Mycobacterial Diseases
Open Access
ISSN: 2161-1068
ISSN: 2161-1068
Case Report - (2019)Volume 9, Issue 1
Orbital and Periorbital involvement of tuberculosis is rare even in endemic regions. It is a rare manifestation of extra pulmonary tuberculosis. We report a rare case of discharging Periorbital tuberculosis sinus with no systemic symptoms. Our report emphasises the importance of awareness and high clinical suspicion in cases of nonresolving orbital swellings and infections. It also emphasizes the role of detailed investigations for early diagnosis and prompt treatment of the disease.
Periorbital; Tuberculosis; Sinus; Anti-tubercular therapy
According to WHO report 2008 worldwide epidemic of tuberculosis include 9.2 million new cases and 1.7 million deaths every year [1]. However ophthalmic manifestations occur only in 1%-2% of cases with systemic tuberculosis [2]. Eye involvement is due to haematogenous spread or hypersensitivity to the organism. Clinical presentations of ocular tuberculosis include uveitis, chorioretinitis, retinal vasculitis, panophthalmitis, and phlyctenular conjuctivitis [3]. Simple decline in visual acuity can be associated with macular edema caused by tuberculosis. Anterior uveitis or choroiditis are most common ocular manifestations of tuberculosis [4]. Inability to diagnose the disease can lead to loss of sight and loss of life [5]. Thus early diagnosis and treatment is essential to lessen the burden of blindness in the society.
A 23-year-old boy from poor socio economic background presented to our tertiary care eye center with complaint of recurrent discharging lesion below left eye from last 3 months. There was no history of trauma or other systemic illness. Patient was treated with multiple combinations of oral antibiotics and analgesics from elsewhere with no relief. Patient had good appetite and sleep pattern with no history of weight loss or fever. On examination a discharging sinus was seen 8 mm below the lateral aspect lower lid of left eye with excoriation of skin around it (Figure 1).
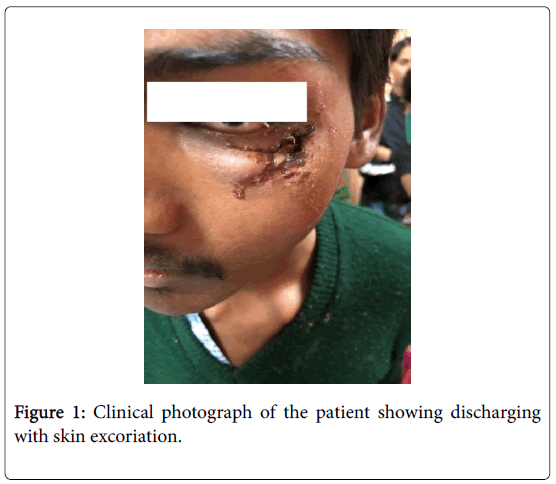
Figure 1: Clinical photograph of the patient showing discharging with skin excoriation.
Mouth of sinus was 10 mm × 10 mm in size with pus filled in it. Eye examination revealed 20/20 vision in both eyes with full and free extra ocular movements and normal pupillary reactions. Slit lamp examination showed clear cornea with quite anterior chamber. Fundus was normal on posterior segment examination. Digital tension in both eyes was normal with negative regurgitation test. Pre auricular and submandibular lymph nodes were palpable on left side which was mobile, non-matted and non-tender. Otherwise patient was afebrile to touch with no icterus, pallor with no constitutional symptoms. Complete hemogram showed haemoglobin 12.3 mg/dl, total leucocyte count 15000 cells/mm2, ESR 60 mm in the 1st hour; Mantoux test 29 mm × 34 mm at 48 hours; chest X-ray was normal. Ziehl-Neelsen (ZN) staining of pus showed Acid fast Bacilli (AFB) along with many pus cells (Figure 2).
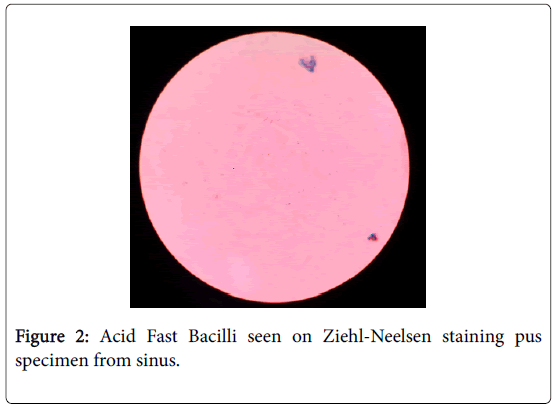
Figure 2: Acid Fast Bacilli seen on Ziehl-Neelsen staining pus specimen from sinus.
On the basis of positive Mantoux, high leucocyte count, high ESR, Z-N staining positive for AFB, diagnosis of tubercular sinus was made. Chronicity of the disease, no response to various combinations of antibiotics, poor socio economic background and unilateral disease, recurrent in nature further supported the diagnosis. Category 1 Antitubercular therapy (ATT) consisting of rifampicin(R) 450 mg, isoniazide (H) 600 mg, pyrazinamide (Z) 1500 mg, ethambutol (E) 1200 mg on alternate day were started. R and H were continued for next fifteen months. After three weeks of ATT sinus showed signs of healing as there was no discharge, no edema and no excoriation of surrounding skin along with decrease in size of sinus mouth (Figure 3).
