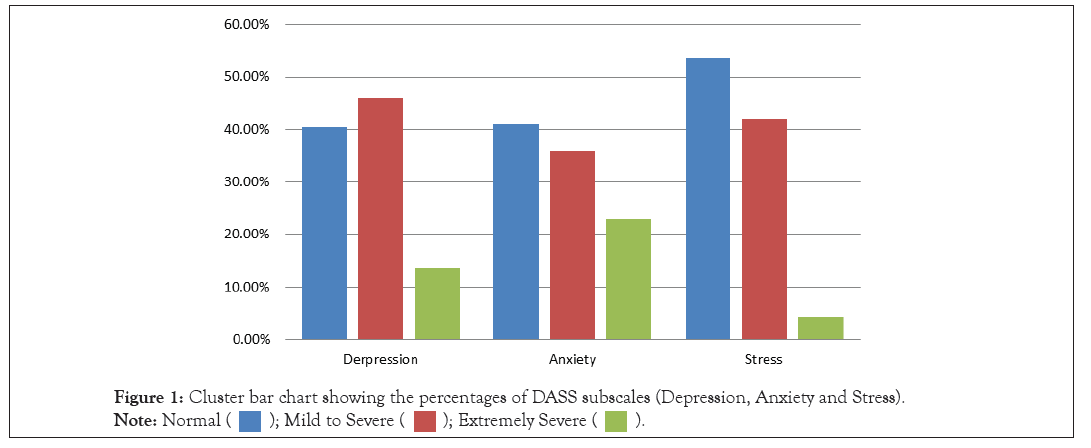
Figure 1: Cluster bar chart showing the percentages of DASS subscales (Depression, Anxiety and Stress). Note: Normal
When comparing DASS subscales between demographics groups, medical schools which opened their doors during the lock down period had students with higher depression, anxiety and stress scores (p-value>0.05), while students in the second grade had the most anxiety score (p value 0.02) (Table 2).
| Depression | Anxiety | Stress | ||||
|---|---|---|---|---|---|---|
| Mean (SD) | P-value | Mean (SD) | P-value | Mean (SD) | P-value | |
| Gender | ||||||
| Males | 7.4 (5.7) | 0.59 | 6.0 (5.0) | 0.77 | 7.5 (5.4) | 0.65 |
| Females | 6.8 (5.1) | 5.8 (4.8) | 7.2 (5.3) | |||
| Living status | ||||||
| With parents | 6.9 (5.1) | 0.99 | 5.8 (4.8) | 0.82 | 7.3 (5.3) | 0.99 |
| Away from parents | 7.4 (6.5) | 6.2 (5.4) | 7.4 (5.9) | |||
| Income | ||||||
| Steady | 6.9 (5.4) | 0.92 | 5.7 (5.1) | 0.15 | 7.2 (5.4) | 0.4 |
| Non steady | 6.9 (5.2) | 6.3 (3.9) | 7.8 (5.2) | |||
| Medical schools status during lock down | ||||||
| Open | 9.1 (5.2) | 0.03 | 8.9 (6.2) | 0.01 | 9.3 (5.7) | 0.05 |
| closed | 6.7 (5.3) | 5.5 (4.6) | 7.1 (5.3) | |||
| Medical school level | ||||||
| 1st | 6.8 (5.5) | 0.31 | 6.2 (4.4) | 0.02 | 7.2 (4.8) | 0.29 |
| 2nd | 7.3 (5.0) | 7.5 (5.9) | 7.9 (5.0) | |||
| 3rd | 7.2 (4.7) | 6.1 (4.7) | 7.4 (5.5) | |||
| 4th | 7.9 (5.4) | 6.4 (5.1) | 8.4 (5.8) | |||
| final | 6.2 (5.9) | 4.2 (4.3) | 6.3 (5.6) | |||
| Media | ||||||
| Social media | 6.8 (5.2) | 0.09 | 6.1 (4.9) | 0.59 | 7.4 (5.5) | 0.26 |
| News media | 6.5 (5.3) | 6 (4.7) | 7.1 (4.9) | |||
| Both | 7.4 (5.5) | 5.7 (5) | 7.4 (5.4) | |||
| None | 2.8 (3.0) | 4 (1.7) | 3.7 (2.9) | |||
Table 2: Depression, anxiety and stress scores among the demographic groups.
