Journal of Yoga & Physical Therapy
Open Access
ISSN: 2157-7595
ISSN: 2157-7595
Research Article - (2015) Volume 5, Issue 2
Objective: Increasingly, yoga is among the therapies included in recommended multimodal treatment approaches for persons with fibromyalgia. Given the numerous yoga lineages, styles, practice components, and the relatively scant empirical evidence of the effectiveness of yoga therapy for persons diagnosed with fibromyalgia, rigorous studies are needed to support these recommendations. The development of sound methodological designs and protocols to ensure study rigor, enhance replication potential, and synthesize results across studies for establishing evidence-based best practices is needed. Thus, this article presents the design and protocol used in an 8-week intervention study aimed at determining the feasibility of restorative yoga as an appropriate intervention for persons diagnosed with fibromyalgia. A secondary aim was to collect preliminary data on the perceived effects of restorative yoga to inform future fibromyalgia yoga therapy research.
Method: Using a prospective, mixed-methods, single-arm design, the investigators assessed the feasibility of an 8-week restorative yoga intervention for persons diagnosed with fibromyalgia. Twelve (12) persons with physiciandiagnosed fibromyalgia took part in twice weekly, 90-minute restorative yoga group classes and a 20-minute home practice on the five non-class evenings. The Theory of Planned Behavior informed the study design. Quantitative findings for feasibility included recruitment, study completion, and adherence rates during the 8-week intervention and at a 1-month follow-up. These findings were corroborated by qualitative findings from semi-structured pre- and post-intervention interviews. Data regarding the perceived effects of restorative yoga were collected using self-report questionnaires at intervention baseline and at weeks 4 and 8.
Discussion: The study protocol provides a template for future feasibility studies of restorative yoga for persons diagnosed with musculoskeletal conditions, and one that can inform future yoga intervention studies aimed at identifying the most efficacious and feasible yoga style(s) for persons diagnosed with fibromyalgia.
Keywords: Fibromyalgia, Restorative yoga, Yoga, Relaxation response; Mind-body therapies, Protocol, Sleep, Pain, Health-related quality of life, Symptom self-management
The Institute of Medicine characterizes pain as a costly and pervasive condition in the United States that is associated with conditions such as fibromyalgia (FM) [1]. Prevalence rates for FM have been estimated at 2.5% to 7.9% of adults in the United States, with a female to male ratio of 7:1 [2,3]. However, with recent changes in the American College of Rheumatology criteria, diagnostic rates among men have increased [4,5]. FM-related symptoms include chronic widespread pain, sleep disturbance, fatigue, morning stiffness, anxiety, depressed mood, and impaired cognitive function. A diagnosis of FM is made based on the presence of chronic widespread pain that cannot be attributed to any other condition for the duration of 3 months or longer and the assessment of presenting symptoms by a physician using the Widespread Pain Index in combination with the individual’s Symptom Severity Score [5]. For persons diagnosed with FM, these symptoms impact their lives and result in a decreased ability to engage in daily activities, functional decline, and a diminished health-related quality of life (HQoL) [6,7].
The etiology of FM remains unclear; however, research findings support the primary mechanism in FM as a dysregulation of the central nervous system (CNS) [8-10]. CNS and peripheral nervous system changes as well as altered immune and neuroendocrine function are implicated in the widespread pain and other symptoms experienced by those with FM [9,11,12]. Genetics, too, may predispose individuals to development of FM, but environmental and psychological stressors are thought to act as triggers and sustaining factors [8,13,14]. Chronic psychological stress has been implicated as a primary contributing factor to the CNS dysregulation and increased sensitization that occurs [15]. Thus, treatment recommendations for persons with FM include a multimodal approach of both pharmacologic strategies to reduce FMrelated symptoms such as pain, depressed mood, and sleep disturbance, and non-pharmacologic stress-reducing, restorative sleep-enhancing therapies such as yoga and exercise [8,16-18].
Although exercise is a highly recommended treatment modality, those with FM demonstrate a reduced aerobic capacity and diminished strength [19,20]. In addition, some forms of exercise may intensify FM-related pain [21,22]. Given that increases in pain severity have been associated with functional decline in persons with FM [23], it is important to identify exercises that are appropriate for FM-related aerobic and strength limitations and those that do not promote or exacerbate pain. Increasingly, persons with FM are seeking gentle forms of mind-body movement therapies such as yoga to meet their specific exercise requirements [24].
Gentle forms of yoga that incorporate mindfulness practices may be especially useful for treating those with FM because low intensity movement serves to prevent pain-enhancing eccentric and concentric muscle contractions and minimizes energy expenditure while promoting balance and joint mobilization [21,25]. Equally important, the mindfulness practices incorporated into a yoga program may help individuals manage stress and decrease perceived pain severity [26- 28]. One gentle yoga style is restorative yoga (RY), which is noted for its ability to invoke the relaxation response, making it especially well suited for persons diagnosed with FM [29,30]. A typical full RY practice session is designed to move the spine in all directions, promote relaxation of the muscles, increase blood flow and oxygen exchange to the abdominal organs, reverse the effects of gravity, and decrease stress [30]. As opposed to stretching or contracting muscles, RY is designed to support muscles, thereby minimizing the muscle guarding commonly found in chronic pain conditions. A decrease in levels of perceived stress and fatigue and improved sleep quality has been demonstrated using RY for women with ovarian and breast cancer and for women experiencing menopausal hot flushes and associated menopausal insomnia [31-33].
