Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 1
Objective: Detecting prognostic factors of pars plana vitrectomy in treatment of lamellar macular holes using Spectral Domain Optical Coherence Tomography (SD-OCT).
Methods: Prospective intervention study recruiting 20 eyes of 20 patients with lamellar macular hole. Patients underwent 23 G Pars plana vitrectomy with Epi-Retinal Membrane (ERM) and Internal Limiting Membrane (ILM) peeling with inverted flap on the surface with sulphur hexafluoride gas tamponade. Patients were evaluated pre-operatively and at one, three and six months post-operatively for Best Corrected Visual Acuity (BCVA, logMAR), OCT evaluation of ellipsoid zone, Central Macular Thickness (CMT) and foveal configuration.
Results: Visual acuity improved in 14 eyes at a mean of 6 months after vitrectomy. Subgroup analysis showed that statistically significant visual benefit was only observed in patients with an intact photoreceptor Inner Segment/Outer Segment (IS/ OS) junction (p=0.022), with foveal thickness bigger than 100 μm (p<0.0001), presence of preoperative epiretinal membrane (p=0.01), absence of Lamellar Hole associated Epiretinal Proliferation (LHEP) (p=0.01) and pre-operative BCVA is significantly correlated to post-operative BCVA (r=0.506, p=0.023). The most efficient model to predict final VA was the combination of preoperative Visual Acuity (VA) and the presence or absence of IS/OS disruption.
Conclusion: Presence of Epiretinal Membrane (ERM), absence of Lamellar Hole associated Epiretinal Proliferation (LHEP), intact photoreceptor IS/OS junction, minimum foveal thickness more than 100 μm and good initial BCVA are all favorable prognostic factors.
Lamellar Macular Hole; Epiretinal membrane; Epiretinal proliferation; SD-OCT
Lamellar Macular Holes (LMH) is a clinical entity first described by Gass in 1975 as a result of rupture of cystoid macular edema [1]. It is considered as a partial thickness defect of the macula caused by separation between outer and inner retinal layers [2]. Lamellar hole was described as an abortive process in the formation of a full-thickness macular hole [3,4]. Optical Coherence Tomography (OCT) evaluation has improved the diagnosis of lamellar holes, because it allows visualization of non– full-thickness defects of the macula [5].
Recent studies classified LMH according to type of Epi-Retinal Membrane (ERM) associated with it, into Conventional ERM (C ERM) and Atypical ERM (A ERM). These two types of ERM differ in their cell and collagen composition. LMHs with A ERM are compromised functionally and morphologically than those with C ERM [6].
It is noticed that most patients with LMH experience mild to moderate visual loss and/or metamorphopsia, and the lesion remains stable on OCT over the years, so many physicians follow up these patients in the long term without surgery [7]. Vitrectomy is considered if there is decrease in visual acuity or progressive thinning of the fovea during follow up period [8].
The classification of lamellar defects subtypes has been recently proposed into two subtypes; tractional vs. degenerative. The tractional form is characterized by macular schisis-like appearance, tractional epiretinal membrane, and intact ellipsoid layer. Degenerative type often presents intraretinal cavitation, non- tractional epiretinal proliferation, and ellipsoidal line disruption [9]. Tractional lamellar holes have better surgical outcome as they associated with lesser alteration to outer retina [10,11].
Poor preoperative visual acuity, disrupted IS /OS junction or lower central foveal thickness on preoperative Spectral Domain Optical Coherence Tomography (SD-OCT) predict poor visual outcome after LMH Surgery [12]. LMH with Epiretinal Proliferation (LHEP) associated with A ERM has worse surgical prognosis than LMH associated with C ERM [13,14].
In this prospective interventional study, we investigate the prognostic factors of pars-plana vitrectomy in treatment of lamellar macular holes using Spectral Domain Optical Coherence Tomography (SD-OCT).
A prospective interventional study including 20 eyes of 20 patients with lamellar macular holes (tractional or degenerative). Patients were recruited between July 2019 to January 2021 at Fayoum University Hospital and Research Institute of Ophthalmology. Written informed consent was obtained from all patients. The study was carried out with approval of the Ethics research committee of Fayoum University hospitals and in adherence to the tenets of the Declaration of Helsiniki.
