Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2022)Volume 13, Issue 6
Introduction: Behcet’s disease is a systemic inflammatory disease. Ocular manifestations are an important diagnostic criterion. It is frequent and serious and may affect the visual prognosis. Its particularity is the richness of the initial ophthalmologic presentation and the good clinical evolution under treatment.
We present the case of a patient with a posterior scleritis revealing Behcet’s disease.
Aim: Underline a rare mode of revelation of Behcet’s disease, which is posterior scleritis.
Observation: It is about a young patient of 24 years old who presented for a painful exophthalmos of the left eye with a decrease visual acuity whose questioning revealed a recurrent oral aphthosis with pseudo folliculitis.
Results: Ophthalmologic examination of the left eye revealed retinal folds at the posterior pole with papillary oedema.
B-scan ultrasonography showed thickening of the scleral tissue, revealing a T-sign suggestive of posterior scleritis, which was also clearly visible on orbit scanner and orbit Magnetic Resonance Imaging (MRI). The clinical, radiological and biological arguments made it possible to make the diagnosis of Behcet’s disease. High dose corticosteroid therapy was introduced and the outcome was spectacular.
Discussion: Ocular involvement in Behcet’s disease is an important diagnostic criterion. Only two cases of posterior scleritis that is reported in the literature and no case so far has revealed the disease.
Conclusion: Although posterior scleritis is a rare condition in Behcet’s disease, it must be thought about.
Posterior scleritis; Behcet’s disease; B-scan ultrasonography; Visual acuity; Oral aphthosis
Behcet’s disease is a chronic systemic inflammatory disease of unknown etiology. Ocular involvement is common, varying between 30% and 80% [1]. Several ocular manifestations are described, scleritis is one of them.
Posterior scleritis is the rarest form of scleritis and often misdiagnosed. It corresponds to a scleral inflammation located behind the ora serrata. Their diagnosis is particularly difficult, both when it is isolated because the eye is not red, and when it is associated with anterior scleritis which could make you forget to look for it [2].
In the literature, it is rarely reported in Behcet’s disease [1,3]. We report the case of Behcet’s disease revealed following a posterior scleritis.
It is about a 24-year-old patient with no significant history who presented to the emergency room with inflammatory left eye and reduced visual acuity.
On questioning, the patient complains of recurrent oral aphthosis with pseudo folliculitis in the back. On examination, the right eye is normal. On the left, visual acuity is assessed at 7/10 Parinaud 3, unilateral and axil exophthalmos and limited abduction and elevation (Figure 1).
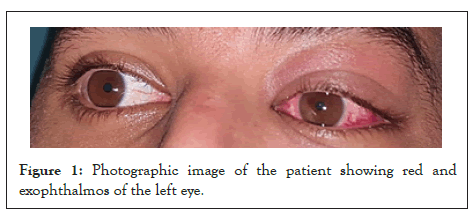
Figure 1: Photographic image of the patient showing red and exophthalmos of the left eye.
Biomicroscopic examination revealed conjunctival hyperemia in the anterior segment without tyndall of the anterior chamber. The photomotor reflex and pression intraocular were normal. On fundus examination, retinal folds were noted predominantly at the posterior pole and temporally of the papilla with papillary edema.
Macular OCT revealed the presence of retinal folds in the inner layers of the neuroretin (Figure 2).
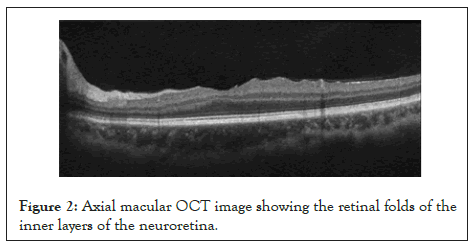
Figure 2: Axial macular OCT image showing the retinal folds of the inner layers of the neuroretina.
Fluorescein retinal angiography found retinal folds and papillary diffusion (Figures 3 and 4).