Individual components of RY practice have been investigated as non-pharmacologic means for sleep promotion in competitive athletes [34]. The warm and quiet environment in which RY practices are conducted promotes skin warming, core cooling, and relaxation of skeletal muscles contributing to shortened sleep latency [35]. Repeating a sound or word(s) during a lengthened exhale promotes habituation and sensory withdrawal and nurtures a state of calmness [29,34]. Encouragement to adopt a passive attitude toward thoughts and to focus on one’s breath is an approach used during RY practices to elicit the relaxation response [29]. The dark environment and supine, inverted restorative postures reduce activity of the reticular activating system, resulting in a state of decreased brain arousal [34]. As compared with upright postures, reclining and inverted RY postures stimulate baroreceptor responses, which, in addition to decreasing brain arousal, decrease sympathetic nervous system activity, promote parasympathetic nervous system dominance, and diminish other physiologic responses characteristic of CNS arousal and stress states [36-41]. Given that baroreceptor responses have been shown to be impaired in persons with FM during stress [42], and that this impairment has been implicated in the hyperalgesia and autonomic nervous system dysregulation found in those with FM [42,43], baroreceptor stimulating practices such as RY may be important in FM-related symptom management.
Although investigators report that yoga shows promise for use in FM-related symptom management, only seven articles reporting on six studies were found in the literature [26,27,44-48]. These studies investigated three styles of yoga (“Relaxing” yoga, Yoga of Awareness, and Hatha yoga) for symptom management in FM [26,44,45,47]. Although one study [44] identifies the yoga intervention as relaxing yoga, a yoga therapy delivered as a one-on-one participant to therapist intervention, the description of the intervention given includes stretching and, therefore, is not consonant with a RY practice. Thus, the primary aim of this study was to establish whether or not the practice of an 8-week RY intervention was feasible for persons diagnosed with FM. The secondary aim of this study was to gather preliminary data on the study participants’ perceptions of the effects of RY on the FMrelated symptoms of pain, sleep disturbance, fatigue, functional status, and HQoL. In 2014, accepted and recognized yoga research guidelines did not exist; therefore, recommendations for yoga therapy research proposed by Sherman [49] and the Delphi survey recommendations for yoga therapy research for musculoskeletal disorders by Ward and colleagues [50] guided the design of this study protocol.
Study design
The Theory of Planned Behavior (TPB) [51] provided a heuristic framework for this study design. A mixed-methods, single-arm, prospective design using a concurrent triangulation strategy was used [52]. This sub-study aimed to evaluate the feasibility aspects of an 8-week RY intervention. The larger parent study (PI Taylor) aim was to gather preliminary information on changes in pain processing in the brain related to this 8-week RY intervention in the same group of study participants. Results of the parent study will be reported in a separate article.
Feasibility was operationalized as recruitment, retention, and adherence rates. Resource utilization and intervention safety also were incorporated into feasibility calculations. Pre- and post-interview data were used to help explain observed RY behavior and to identify participant-perceived facilitators and barriers to RY practice. Feasibility has been operationalized similarly in RY intervention studies for women with menopausal hot flushes and for women with breast and ovarian cancer [31-33].
Two 8-week RY intervention sessions were conducted. Self-report outcome measures were completed at intervention baseline and at weeks 4 and 8. Pre- and post-intervention, one-on-one, in-person, audio-recorded interviews and a 1-month follow-up were conducted.
The Institutional Review Board for Health Sciences Research (IRBHSR) for the university approved the study protocol and all study materials. Informed consent was obtained from all study participants prior to their participation in any study activities.
Setting: All group RY classes were held in a room appropriate for a RY intervention [30] at the School of Nursing (SON) within a research-intensive university located in central Virginia. Consent and pre- and post-interview study visits were held in a private room located within research facilities at the same university. Free parking and direct elevator access were available to participants for all study visits.
Study population: A consecutive convenience sample of six persons between the ages of 21 and 75 with physician-diagnosed FM were recruited for each of two 8-week RY intervention sessions. Potential study participants were persons who (a) were being seen in the university rheumatology clinic, (b) agreed to be contacted for future FM studies, or (c) responded by e-mail or telephone to a posting on the university’s clinical trials Web site. All interested persons who contacted the investigators were sent an informational study brochure that included a telephone number to call for study eligibility prescreening. Those persons who contacted the investigators by telephone were prescreened and study eligibility determined according to the inclusion and exclusion criteria listed in Table 1 and, if eligible, a 30-minute consent visit was scheduled. A letter confirming the consent visit date and time, along with a copy of the informed consent document, was sent via e-mail or postal service. Appointment reminders were e-mailed 2 days prior to the appointment and telephone reminder calls were made 1 day prior to the appointment. Persons who declined to participate or those who withdrew from the study were asked to provide their reasons for non-participation or withdrawal voluntarily. Study participant flow is presented in Figure 1.