Adjusted linear regression model revealed that lower levels in the medical school and open colleges during the lock down period were associated with more anxiety (p-value 0.01, 0.006 respectively), while having a family member working in the medical field is associated with less stress (p value 0.02) (Table 3).
| Depression | Anxiety | Stress | |||||||
|---|---|---|---|---|---|---|---|---|---|
| β (95% CI | Std β | P-value | β (95% CI) | Std β | P-value | β (95% CI) | Std β | P-value | |
| Gender | -0.66 (-2-0.7) | -0.1 | 0.35 | -0.1 (-1.3-1.1) | -0.01 | 0.8 | -0.5 (-1.8-0.9) | -0.04 | 0.5 |
| Current residence | -0.2 (-1-0.7) | -0.03 | 0.7 | 0.6 (-0.2-1.3) | 0.09 | 0.2 | -0.2 (-1.1-0.7) | -0.3 | 0.6 |
| Previous psychological disorder | 3.6 (2.1-5) | 0.8 | >0.001 | 3.3 (1.9-4.6) | 0.3 | >0.001 | 4.1 (2.6-5.6) | 0.3 | >0.001 |
| Livening status | 0.8 (-2.4-0.9) | 0.06 | 0.4 | -0.9 (-2.4-0.6) | -0.1 | 0.2 | -0.6 (-2.2-1.1) | -0.04 | 0.5 |
| Medical school level | -0.1 (-0.5-0.4) | -0.2 | 0.7 | -0.5 ((-0.9)- (-0.1)) |
-0.2 | 0.01 | -0.1 (-0.5-0.3) | -0.03 | 0.7 |
| Medical school status | 1.6 (-0.3-3.6) | 0.1 | 0.1 | 2.5 (0.7-4.30) | 0.2 | 0.006 | 1.5 (-0.7-1.1) | 0.1 | 0.08 |
| Family member working in the medical field | -1 (-2.3-0.3) | -0.1 | 0.1 | -0.9 (-2.1-0.3) | -0.1 | 0.2 | -1.6 ((-2.9)-(-0.3)) | -0.2 | 0.02 |
Table 3: Adjusted linear regression model of depression, anxiety and stress scores.
This study was conducted to assess the degree of psychological impact among medical students during the pandemic since this emerging infection had a great impact in prompting fear and other feelings due to contagiousness of COVID-19 and lockdown so that mental health of the people is greatly affected. This crisis is one of the most challenging threats to mental health so we use DASS scale and it specifically designed to determine the level of the three negative emotional states among people which include depression, anxiety and stress [10].
We found that more than 40.5% of the study participants were free of depression, about 41% were free of anxiety and about 53% were free of stress and these good percentages may be attributed to good perception and fully awareness of the outbreak so that good psychological health. Our finding was similar to recent study done to assess the psychological impact of COVID-19 pandemic on the general population of Saudi Arabia where 59.1% had normal scores on the depression subscale, 70.1% had normal scores on the anxiety subscale and 70.2% had normal scores on the stress subscale [11]. On the other hand, our study showed that more than 13% had extremely severe depression; only 4.4% had extremely severe stress while anxiety ranked the higher numbers with 23% had extremely severe anxiety. In Saudi study, severe symptoms of stress were experienced by 13.7%, which is similar to the 13.9% who experienced severe symptoms of anxiety and 16.4% who experienced severe symptoms of depression [11]. Our participants experienced lower level of stress may be due to good awareness about COVID-19 that may prevent the stress. In another study done in China, 16.5% reported moderate to severe depressive symptoms; 28.8% reported moderate to severe anxiety symptoms; and 8.1% reported moderate to severe stress levels [12]. This finding was in alignment to our study where the anxiety levels ranked the higher numbers meaning that the pandemic comprises such an event which urge the person get anxious about it. In another study done in China about the psychological impact of the COVID-19 epidemic on undergraduate medical students since they feel an overwhelming sense of duty to support their National Health Service (NHS), but the fear and anxiety of what they are to face is not eased and even may become worse by the large number of erroneous news reports [13].
The mean (SD) age of our study participants was 21.8 (2.4) with female to male ratio of 2.1, similar to Saudi study where the majority of the participants were females (63.9%) [11]. In our study, the gender was not influencing the DASS subscales because the perception of the event was not differ by gender difference since they were medical students, in contrary to Saudi study which is done in general public where the female gender was associated with higher scores in all three sub-scales of the DASS [11]. Also in China, female gender was significantly associated with a greater psychological impact and higher levels of stress, anxiety, and depression (p<0.05) [12].
About 79% of the participants had stable monthly income either from their families since they were students yet or by themselves. In our study, income whether steady or not did not influence the DASS subscales so that it does not affect the psychological heath, but this is not follow the logic since the economic impact of the pandemic cannot be overlooked because it had made families with lower income fearing of losing their jobs and even homes due to long period of lockdown with no jobs and so no source of income. In contrast, Saudi study showed that earning less than 5000 SAR was significantly associated with higher scores on depression subscale of the DASS [11].
Regarding the sources of COVID-19 information and updates, social media was the most used source by our participants with more 46% using it followed by news media 26%, while the majority of Saudi participants sourced their information from the Saudi Ministry of Health (87.2%), the World Health Organization (40.9%) and non-official social media applications and platforms such as WhatsApp, Twitter, YouTube, etc. (40.3%). In our study, the information sources had no significant associations with DASS scores, meaning that regardless of how the information reached to someone it does not affect the reliability of psychological impact. In Saudi study, participants who sourced their information from the World Health Organization were significantly more likely to have worse scores across DASS stress, anxiety and depression subscales. Relying on local news was significantly associated with lower scores on the DASS-anxiety. All other information sources had no significant associations with DASS scores [11].