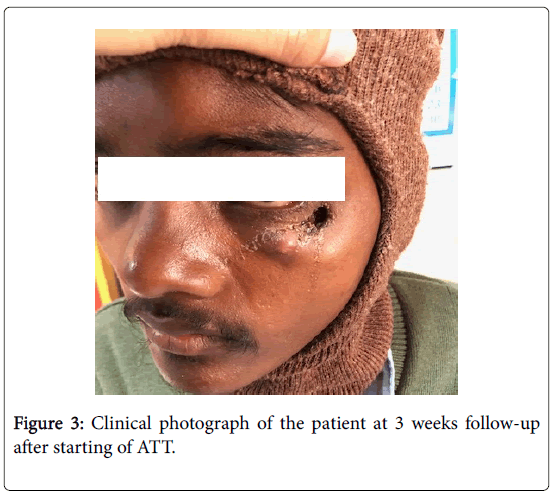
Figure 3: Clinical photograph of the patient at 3 weeks follow-up after starting of ATT.
Complete healing of sinus occurred at 3 months post initiation of ATT. Patient was followed up 2 weekly till the completion of ATT (Figures 4 and 5). Post-treatment 2 year follow up did not show any recurrence.
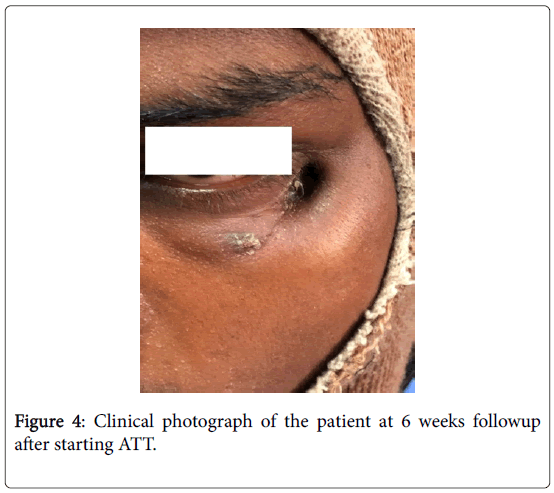
Figure 4: Clinical photograph of the patient at 6 weeks followup after starting ATT.
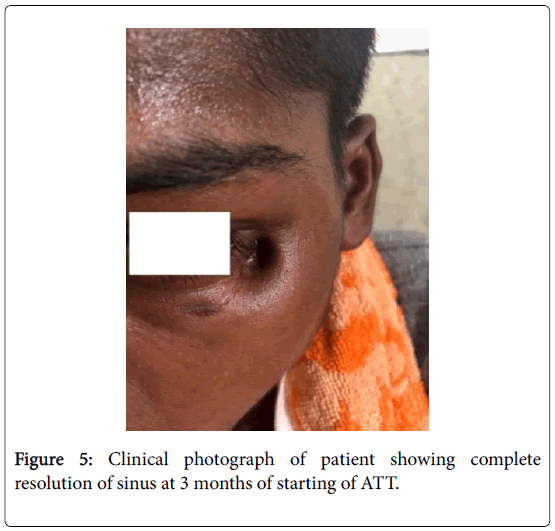
Figure 5: Clinical photograph of patient showing complete resolution of sinus at 3 months of starting of ATT.
Ocular tuberculosis has variety of clinical presentations. Ocular symptoms may mimic ocular tumours or any inflammatory conditions. Abadie reported the first case of orbital tuberculosis in 1881, but the condition is still rare [6]. Isolated tubercular sinus of orbit is rarely reported. Pyogenic granuloma, eosinophilic granuloma, fungal and pyogenic osteomyelitis can be its differential diagnosis. Due to rarity of orbital tuberculosis diagnosis is quite difficult. Involvement of all the orbital margin bones is seen. Lateral wall of orbit usually gets infected by haematogenous spread of infection while medial wall gets the infection from adjacent para-nasal sinus [7]. In many cases trauma acts as precipitating cause of osteomyelitis [8,9]. However in our case there was no history of any trauma, systemic illness and the chest Xray was normal. Lymph nodes get involved by lymphatic spread, as seen in our case [8]. Clinical course of the disease is slow starting from swelling and redness but becomes evident when a sinus is formed. For establishing the diagnosis of tubercular origin in such cases we have to consider all direct and indirect evidences. In our case besides haematological and biochemical investigations, clinical history of disease was taken into account to make final diagnosis. Systemic evidences must be taken into account as these cases are usually secondary to primary infections in lungs or elsewhere. Agrawal et. al have reported histological, microscopic examination of tissue and culture, stain positivity for tubercular bacilli is direct undisputed evidence of the disease which is seen in our case also [8]. Certain principles should be observed while treating such cases which include that the treatment should be continued at least for a period of one year or more on regular basis [8,10], a combination of two or more drugs should be prescribed and that too in adequate dosages. Incomplete, irregular treatment can result in re-factory type of lesions which can even spread to orbit and brain. Surgery is also indicated in severe diseases which may need drainage of abscess, scraping of unhealthy tissues and bones. Ophthalmologist needs to coordinate with pathologist, microbiologist, radiologist and physician for full diagnosis and management of such type of lesions.
Diagnosis of periorbital tuberculosis sinus is challenging. High clinical suspicion and awareness along with haematological and microbiological investigations are very essential to come to accurate diagnosis. Early diagnosis and early initiation of treatment are essential for complete recovery and decreasing morbidity. Complete and regular treatment for a period of at least one year is recommended to prevent recurrence and further spread of the disease.
• Ethics approval for this study was obtained from Maulana Azad Medical College and associate Hospital Ethics Committee.
• No financial support.
• No conflicts of interest.
Citation:
Sharma P, Goyal JL, Chaudhary S (2019) Periorbital Tuberculosis Sinus: A Rare Case Report. Mycobact Dis 9: 272.
Received: 16-Feb-2019 Accepted: 05-Mar-2019 Published: 12-Mar-2019 , DOI: 10.35248/2161-1068.19.9.272
Copyright:
© 2019 Sharma P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.