| Inclusion Criteria | Rationale |
|---|---|
| Adults between the ages of 21 to 75 | A diagnosis of fibromyalgia (FM) is not common in individuals under 21 years. Individuals are generally diagnosed later in life as FM symptoms worsen. FM increases with age, peaking in individuals between 70 to 79 years of age.3 Individuals over 75 years of age are not seen in large numbers in the clinic population and show increased numbers of comorbidities that may have confounded the results of this feasibility study. |
| Diagnosis of FM by a physician (confirmation by physician or by self-report of name of diagnosing physician and years since diagnosis) | Only those individuals who had been diagnosed by a physician were included to establish a confirmed diagnostic baseline for the study. |
| Stable non-steroidal treatment regimen for 3 months or longer prior to the study period start date | Without a stable treatment regimen (i.e., no expected changes in medication and/or dosage during the intervention period), it would not be possible to determine if any effects on pain, sleep, stress, and health-related quality of life were the result of other treatments or the restorative yoga intervention being evaluated. |
| English speaking/writing | This feasibility study did not have the resources necessary to evaluate and accommodate non-English speaking/writing participants. |
| Exclusion Criteria | Rationale |
| Any physical limitation that prevents the person from doing the required RY postures (e.g., spondylolisthesis or spondylolysis, herniated disc disease) | Although many poses can be modified, all participants must be able to do some form of each posture to induce the functional response being sought; numbers of those excluded for this reason were tracked and considered a part of the feasibility calculations for this study. |
| Currently pregnant | Many yoga poses are not safe for pregnant women, and hormones are thought to play a role in the mechanisms of FM; therefore, the hormones present during pregnancy could potentially alter outcomes. |
| Current diagnosis or history of diagnosis of bipolar disorder or schizophrenia | Yoga mindfulness practices may increase the potential for a negative psychological event and thus require instructors skilled in the treatment of these disorders. |
| Current use of steroids | Inflammation is suggested to be involved in the mechanism of FM. By reducing inflammation in the body, the use of steroids has the potential to alter the outcomes for pain and sleep, confounding the results of this study. |
| Mindfulness or yoga practice 2 or more times per week for 6 months or more within the past 3 years | Recent or current mindfulness or yoga practice may confound the study findings. |
Table 1: Inclusion and Exclusion Criteria and Rationale.
Study participant compensation: Study participants were compensated $20 per study visit, which was paid incrementally at four protocol-designated time points and in accordance with the guidelines for payment to human subjects.
Yoga instructor and assistants qualifications and training: All yoga classes were taught by a registered nurse who is a registered yoga teacher with Yoga Alliance and a certified Relax and Renew® Trainer for RY. Relax and Renew® is the service mark associated with Judith Lasater’s RY training. The yoga instructor is an experienced yoga practitioner who has taught both healthy persons and those with chronic disorders, including musculoskeletal conditions. The yoga instructor taught the class assistants, who also had nursing and research expertise, the principles of RY. During the two 8-week sessions, the assistants set up for the class sessions, collected and reviewed for clarity and completeness all completed study materials, took participants’ preand post-class pulse and respiration rates, and assisted participants with RY posture transitions.
Treatment fidelity: The yoga instructor and assistants used a RY training and class manual designed by the first author. Prior to contact with study participants, assistants attended a 3-hour training class, completed assigned readings [29,30,34], and demonstrated a grasp of RY positioning. The yoga instructor conducted all classes according to a script. Sequencing and timing of postures remained the same for every class. To ensure a consistent RY dose, a stopwatch was used to time the RY postures. The yoga instructor and assistants each took the pulse and respiratory rates and assisted the same two participants over the entirety of the 8-week intervention. The yoga instructor maintained a class attendance log. One of the assistants (KA) observed the yoga instructor for intervention delivery fidelity throughout the 8-week session and, along with the yoga instructor, monitored study participants for Adverse Events (AEs). Individual deviations from the intervention protocol during a class, posture modifications, or other treatment fidelity issues were noted in a log maintained by the yoga instructor. The yoga instructor and assistants met briefly after each class to discuss any posture modifications needed and to resolve any challenges that may have occurred during the class session.
All study participants attended an orientation class during which the yoga instructor provided instructions for both class and home practice. Participants were instructed in centering, breath/body awareness, asana, and pranayama. Individual posture modifications were determined and participants’ questions were answered. The yoga instructor and assistants observed the study participants, giving feedback and assistance as needed to ensure that they were able to perform the RY class and home postures and practices. Treatment fidelity also was assessed during weekly telephone calls.
AE reporting: For this study, an AE was considered to be any undesirable sign, symptom, or medical condition considered related to the RY intervention. Medical conditions/diseases present before starting the intervention were considered AEs only if these worsened after starting the study and that worsening was considered to be related to the RY intervention. An AE was also any undesirable and unintended effect of the research occurring in human subjects as a result of the collection of identifiable private information for the study. The yoga instructor and assistants monitored participants for AEs during the twice-weekly group RY classes. The yoga instructor monitored for AEs during the weekly telephone calls to the participants. Adverse events, had any occurred, would have been reported to the IRB-HSR office in the appropriate time period based on the severity of the event and in accordance with the IRB-HSR guidelines.