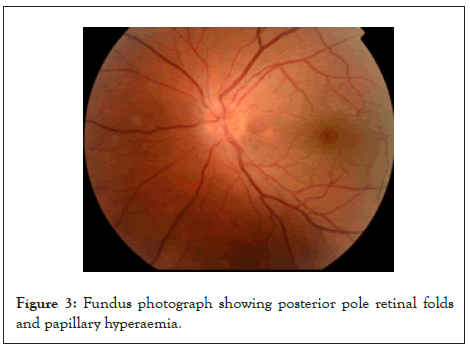
Figure 3: Fundus photograph showing posterior pole retinal folds and papillary hyperaemia.
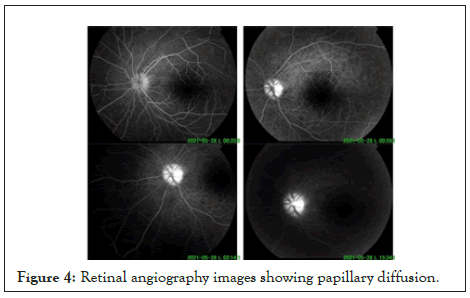
Figure 4: Retinal angiography images showing papillary diffusion.
B-scan ultrasonography showed thickening of the scleral tissue, revealing a T-sign suggestive of posterior scleritis (Figure 5).
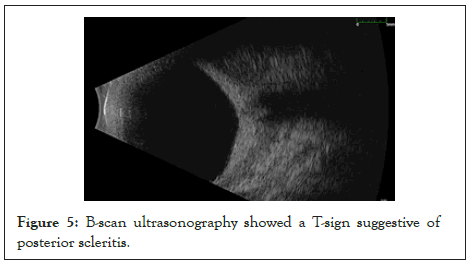
Figure 5: B-scan ultrasonography showed a T-sign suggestive of posterior scleritis.
A radiological complement was made in particular an oculo- orbital scanner which revealed a grade 1 exophthalmos with irregular thickening of the posterior sclera around the optic nerve and the oculo-orbital Magnetic Resonance Imaging (MRI) revealed an infiltration of the intra-conical orbital fat (Figures 6 and 7).
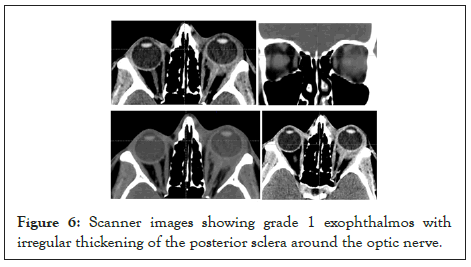
Figure 6: Scanner images showing grade 1 exophthalmos with irregular thickening of the posterior sclera around the optic nerve.
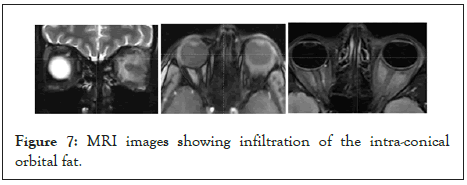
Figure 7: MRI images showing infiltration of the intra-conical orbital fat.
The diagnosis of Behcet’s disease is retained. A biological assessment was requested. Markers of inflammation were elevated (CRP at 30 mg/l and ESR at 60 mm/h). The immunological markers (rheumatoid factor, anti-citrullinated peptide antibodies, antinuclear antibodies and anti-neutrophil cytoplasm antibodies) were negative. Serological tests for herpes simplex, herpes zoster, syphilis, Lyme disease, HIV and toxoplasmosis as well as tuberculosis came back negative. A bolus of methylprednisolone was instituted at a rate of 10 mg/kg/day for 3 days, followed by oral prednisone at a dose of 1 mg/kg/day. The evolution was spectacular with improvement in pain, improvement in visual acuity to 10/10, reduction in the thickness of the scleral tissue on ocular ultrasound and marked regression of the macular folds on examination of the fundus and macular Optical Coherence Tomography (OCT) (Figures 8 and 9).
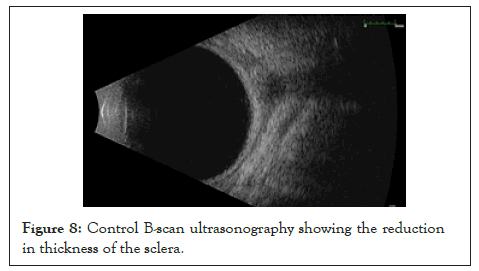
Figure 8: Control B-scan ultrasonography showing the reduction in thickness of the sclera.