We excluded patients with previous pars-plana vitrectomy, diabetic retinopathy, full thickness macular hole, retinal detachment, age related macular degeneration, choroidal neovascularization or with advanced glaucoma.
Collected data included demographic information, general medical and ophthalmological history. All patients underwent full ophthalmological examination including slit lamp biomicroscopy, dilated fundus examination and BCVA was recorded in logMAR.
We used SD-OCT (Optovue, Inc., Fremont, CA, USA) as a preoperative evaluation of lamellar macular hole for differentiation between tractional and degenerative type. Detecting the presence of Epi-Retinal membrane (ERM), Epi-Retinal Proliferation (LHEP) and ellipsoidal zone disruption (intact photoreceptor IS/OS junction was evaluated as continuous hyper reflective line, whereas loss or irregularity of this line indicate disruption at IS/OS junction). Minimum foveal thickness was measured manually from the vitreoretinal surface to the sensory retina / retinal pigment epithelium interphase using a caliper on SD- OCT. Lamellar macular hole diameter (inner diameter&outer diameter) was recorded.
All patients in this study underwent 23 G Pars plana vitrectomy with ERM peeling and ILM peeling with inverted flap on the surface not inside the hole using brilliant blue dye under local anesthesia with isoexpansile sulphur hexafluoride gas tamponade. Patients with significant cataract underwent phacovitrectomy.
Patients were instructed to maintain a prone position for up to 7 days after surgery. All patients were ophthalmologically evaluated one month, three months and six months post operatively for BCVA (logMAR), OCT evaluation of ellipsoid zone, CMT, foveal configuration.
Our study included 20 patients 9 males and 11 females. The mean age was 58.5 ± 11.8 years. The mean pre-operative BCVA was logMAR 1.28 ± 0.36. BCVA significantly increased to logMAR 0.94 ± 0.49 at 6 months after surgery, as illustrated in Figure 1. Post-operatively the BCVA improved in 14 eyes early and late postoperative. Two eyes BCVA worsened early post-operative due to development of Full Thickness Macular Hole (FTMH) then improved late post-operative after closure of FTMH (one of them closed spontaneously and the other closed by fresh frozen amniotic membrane and isoexpansile sulfur hexafluoride (SF6) tamponade) as shown in Figure 2.
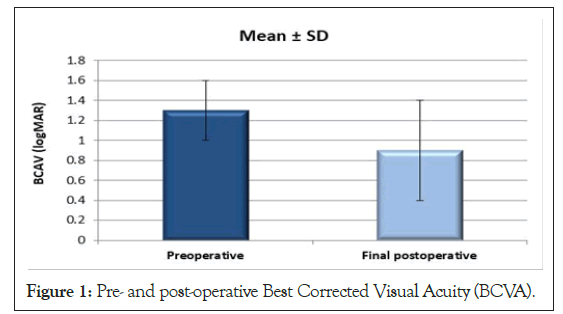
Figure 1: Pre- and post-operative Best Corrected Visual Acuity (BCVA).
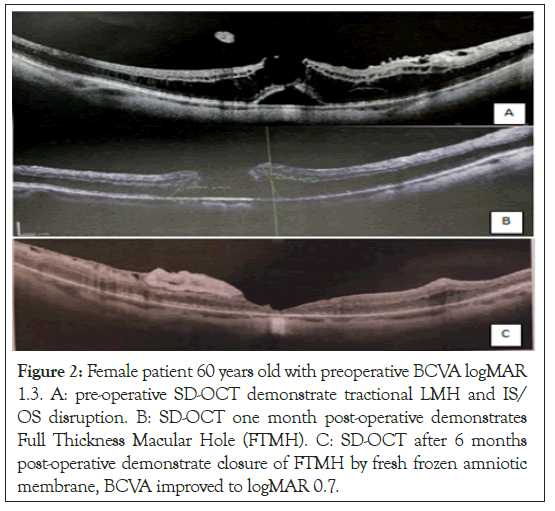
Figure 2: Female patient 60 years old with preoperative BCVA logMAR 1.3. A: pre-operative SD-OCT demonstrate tractional LMH and IS/ OS disruption. B: SD-OCT one month post-operative demonstrates Full Thickness Macular Hole (FTMH). C: SD-OCT after 6 months post-operative demonstrate closure of FTMH by fresh frozen amniotic membrane, BCVA improved to logMAR 0.7.