Intervention
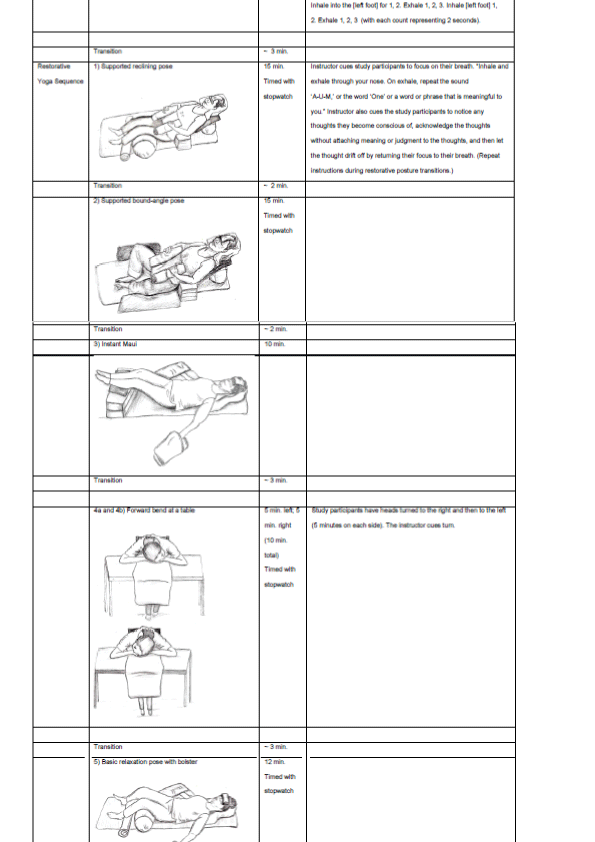
Study participants continued to receive their usual medical care during the intervention period and were asked not to begin any new therapies for the duration of the RY study period. The RY intervention consisted of one 90-minute orientation session followed by 8 weeks of twice-weekly 90-minute group classes and one 20-minute home practice 5 days a week on non-class days. The 90-minute class sequence consisted of centering and breath/body awareness exercises followed by a 75-minute sequence of five RY postures (asanas) that incorporated 3 minutes of a yoga breathing technique (pranayama).
Pulse and respiration rates were taken before and after each of the RY class sessions to assess the extent that the relaxation response was achieved during the RY practice [29,53]. Classes were held each week on Monday and Thursday between 5:30 and 7:00 P.M., which met the Delphi survey key component recommendations for minimum dose, duration, and frequency of a yoga intervention for a musculoskeletal condition [50].
The home practice consisted of (a) basic relaxation pose with a bolster, which participants were asked to do at approximately the same time each day, immediately prior to their bedtime, and (b) recording in their daily logs (1) the length of each RY practice and (2) how they felt before and after each practice. The key component recommendations for home practice are 3 times per week for 30 minutes [50]. This study used a 20-minute home practice 5 times per week. The 20-minute practice time was purposefully selected based upon RY practice principles and the time necessary to elicit the relaxation response [29,30,54].
The class postures and sequence, designed by the first author, were adapted for persons diagnosed with FM from the RY practice for insomnia published by Judith Lasater [30]. The selection of the insomnia sequence and the late afternoon and evening timeframes to engage in RY were purposefully selected to address the FM-related symptoms of fatigue and sleep disturbance and the bi-directional association between disturbed sleep and perceived increase in pain severity [55-57]. The RY posture and sequence selection were based on the ability of study participants to safely and easily move from one posture to another. Any posture modifications, to the extent necessary, were implemented on the basis that the modified posture would have an equivalent functional purpose to that of the sequence posture. RY postures are considered safe and have few contraindications. Comorbid conditions were assessed for each participant and individual modifications were made as needed. The nomenclature identifying the postures in the intervention is the same as that used in Relax and Renew® training. To the authors’ knowledge, no studies have reported using RY for musculoskeletal conditions.
RY props used in the group class sessions included yoga mats, bolsters, towels, blankets, sand bags, petite eye pillows, and standard size eye pillows. Each participant’s props were stored separately between the class sessions. Petite eye pillows were distributed for home use. At the orientation class, a demonstration was given showing study participants how to use items at home as RY props for the home practice (e.g., comforters, blankets, pillows, towels). Each participant received a home practice manual showing step-by-step instructions for proper postural alignment and positioning of the basic relaxation pose using a bolster. Participants were encouraged to create a dedicated quiet RY practice space in their homes where the home practice setup could remain throughout the 8-week intervention.