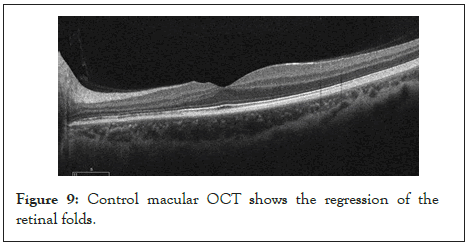
Figure 9: Control macular OCT shows the regression of the retinal folds.
The patient is therefore referred to the internal medicine department for development of her basic treatment.
Posterior scleritis is a very rare ocular manifestation in Behcet’s disease. It corresponds to scleral inflammation behind the oraserrata. It is the rarest form of scleritis (2%-12%) [4]. Many physiopathogenic mechanisms may be at the origin of scleritis. Immunological scleritis are the most frequent [4,5]. They are linked to two mechanisms:
• Delayed hypersensitivity to scleral antigens linked to a breakdown in immune tolerance spontaneous, post-surgery or following a viral disease.
• Deposits of circulating immune complexes.
Behcet’s disease is a multisystemic disease of unknown etiology. It is ubiquitous but more frequent in the Mediterranean basin and in Japan. It mainly affects young and middle-aged adults with a balanced male-female distribution [1]. Its diagnosis is based on clinical criteria based on the mucocutaneous and ophthalmological manifestations. Several ocular manifestations are described. Posterior scleritis is rarely reported [1,6]. In the literature, only two cases of posterior scleritis in Behcet’s disease have been published recently, one in 2019 by Yanagida et al. [7] and the other in 2021 by Dehghani et al. [8].
In our case, the patient presented with a sudden exophthalmos of the left eye with reduced visual acuity. Ophthalmologic examination revealed retinal folds with papillary oedema. B-scan ultrasonography made it possible to make the diagnosis of posterior scleritis by showing significant scleral thickening with the T-image. Oculo-orbital Computed Tomography (CT) scan and MRI confirmed the thickening of the scleral tissue. The history, the etiological assessment and the ophthalmological examination point to Behcet’s disease. In the study by Yanagida et al. the patient is already followed for Behcet’s disease and he presented eye pain with choroidal folds, retinal serous detachment and scleral thickening on B-scan ultrasonography with retinal vasculitis at fluorescein retinal angiography [7].
In the study by Dehghani et al. the patient was also followed by a rheumatologist for Behcet’s disease and she was on long- term under corticosteroid therapy with immunosuppressants. She presented with reduced visual acuity with eye pain. She was referred to an ophthalmologist whose ophthalmologic examination revealed central retinal serous detachment. The diagnosis of central serous chorioretinioathy was retained, hence the discontinuation of corticosteroid therapy. After two weeks, she returned with severe eye pain, worsening visual acuity, a tyndall of the anterior chamber with hyalitis. The B-scan ultrasonography revealed scleral thickening. The diagnosis was corrected and posterior scleritis was retained [8].
Behcet’s disease is a serious systemic inflammatory disease. It may affect the visual prognosis. Ocular involvement is an important diagnostic criterion.
Although posterior scleritis is a very rare manifestation of Behcet’s disease, ophthalmologists and internists should think about it. Its particularity is the richness of the initial ophthalmologic presentation and the good clinical evolution under treatment.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Benelkadri F, Filali ME, Bouabbadi S, Kriet M (2022) Posterior Scleritis Revealing Behcet's Disease: A Case Report. J Clin Exp Ophthalmol. 13:939.
Received: 31-Oct-2022, Manuscript No. JCEO-22-18565; Editor assigned: 02-Nov-2022, Pre QC No. JCEO-22-18565 (PQ); Reviewed: 16-Nov-2022, QC No. JCEO-22-18565; Revised: 23-Nov-2022, Manuscript No. JCEO-22-18565 (R); Published: 02-Dec-2022 , DOI: 10.35248/2155-9570.22.13.929
Copyright: © 2022 Benelkadri F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.