One eye BCVA did not improve postoperatively. Three eyes BCVA worsened post operatively due to development of cataract or papillo-macular bundle injury during ERM removal, as illustrated in Figure 3.
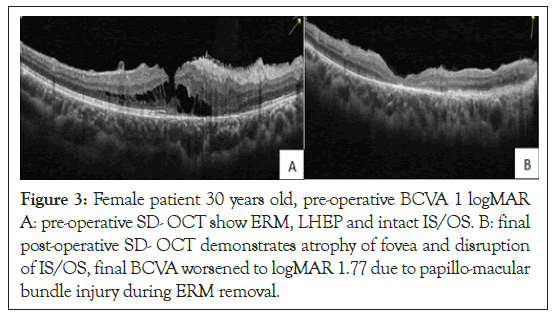
Figure 3: Female patient 30 years old, pre-operative BCVA 1 logMAR A: pre-operative SD- OCT show ERM, LHEP and intact IS/OS. B: final post-operative SD- OCT demonstrates atrophy of fovea and disruption of IS/OS, final BCVA worsened to logMAR 1.77 due to papillo-macular bundle injury during ERM removal.
Pre-operative mean central foveal thickness was 136.6 ± 49.6 μm which significantly increased to 191.9 ± 61.6 μm post-operatively as shown in Figure 4.

Figure 4: Pre-operative and final post-operative central foveal thickness (μm).
When initial foveal thickness was >100 μm, the VA significantly increased from 1.29 ± 0.38 logMAR to 0.83 ± 0.44 logMAR, while it did not for the group with foveal thickness of 100 μm or less, as demonstrated in following Table 1 and Figures 5-7. So, Pre-operative foveal thickness is significantly correlated to final post-operative BCVA as shown in Figure 8.
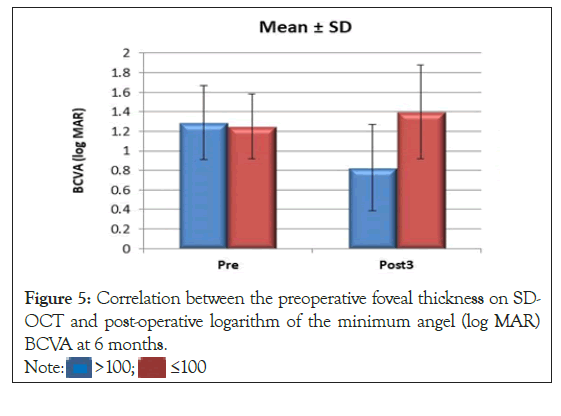
Figure 5: Correlation between the preoperative foveal thickness on SD-
OCT and post-operative logarithm of the minimum angel (log MAR) BCVA at 6 months. 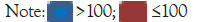
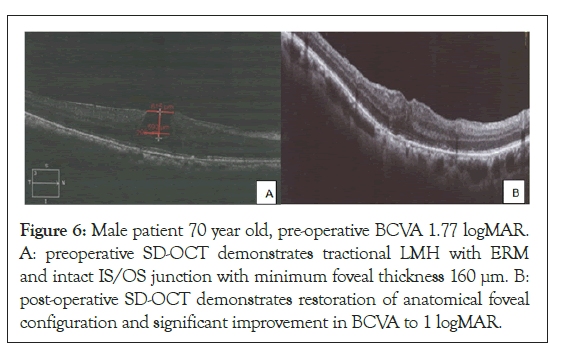
Figure 6: Male patient 70 year old, pre-operative BCVA 1.77 logMAR. A: preoperative SD-OCT demonstrates tractional LMH with ERM and intact IS/OS junction with minimum foveal thickness 160 μm. B: post-operative SD-OCT demonstrates restoration of anatomical foveal configuration and significant improvement in BCVA to 1 logMAR.