Participants were assigned a mat space, a place at a table, and a chair with arms for each class. Prior to each class session the instructor and assistants set up the mats for the first RY posture, making provisions for modifications for individual physical needs and limitations. Upon arrival, study participants sat in their designated seats and entered their pre-practice data in their practice logs. At 5:30 P.M. the class session commenced. During class, the yoga instructor and assistants aided the participants in assuming each posture, giving attention to postural alignment and comfort. The yoga instructor tracked individual posture modifications. After completion of the 90-minute class and assessment of post-intervention pulse and respiration rates, the participants were asked to lie on their side for 5 to 6 complete breaths, then come to a seated position for 5 to 6 complete breaths, and then stand and return to their designated chairs and tables to fill out the post-practice portion of their weekly practice logs. Class details are presented in Table 2.
Outcome measures
Outcome measures for this study protocol were selected in accordance with the study aims and recommendations of the Outcome Measures in Rheumatology (OMERACT) working group for FM. OMERACT recommendations for assessments in all FM studies include the core domains of pain, tenderness, fatigue, sleep disturbance, and patient global multidimensional function [58]. In addition, the selection of outcome measures was informed by the Delphi survey guidelines for musculoskeletal disorders [50], use and reliability of the outcome measure in past FM research, ease of completion, and study participant burden (defined as time required to complete the questionnaire).
Baseline assessments: Baseline assessment self-reported demographic and health history information that included a listing of all current medications was collected using an investigator-developed paper form.
Primary outcome measures: Primary outcome measures were defined as rates of recruitment, retention, and adherence as well as resource utilization and safety of the RY intervention for persons diagnosed with FM. Study participant-perceived acceptability and continued practice at the 1-month follow-up telephone call were also included in the feasibility assessment.
Recruitment. Recruitment was defined as the number of potential participants screened for study eligibility versus the number of persons who enrolled in the study. Two [26,45] of six [26,44-48] identified yoga intervention studies for persons with FM have reported recruitment rates: one at 82.8% [26] and the other at 38.6% [45]. Therefore, a recruitment rate above 40% was considered an acceptable rate to support this aspect of feasibility.
Retention. Retention was defined as the number of participants enrolled who completed the 8-week RY intervention and all study measures. Attrition rates for studies of yoga interventions in persons with FM have ranged from 14% to 40% with a mean of 25.35% ± 10.57% [26,44-46]; therefore, a retention rate ≥ 75% was considered an acceptable retention rate to support the feasibility of the RY intervention.
Protocol adherence. Adherence to the study protocol was determined by class attendance rates and participants’ home practice rates as reported in their daily practice logs. Adherence to home practice and class attendance was encouraged during the weekly telephone calls. Reasons for missing classes or non-adherence to home practice were tracked. Rates of class and home practice adherence have not been well documented in previous FM and yoga studies. Two studies reported class adherence rates of 87.5% [26] and 86% [45], but no rates of home practice adherence have been reported. Thus, an adherence rate of ≥ 80% for the RY group class was considered indicative of intervention feasibility. Given the lack of home practice data, the class adherence rate of ≥ 80% was used for the home practice parameter, too.
Resource utilization. Costs associated with conducting the RY intervention and feedback from the yoga instructor and assistants were included in feasibility calculations. Feasibility related to staffing requirements for the full 90-minute RY intervention practice as an at-home symptom self-management strategy or in a community class setting was operationalized as the ability to transition independently between RY postures by the end of the 8-week intervention and performing the 90-minute class practice at home once the 8-week intervention period had ended.
Safety of the RY intervention. The occurrence or non-occurrence of an AE and the number and types of AEs determined safety of RY for persons diagnosed with FM.
Perceived feasibility. Perceived feasibility was based on participantidentified facilitators and barriers, the types and number of these, and on participants’ levels of satisfaction with the RY intervention.
Descriptive data collection: Pre- and post-intervention, one-onone audio recorded interviews were used to gain a perspective of those living with FM and their experiences of participating in the 8-week RY intervention. Semi-structured sample interview questions assessed predictors of behavior according to the TPB. Questions were developed to capture data about the participants’ (a) behavioral beliefs of RY based on knowledge or experience, (b) perceived and actual behavioral control regarding their participation in the RY class sessions and home practices and use of RY as a means of symptom self-management, and (c) perceptions of societal attitudes and beliefs and the beliefs and attitudes of those around them that influenced their behavior during the 8-week RY intervention (Table 3).
| Pre-Intervention Interview Questions | Post-Intervention Interview Questions |
|---|---|
| 1. What are your thoughts on complementary healing approaches such as restorative yoga for persons like yourself? 2. What comes to mind when you think about having fibromyalgia? 3. What comes to mind when you think about yoga as an intervention to aid you in symptom control; about restorative yoga? 4. Have you ever practiced yoga or seen it practiced? 5. What do you think will happen during the 8-week restorative yoga study? How do think it might make you feel physically and mentally? 6. What are some of the things that might motivate you to be more active? 7. Do you think the people who are important to you support your participation in the restorative yoga study? Yes ___ No___ Explain 8. In the past, have you been able to participate in an activity that was helpful? If yes, please describe that activity. |
1. Tell me about your experiences with the restorative yoga sessions. 2. Tell me about your motivation level throughout the 8 weeks of restorative yoga sessions. 3. Did you experience any barriers to continuing in the study during the restorative yoga sessions? If yes, what were these? 4. What symptoms, if any, did you experience following the restorative yoga sessions? 5. What did you enjoy most about the restorative yoga sessions? What did you enjoy the least? 6. Did your initial impression of restorative yoga change over the course of the 8 weeks of restorative yoga sessions? 7. What future plans do you have related to restorative yoga? 8. If you had the opportunity, would you recommend restorative yoga to others with fibromyalgia? |
Table 3: Pre- and Post-intervention Semi-structured Interview Questions.