Participants who have family member/members working in the medical field were 37.3%, and this was near to 27.9% of Saudi participants who had family members worked in the medical field and only a small proportion did work in a medical field 11.7% [11], since our participants were medical students. In Saudi study, working in the medical field or having a family member who works in the field was associated with higher scores on the DASS. When participants worked in the medical field, they were more likely to have higher scores on the stress and depression subscales of the DASS. When they had family members who worked in the medical field, they were more likely to have higher scores across all three subscales of the DASS [11]. This finding was not in line with our study where adjusted linear regression model revealed that having a family member working in the medical field is associated with less stress (p value 0.02) and this may attributed to good perception and conception about COVID-19 so they not put themselves in stress. In a study done in Sudan aimed to investigate the psychological impact of COVID-19 pandemic on frontline medical staff and healthcare workers in Khartoum state, the majority (80.1%) of their participants stated that their families are worried and afraid that they will transmit the disease to them. About (35.4%) of their participants thought that people started to avoid them because of the nature of their job, and (62.9%) of them stated that their income got lowered during the COVID 19 pandemic, while (65.6%) thought that their working hours were increased during this time and all of these determinants would affect them psychologically since they were placed in a stressful condition due to the uncertainty about the mode of transmission of the disease, tremendous fear, and implementation of rigorous infection control protocols and most of their participants were found to be suffering from anxiety and depression [14].
Participants who were diagnosed with psychological disorders were 23.1%. 10.5% of Saudi participants had been diagnosed to have a psychiatric disorder and it was significantly associated with higher scores on all the scales of DASS [11]. This is in line with our study where previous diagnosis with psychological disorder was significantly associated with all subscales of the DASS. In Chinese study among medical students, 24.9% anxiety occurrence may have been exacerbations of pre-existing mental health issues rather than new onset problems. The prevalence of mental health problems in Chinese medical students suggested that mental health issues are more prevalent within the medical field [13].
Our study showed that participants who preceded medical schools during lock down period were 9.6%. Moreover, medical schools which opened their doors during the lock down period had students with higher depression, anxiety and stress scores with p value of 0.03 for depression, 0.01 for anxiety and 0.05 for stress and all are considered statistically significant. Also, our study showed that students in the second grade of medical school had the most anxiety score with p value of 0.02 and this again considered statistically significant. Adjusted linear regression model in our study revealed that lower levels in the medical school and open colleges during the lock down period were associated with more anxiety (p-value 0.01, 0.006 respectively). Our finding was not in line with a study done in China among medical students, where medical students transitioning from pre-clinical to clinical years displayed the highest numbers in anxiety, attentional and depressive symptoms and this due to the fact that anxiety levels vary between the younger and older students due to variances in work-load between year groups so that more work-load and pressure in clinical years. In Saudi study since it was conducted among the general public, they found that being a student was significantly associated with higher scores across all three subscales of the DASS. This was congruent with a study done in China where students had higher scores across all DASS subscales. They attributed this to uncertainty of how to continue the educational process after closing up the campuses and schools so this was considered a source of worry. The educational leads can mitigate this by regularly updating their students and colleagues on what is happening regarding the future of their courses. Also, importance of social support and now we are in an era where we can be there for one another, without being physically present.
Limitations of this study include limitations to reach non-social media users since our data was collected using Google forms and this led to less generalizable results. Also, our study provides only a snapshot of psychological responses at a particular point in time, and to know whether the observed impact last for longer periods or not, prospective longitudinal study is required to implement focused mental health strategies. In addition, the self-reported psychological impact may not actually reflect the exact mental health status assessed in an interview. But despite all that, our study provides good idea about the magnitude of the psychological burden upon medical students during the COVID-19 pandemic and showed many factors that can influence mental health so as to emphasize the need to adopt new strategies to improve psychological services and to deliver accurate and evidence-based information to decrease the effect of fake news because the incorrect information in the internet adds negatively to our own health and well-being. In addition, it's important to support high-risk groups especially those with preexisting mental illness to offer advanced psychological interventions. So our study can be used to construct and formulate a psychological intervention and implement mental health strategies directed toward vulnerable groups during the COVID-19 epidemic.
All authors participated in the literature search, manuscript editing and preparation. MEA, AAH and AMB were responsible for draft writing, conceiving the idea for the article and wrote the final manuscript. HHM analyzed the data of this study and participated in draft writing. All authors contributed to and approved the final report.
The authors declare no conflict of interest.
Citation: Omer MEA, Shareef AAH, Al-lahawi AMB, Alhaj HHM, Ali KM (2021) Psychological Impact of COVID-19 Pandemic on Medical Students in Sudan. J Clin Trials. S12:006.
Received: 29-Jun-2021 Accepted: 13-Jul-2021 Published: 20-Jul-2021 , DOI: 10.35248/2167-0870.21.s12.006
Copyright: © 2021 Omer MEA et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.