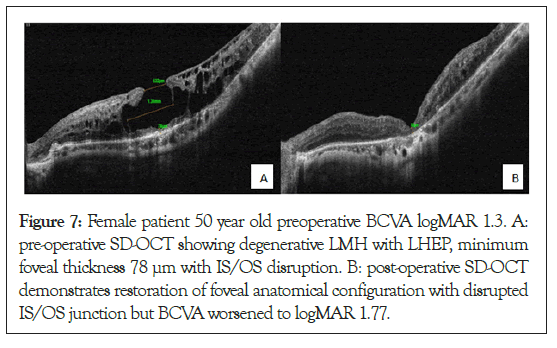
Figure 7: Female patient 50 year old preoperative BCVA logMAR 1.3. A: pre-operative SD-OCT showing degenerative LMH with LHEP, minimum foveal thickness 78 μm with IS/OS disruption. B: post-operative SD-OCT demonstrates restoration of foveal anatomical configuration with disrupted IS/OS junction but BCVA worsened to logMAR 1.77.
Figure 8: Correlation between the pre-operative foveal thickness on SD- OCT and post-operative (log MAR) BCVA at 6 months.
In tractional LMH which associated with Epiretinal Membranes (ERM), VA significantly improved from 1.12 ± 0.35 logMAR to 0.73 ± 0.40 post-operatively, while it did not improve in degenerative LMH not associated with ERM as shown in Table 1 and Figures 9-11. In eyes without LHEP, VA significantly improved from 1.12 ± 0.35 logMAR to 0.73 ± 0.40 logMAR, however eyes with LHEP not significantly improved post operatively as shown in Tables 2,3 and Figures 12-14.
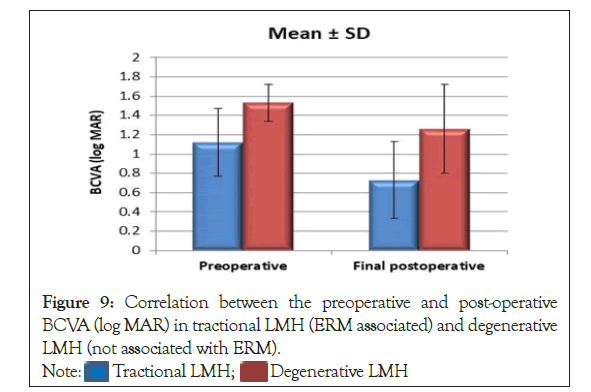
Figure 9: Correlation between the preoperative and post-operative BCVA (log MAR) in tractional LMH (ERM associated) and degenerative LMH (not associated with ERM). 
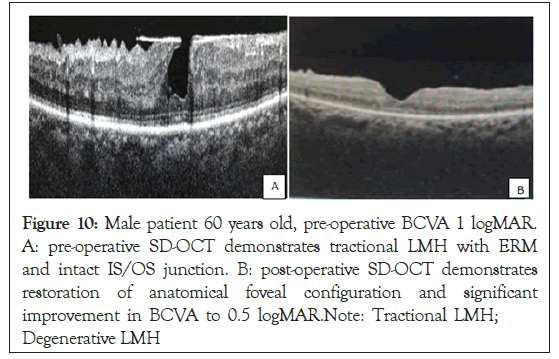
Figure 10: Male patient 60 years old, pre-operative BCVA 1 logMAR. A: pre-operative SD-OCT demonstrates tractional LMH with ERM and intact IS/OS junction. B: post-operative SD-OCT demonstrates restoration of anatomical foveal configuration and significant improvement in BCVA to 0.5 logMAR.Note: Tractional LMH; Degenerative LMH
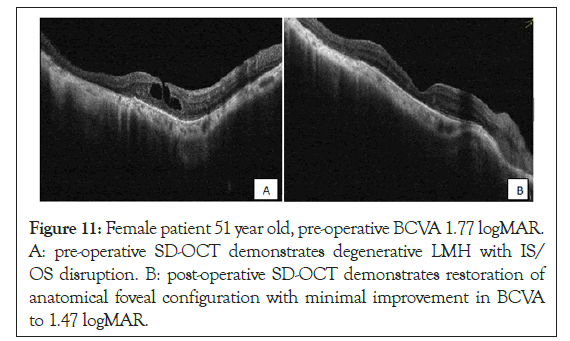
Figure 11: Female patient 51 year old, pre-operative BCVA 1.77 logMAR. A: pre-operative SD-OCT demonstrates degenerative LMH with IS/ OS disruption. B: post-operative SD-OCT demonstrates restoration of anatomical foveal configuration with minimal improvement in BCVA to 1.47 logMAR.