Secondary outcome measures: Secondary outcome measures provided preliminary data on participants’ perceived effects of RY on FM-related symptoms. These measures, completed at baseline and at weeks 4 and 8, included self-report questionnaires that incorporated the recommended OMERACT core domains for research studies of persons diagnosed with FM [58].
Treatment Expectancy Scale. The pre-intervention Treatment Expectancy Scale is a 3-item questionnaire of participants’ expectations of the 8-week RY intervention. Participants responded to 3 questions: (1) Do you think the RY intervention as described will help reduce your pain, stress, negative emotion, fatigue, and sleep disturbance (yes or no); describe why or why not? (2) How confident are you that RY will be successful in improving your FM symptoms (11-point Likert scale where 0 = not at all confident to 10 = very, very confident)? and (3) What degree of improvement do you expect from the RY intervention (11-point Likert scale where 0 = no improvement in symptoms to 10 complete improvement in symptoms)? The higher the total score (range 0 to 20), the higher the level of outcome expectancy [59].
The post-intervention Treatment Expectancy Scale is an 8-item questionnaire of participants’ experiences and expectations following the 8-week RY intervention. Using a 10-point Likert scale (1 to 10 where 1 = not at all, none, or no improvement and 10 = extremely, complete improvement, complete relief, or complete reduction in symptoms), participants answered six questions: (1) How logical does this type of treatment seem to you? (2) How confident were you at the beginning of the study that the treatment would be successful? (3) How confident would you be in recommending RY to a friend with FM? (4) What degree of improvement did you expect from RY? (5) Before beginning the RY sessions, how much change in your FM symptoms did you expect from the RY sessions? and (6) After beginning the RY sessions, how much change did you expect? (7) Do you believe you received any benefit from the RY 8-week intervention, yes or no? (8) If yes, describe the perceived benefits resulting from completing the RY sessions.
Revised Fibromyalgia Impact Questionnaire (FIQR). The FIQR is an updated version of the Fibromyalgia Impact Questionnaire (FIQ) consisting of 21 questions intended to assess perceived FM-related impact on the participants’ daily life over the past 7 days [60-62]. Using an 11-point numeric rating scale (0 to 10 with 10 being the worst outcome for each question or situation assessed), participants ranked three linked domains: functional status (9 questions), overall impact (2 questions), and symptoms (10 questions). The combined score of these three domains indicates the individual’s perceived overall HQoL [62]. Validation and reliability of the FIQR has been established [62].
Numeric Rating Scale for Pain (Pain NRS). Pain intensity was measured using the Pain NRS. Using an 11-point scale (0 = no pain to 10 = worst pain imaginable), participants responded to three questions: (1) intensity of present pain; (2) average pain intensity over the past week; and (3) worst pain intensity experienced during the past week. The Pain NRS has been used in studies comparing clinical and evoked pain measures in individuals diagnosed with FM and has been found to be a simple, reliable, and sensitive measure of pain intensity [63].
Numeric Rating Scale for Stress (Stress NRS). Perceived levels of stress were measured using the Stress NRS. Using an 11-point scale (0 = no stress to 10 = worst stress imaginable), participants rated their perceived average level of stress that day. The Stress NRS has been used in research of individuals with FM and has been found to be a reliable and valid measure of perceived stress levels for this population [64].
Short Form 36v2 (SF-36v2™). The SF-36v2™ was used to assess the participants' perceived health and well-being based upon its 36- item questionnaire, which is a reliable and valid generic measure of perceived functional health and well-being [65-67]. Eight subscales (physical function, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health) are grouped into two summary measures (physical health and mental health).
Daily Stress Inventory (DSI). The DSI, a measure of perceived daily stress, is a 58-item, self-report questionnaire used to assess the occurrence and perceived level of stressfulness of a variety of events. Reliability and validity of the DSI has been established [68,69].
General Sleep Disturbance Scale (GSDS). The GSDS is a 21-item scale intended to measure the frequency of subjective sleep disturbances over the past 7 days. Participants rated their sleep disturbances using an 8-point Likert scale with a numeric range of 0 through 7 (0 = never and 7 = every day). Total scores indicate the level of sleep disturbance, with a higher total score indicating a higher level of sleep disturbance. Persons scoring above 42 are classified as poor sleepers. The GSDS has established reliability and validity [70,71].
Pittsburgh Sleep Quality Index (PSQI). The PSQI has 19 self-report items. Five questions assess sleep patterns, duration, and latency, and 14 items are rated from 0 to 3 (0 = not during the past months, 1 = less than once a week, 2 = once or twice a week, and 3 = three or more times a week). The 14 items generate seven subscale scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication, and daytime dysfunction [72]. The subscales yield one global score ranging from 0-21 points, with higher scores indicating worse sleep quality [72]. The PSQI has established reliability and validity and is useful in studying relationships between sleep quality and other variables.