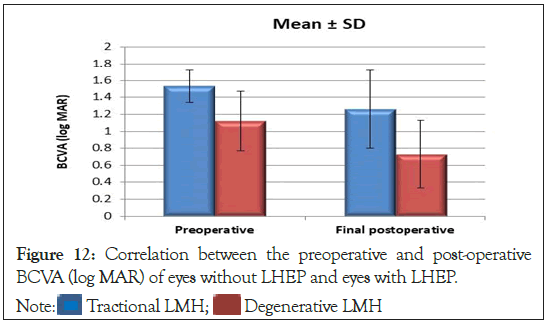
Figure 12: Correlation between the preoperative and post-operative BCVA (log MAR) of eyes without LHEP and eyes with LHEP. 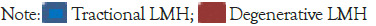
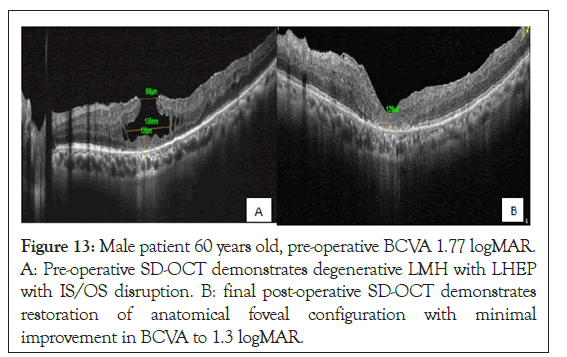
Figure 13: Male patient 60 years old, pre-operative BCVA 1.77 logMAR. A: Pre-operative SD-OCT demonstrates degenerative LMH with LHEP with IS/OS disruption. B: final post-operative SD-OCT demonstrates restoration of anatomical foveal configuration with minimal improvement in BCVA to 1.3 logMAR.
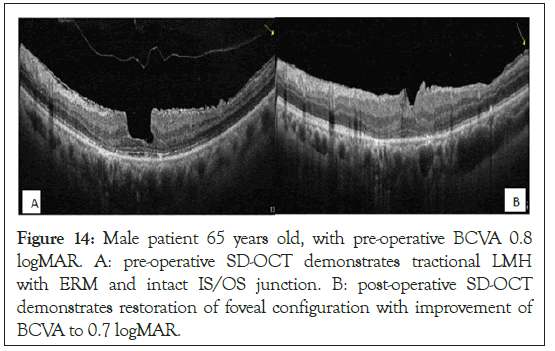
Figure 14: Male patient 65 years old, with pre-operative BCVA 0.8 logMAR. A: pre-operative SD-OCT demonstrates tractional LMH with ERM and intact IS/OS junction. B: post-operative SD-OCT demonstrates restoration of foveal configuration with improvement of BCVA to 0.7 logMAR.
| Tractional LMH (ERM present) N=12 | Degenerative LMH (ERM absent) N=8 | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| BCVA (log MAR) | ||||
| Preoperative | 1.12 | 0.35 | 1.53 | 0.19 |
| Final postoperative | 0.73 | 0.4 | 1.26 | 0.46 |
| P-value | 0.010 (S) | 0.146 (NS) | ||
Abbreviation: ERM: Epi-Retinal Membrane; SD: Standard Deviation; BCVA: Best Corrected Visual Acuity; LMH: Lamellar Macular Holes
Table 1: Correlation between the preoperative and post-operative BCVA (log MAR) in tractional LMH (ERM associated) and degenerative LMH (not associated with ERM).
| LHEP N=8 | No LHEP N=12 | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| BCVA (log MAR) | ||||
| Preoperative | 1.53 | 0.19 | 1.12 | 0.35 |
| Final postoperative | 1.26 | 0.46 | 0.73 | 0.4 |
| P-value | 0.146 (NS) | 0.010 (S) | ||
Abbreviation: LHEP: Lamellar Hole associated Epiretinal Proliferation; SD: Standard Deviation; BCVA: Best Corrected Visual Acuity
Table 2: Correlation between the preoperative and post-operative BCVA (log MAR) of eyes without LHEP and eyes with LHEP.
Visual acuity significantly increased from 1.10 ± 0.73 logMAR to 0.73 ± 0.42 logMAR after surgery for the group without IS/OS disruption pre-operatively, while it did not significantly changed after surgery for the group with pre-operative IS/OS disruption as shown in Figures 15-18.
Figure 15: Correlation between the pre-operative and post-operative BCVA (log MAR) in Photoreceptor’s inner and outer segments junction (IS/OS). 
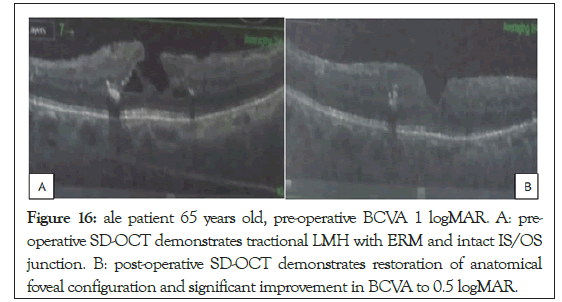
Figure 16: ale patient 65 years old, pre-operative BCVA 1 logMAR. A: pre- operative SD-OCT demonstrates tractional LMH with ERM and intact IS/OS junction. B: post-operative SD-OCT demonstrates restoration of anatomical foveal configuration and significant improvement in BCVA to 0.5 logMAR. improvement in BCVA to 0.5 logMAR.Note: Tractional LMH;
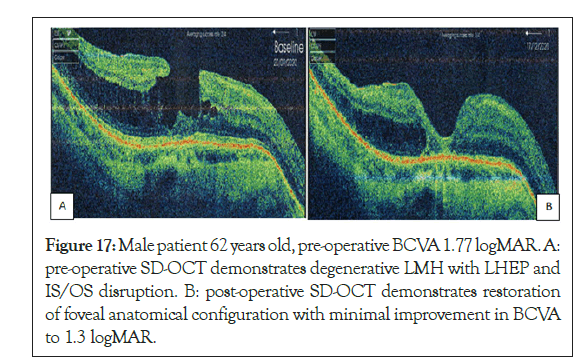
Figure 17: Male patient 62 years old, pre-operative BCVA 1.77 logMAR. A: pre-operative SD-OCT demonstrates degenerative LMH with LHEP and IS/OS disruption. B: post-operative SD-OCT demonstrates restoration of foveal anatomical configuration with minimal improvement in BCVA to 1.3 logMAR.
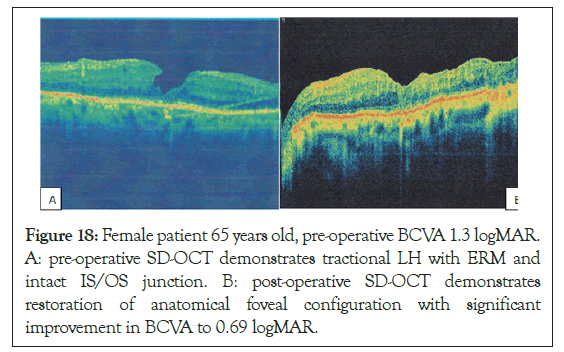
Figure 18: Female patient 65 years old, pre-operative BCVA 1.3 logMAR. A: pre-operative SD-OCT demonstrates tractional LH with ERM and intact IS/OS junction. B: post-operative SD-OCT demonstrates restoration of anatomical foveal configuration with significant improvement in BCVA to 0.69 logMAR.