Positive and Negative Affect Scale (PANAS). The PANAS is used to measure affect. Participants rate aspects of affect using a 1-5 scale (1 = slightly or not at all and 5 = extremely). Each schedule, Positive Affect (PA) and Negative Affect (NA), is composed of 10 items. Total scores for the PA and NA schedules are calculated by summing the participant ratings for each schedule. Total scores range from 10 (minimum) to 50 (maximum), representing the emotional extremes of PA and NA. In clinical research the PANAS has been found to be a valid and reliable measurement for assessing positive and negative aspects of mood [73].
Patient Global Impression of Change Scale (PGIC). The PGIC is a reliable and valid measurement for assessing clinically significant change over time for an intervention study and is especially useful in conditions such as chronic pain where meaningful improvement is based upon the patient’s perceived improvement in her/his condition [74-76]. Study participants were asked to identify their most bothersome symptoms over the past week, to describe any changes since beginning the RY intervention by choosing one of seven descriptions of change on a scale of 1 to 7 (1 = no change to 7 = a great deal better, and a considerable improvement that has made all the difference), and to rate the degree of change since beginning the RY classes on an 11-point Likert scale ranging from 0 to 10 (0 = much better to 10 = much worse).
| Weekly questions |
|---|
| •How are you today? |
| •Are you having any problems completing the daily practice log or sleep diary? |
| • Are you having any difficulties with the two weekly classes? |
| •Are you having any difficulties with the home yoga practice? |
| •Have you had any changes in your medications? |
| •Do you have any questions or concerns? |
| 1-month follow-up questions |
| •Are you still practicing restorative yoga? |
| - If yes, how many times per week? |
| - If yes, can you share with me what motivates you to continue your home restorative yoga practice? |
| - If no, can you share with me the reasons you decided not to continue your restorative yoga home practice? |
Table 4: Weekly and 1-month Follow-up Telephone Call Questions.
Participant logs and diaries: Participants completed daily sleep diaries and practice logs during the 8-week intervention. The research assistants collected completed logs and diaries each week and distributed log forms for the next week at the first RY class each week.
Daily sleep diary. A daily sleep diary was used to collect data on sleep duration, sleep interruptions, and sleep initiation. Sleep diaries are widely used and can be found in a variety of forms. Bedtime, sleep latency, number of sleep interruptions, time of arising, and how rested the study participant felt upon awaking were recorded in a daily sleep diary.
Daily practice log. All participants completed daily practice logs recording their feelings before and after completion of each RY practice, time spent in the RY practice, and whether it was a home practice or RY class.
Telephone calls and log: Each week during the 8-week RY intervention, the study coordinator contacted each participant for the purposes of monitoring (a) overall study and treatment fidelity, (b) any changes in medications, (c) occurrence of any AEs, (d) home practice and encouraging class attendance, and (e) participant questions or concerns. The six questions asked during the telephone call are shown in Table 4.
1-month follow-up. One month after completing the 8-week RY intervention, the investigator contacted each study participant by telephone and asked four questions (Table 4) designed to assess continued adherence to the RY 20-minute home RY practice and feasibility of a 90-minute home RY practice in lieu of a 90-minute group class.
Data analysis
Quantitative analysis: Study sample characteristics at baseline were analyzed using SPSS version 22. Means and standard deviations are reported for age, age diagnosed with FM, and years since diagnosis with FM. Frequencies are reported for sex, race, ethnicity, years of education, partner status, living situation, and comorbidities.
Feasibility data were entered into an Excel spreadsheet for simple ratio calculations of screening, recruitment, retention, and intervention adherence and 1-month post-intervention intention/continuation rates. Reasons for declining to participate in an 8-week RY intervention were tabulated using frequency calculations.
Given the small sample size, Wilcoxon non-parametric tests were run on the secondary outcome measures. Individual scores and overall group means were calculated at 3 time points (baseline to week 4, baseline to week 8, and week 4 to week 8) to identify statistically meaningful trends in levels of perceived pain, stress, sleep disturbances, and HQoL. Statistically significant trends over the 3 time points were based on a two-tailed test with a p-value of p ≤ 0.05. Outcome measures for perceived levels of pain, sleep disturbance, and disease impact on HQoL were assessed for clinically meaningful trends. Clinically meaningful trends in the FIQR were identified as a percent change raw scores from pre- to post-intervention of ≥ 14% [57]. Changes in scores of pain measures of 10-29% were considered minimally important, 30- 49% moderately important, and ≥ 50% a substantial improvement [77]. A change in the SF36 of ≥ 12% from baseline scores [78] and a change in sleep measures (PSQI and GSDS) ≥ 6% [79] were considered minimal clinically important differences. Clinically significant improvement using the PGIC was defined as selection of the categories of “better” or “a great deal better,” and minimal improvement was defined as “moderately better” [75,76].
Qualitative explication: To corroborate and elaborate upon the quantitative feasibility findings, study participants’ descriptions of expectations, perceptions, and the lived experience of the 8-week RY intervention were assessed using a hermeneutic phenomenological methodology. As a heuristic framework guiding the development of the semi-structured interview questions, the antecedents of intention posited by the TPB informed the theoretical coding, analysis, and interpretation of the qualitative data. Study participant pre- and postinterviews were transcribed and checked for accuracy against the original recordings. NVivo software version 10 was used to sort and organize these data. Textual analysis of transcripts from the semistructured interviews was conducted using a primary (open) and a secondary (theoretical-TPB) coding strategy. Interview transcripts were coded until saturation using steps outlined by Giorgi [80], and a reflective diary [81] to support neutrality of researcher analysis was maintained throughout the coding process. This process involved several steps, including the identification of meaning units, and concluded with the identification of themes.
Results interpretation: Using a concurrent triangulation strategy, the quantitative and qualitative study findings were compared for cross-corroboration and interpretation [52]. The mixed-methods approach provided a contextual and expanded understanding of the feasibility findings and provided an explanation of actual behavior, perceived facilitators and barriers to practice, and beliefs related to a RY intervention used as a symptom self-management strategy for those diagnosed with FM.
The study protocol was designed to assess the feasibility of a RY intervention for persons diagnosed with FM and to collect preliminary data on its perceived effects on FM-related symptoms. While the rationale for selecting RY as a feasible and safe yoga style is compelling, the six yoga studies previously conducted in the FM population (none of which investigated RY) support the need for an assessment of the feasibility of a RY intervention in this population. Given limited present day resources, it is practical to first engage in feasibility studies [82]. The heterogeneity of yoga styles and philosophical differences in yoga lineages, as well as the numerous yoga components (e.g., asana, pranayama, yoga nidra, pratyahara, mindfulness, mantra, mudra) and combinations of these, produce an almost endless array of possible interventions. Therefore, feasibility studies that use sound methodologies and guidelines are needed to evaluate potential yoga interventions in specific clinical populations. Findings from these less resource-intensive studies allow investigators to direct their limited resources towards investigating those yoga styles that show the greatest potential for efficacy and effectiveness in a given population [82].
Yoga experts caution against the use of strict methodological and intervention structure, citing that the interventions may become too prescriptive [49,50]. Prior to a large, resource-intensive study, feasibility studies offer the opportunity for researchers to test guidelines and methodologies and to refine acceptable modifications that support individualization of the intervention. Because persons diagnosed with FM have a high incidence of comorbidities [83] and a heterogeneous symptom experience, as well as the fact that the underlying etiology and pathophysiology of FM remains unclear, the selection of a yoga style that can be modified easily for individual needs and limitations is especially important.
Yoga and yoga therapy research guidelines are emerging, but more work is needed to improve the rigor of yoga therapy study designs and the reporting of the findings. The protocol for the current study was developed using the TPB theoretical framework [51,84], the CONSORT statement extension for non-pharmacologic intervention treatments [85], guidelines for yoga research proposed by Sherman [49], and the Delphi survey recommendations for musculoskeletal conditions proposed by Ward and colleagues [50]. Use of frameworks and guidelines such as those reported here form the basis for replicable research and validation of intervention outcomes leading to evidencebased best practices for the clinical application of yoga therapy.
The study protocol described here is a single-arm feasibility study with a small sample recruited using a convenience sampling methodology, which limits generalizability of findings. Potential for selfselection exists for yoga interventions; however, the limitations resulting from this design are appropriate for the study aims assessing feasibility. The design is consistent with acceptable research practices. Based on the preliminary nature of the study and its purpose to determine feasibility by answering the questions: “Can persons with FM participate in an 8-week RY intervention?” and “Will persons with FM participate in an 8-week RY intervention?” assessing individual behavioral beliefs, behavioral control (actual and perceived), and social norms provides an expanded contextual understanding of feasibility [82].
This study protocol was designed to align with currently available guidelines for yoga and yoga therapy research and those specific to individuals diagnosed with FM. The selection of a theoretical framework provided structure, guidance for outcome measure selection, and interpretation of the study findings. The intervention design allows for individual modification of the RY intervention postures while maintaining the essential functional elements of the RY sequence and practice. The outcomes of this feasibility study will be used to inform the design of a future larger, randomized, controlled trial to investigate the efficacy of a RY or other yoga style intervention for self-management of FM-related symptoms.
This study was made possible through a grant from the University of Virginia Contemplative Sciences Center and by funding from the University of Virginia Center for the Study of Complementary and Alternative Therapies
The authors are grateful for the assistance of Katharine Adelstein, MSN, ANPBC, RN, and Olivia Pagano and Jessica Denomme (two undergraduate nursing students), who provided valuable help in the conduct of the RY study. Also, the authors acknowledge the contribution of Dana Mowdy-Spencer, who created the illustrations of the RY postures shown in Table 2. The authors thank the University of Virginia School of Nursing for use of its facilities and the University of Virginia Contemplative Sciences Center and Center for the Study of Complementary and Alternative Therapies for funding this study.