| Intact IS/OS N=11 | Disrupted IS/OS N=9 | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| BCVA (log MAR) | ||||
| Preoperative | 1.1 | 0.37 | 1.51 | 0.2 |
| Final postoperative | 0.73 | 0.42 | 1.2 | 0.47 |
| P-value | 0.022 (S) | 0.075 (NS) | ||
Abbreviation: BCVA: Best Corrected Visual Acuity; IS: Inner Segment; OS: Outer Segment; SD: Standard Deviation
Table 3: Correlation between the preoperative and post-operative BCVA (log MAR) in Photoreceptor's inner and outer segments junction (IS/OS).
In our study we evaluated prognostic factors that determine anatomical and functional outcome after pars plana vitrectomy in treatment of patients with LMHs. We used SD-OCT for pre- operative evaluation of the patient and further classification into tractional LMH or degenerative LMH depending on presence or absence of Epi-Retinal Membrane (ERM) and presence or absence of lamellar hole associated epiretinal proliferation. Also, we determined the status of photoreceptors IS/OS junctions and minimum foveal thickness. Evaluation of pre-operative logMAR BCVA was important for correlation with post-operative results. Regarding to the condition of preoperative IS/OS junction we conducted that visual acuity significantly increased after surgery for the group without IS/OS disruption pre-operative, while it did not significantly change after surgery for the group with pre- operative IS/OS disruption. Similarly, Michalewska et al. studied the correlation between pre-operative IS/OS status and final post-operative outcome and find that patients with pre-operative IS/OS disruption have lower post-operative visual acuity and have final postoperative VA less than 0.2 Snellen [15]. Also, Lee et al. investigated pre-operative VA and SD-OCT features as predictors of surgical outcome and showed that statistically significant visual benefit was only observed in patients with an intact photoreceptor Inner Segment/Outer Segment (IS/OS) junction [12]. Similarly, Sun et al. examined the surgical results of Lamellar Macular Hole (LMH) secondary to Epi-Retinal Membrane (ERM) in a retrospective study and found that final post-operative BCVA is related to an intact photoreceptor IS-OS junction rather than to the normalization of the macular contour, so there is a strong association between final visual outcome and preoperative intact IS/OS [16]. According to LMH classification into tractional or degenerative, our study demonstrated that in tractional LMH which associated with Epi-Retinal Membranes (ERM) VA significantly improved post-operatively while it did not in degenerative LMH which not associated with ERM so pre- operative classification of LMH into tractional or degenerative depending on SD-OCT characteristics is important for determining post-operative outcome. Similarly, Figueroa et al. compared functional and anatomical outcomes of vitrectomy with membrane peeling in tractional Lamellar Macular Holes (LMH)/Macular Pseudo Holes (MPH) versus degenerative LMH in a multicenter retrospective study and found that pre-operative best-corrected visual acuity was better in tractional LMH/MPH than degenerative LMH, premacular membranes were found in all tractional LMH/MPH, whereas LMH-associated Epiretinal Proliferation (LHEP) was present in all degenerative LMH. Best-corrected visual acuity improved in both tractional LMH/ MPH and degenerative LMH but was better in tractional LMH/ MPH [13]. Similar to our results, Coassin et al. reported long- term results of vitrectomy for Lamellar Macular Holes (LMH) to evaluate the correlation between type of lamellar hole tractional vs. degenerative and visual outcome and found that visual acuity significantly increased in the tractional but not in the degenerative forms of LMH [17]. According to the condition of Lamellar Hole associated Epiretinal Proliferation (LHEP), our results demonstrated that LMH with LHEP had higher rate of disrupted IS/OS junction pre-operatively rather than LMH without LHEP, we found also that in eyes without LHEP VA significantly improved post-operatively, however eyes with LHEP not significantly improved post-operatively. Like our results, Lai et al. reported the clinical findings and surgical outcomes of Lamellar Macular Holes (LMH) with or without Lamellar Hole-associated Epiretinal Proliferation (LHEP), and found that in the LMH with LHEP had significantly thinner bases and larger openings than those without. The rate of disrupted IS/ OS line was higher in the LHEP subgroup pre-operatively, but similar between subgroups post-operatively [18]. Contrary to our results, Lai et al. conducted that the pre-operative and post- operative visual acuity showed no significant difference between two subgroups so LHEP was associated with a more severe defect but didn’t affect surgical outcomes [18]. Ko et al. agreed with our results and reported the clinical findings and surgical outcomes of Lamellar Macular Holes (LMHs) with and without Lamellar Hole-associated Epiretinal Proliferation (LHEP) and found that pre-operatively, eyes with LHEP were characterized by a greater hole diameter, thinner fovea and greater incidence of outer retinal disruption. Best-Corrected Visual Acuity (BCVA) significantly improved after surgery in eyes without LHEP but showed no change in eyes with LHEP. Initial BCVA was not different between the two groups; however, final BCVA was better in eyes without LHEP so there was no visual benefit after surgery in LMH patients with LHEP [14]. Contrary to our results, Dell’Omo et al. compared the morphologic and functional characteristics and response to surgery of Lamellar Macular Holes (LMHs) with and without Lamellar Hole-associated Epiretinal Proliferation (LHEP) and standard Epiretinal Membrane (ERM) in a retrospective study and found that the presence of LHEP does not seem to influence the natural course of the disease and the response to surgery and VA did not differ in cases with and without LHEP post-operatively [19]. Regarding to preoperative BCVA as an indicator for postoperative functional outcome, we demonstrated a correlation between preoperative visual acuity and final post- operative visual acuity and found that pre-operative BCVA significantly correlated to final post-operative BCVA as when initial VA is poor there is no significant improvement in final post-operative VA. Similar to our results, Lee et al. investigated pre-operative VA and SD-OCT features as predictors of surgical outcome and found that statistically significant visual benefit was only observed in patients when initial VA better than 20/100, so poor initial VA predicted poor vision outcome after LMH surgery [12]. Regarding to preoperative central foveal thickness, we demonstrated a correlation between the pre-operative foveal thickness on spectral domain optical coherence tomography and post-operative logarithm of the minimum angel (logMAR) BCVA at 6 months and found that when initial foveal thickness was >100 μm VA significantly increased, while it did not for the group with foveal thickness of 100 μm or less. Similarly, Lee et al. investigated pre-operative VA and SD-OCT features as predictors of surgical outcome. Results showed that statistically significant visual benefit was only observed in patients with foveal thickness bigger than 100 μm, so a thin fovea on pre-operative SD-OCT predicted poor vision outcome after LMH surgery [12]. Similar to our results, Coassin et al. reported the causes of VA loss after surgery were persistent foveal splitting, cystoid macular edema, papillo-macular bundle defect, retinal detachment, FTMH and post-operative cataract development [17].
In our study we concluded causes of visual loss after surgery as we reported two patients (10%) developed postoperative FTMH, two patients (10%) developed post-operative cataract and one patient (5%) developed papillo-macular bundle injury. Presence of Epiretinal Membrane (ERM), absence of Lamellar Hole associated Epiretinal Proliferation (LHEP), intact photoreceptor IS/OS junction, minimum foveal thickness more than 100 μm and good initial BCVA are all prognostic factors that favors the postoperative results of pars-plana vitrectomy in the treatment of Lamellar macular hole.
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: El-Sayed SSE, Kamal MA, Azab AAA, Saif ATS, Mohamed KKA (2021) Prognostic Factors of Pars Plana Vitrectomy in Treatment of Lamellar Macular Holes. J Clin Exp Ophthalmol. 13:904
Received: 09-Dec-2021, Manuscript No. JCEO-21-14873; Editor assigned: 13-Dec-2021, Pre QC No. JCEO-21-14873 (PQ); Reviewed: 27-Dec-2021, QC No. JCEO-21-14873; Revised: 13-Jan-2022, Manuscript No. JCEO-21-14873 (R); Published: 10-Jan-2022 , DOI: 10.35248/2155-9570.22.13.904
Copyright: © 2021 El-Sayed SSE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.