Maternal and Pediatric Nutrition
Open Access
ISSN: 2472-1182
ISSN: 2472-1182
Research Article - (2025)Volume 10, Issue 1
Background: Maternal depression is identified to be a significant health problem in low and-middle-income countries. Studies have shown maternal depression as a risk factor for poor infant growth. Sever acute malnutrition is results from insufficient energy, fat, protein and other nutrients to cover individual needs.
Objective: To investigate the association between maternal common mental disorder and sever acute malnutrition in children 6-59 months attended in Saint Luke Catholic Hospital and Woliso General Hospital south west Showa, Ethiopia.
Methods: Unmatched case-control study design was employed from January 12/2023 to march 5/2023. One hundred twelve sampled mothers who care givers children (39 cases and 73 controls) were used randomly sample technic selected. Anthropometric measurements (height/length and weight) and MUAC were taken by calibrated instruments. Maternal depression was measured by the Self-Reporting Questionnaire (SRQ-20) developed by the World Health Organization a CMD screening instrument that includes 20 yes/no questions on depression, anxiety and somatic symptoms experienced in the last 30 days. It used ≥ 8 cutoff scores to determine probable cases of mental. Data analysis was done by SPSS 24.0 statistical software. Bivariate and multivariable logistic regression analysis was performed. The association of strength was measured through adjust odds ratio at 95% CI and statistical significance was set at p<0.05.
Result: A total of 39 children (cases) and 73 children (controls) with their mother’s care givers were participated in the study. The percentage of malnourished children was highest 31 (79.5%) in the 6-23 months and lowest 8 (20.5%) among 24-59 months while malnourished children was higher in female 30 (76.9%) than in male 9 (23.1). In multivariable logistic regression age of children, low monthly income, CMD and diarrhea are statistical significance was the level of p<0.05. Children who have a mother with a common mental disorder are 4.444 times (AO=4.444, 95% CI 1.516, 13.028) more likely to develop sever acute malnourished than children who have mothers with no common mental disorder.
Conclusion: Maternal depression carries a significant burden in the mothers of children hospitalized with SAM. Interventions to address routine screening for maternal depression in childbearing age mother, child nutrition programs might contribute to improving child nutritional status and increase crop production.
Sever acute malnutrition; Maternal depression; Malnourished
Children’s age under 59 months is the critical period for rapid physical growth as well as overall child development. Malnutrition is also characterized as a condition that arises from consuming an unbalanced diet in which specific nutrients are absent, in excess (too high) or in the wrong proportion. Malnutrition is also defined as the ingestion of dietary nutrients either insufficiently or entirely. The World Health Organization (WHO) recommends child malnutrition as one of the health indicators for health equity. Sever Acute Malnutrition (SAM) or sever wasting is defined by low Weight for Height (WFH) less than -3 Standard Deviation (SD) of the median world health organization growth standards and a low Mid-Upper-ArmCircumference (MUAC) less than 11.5 cm and presence of bilateral pitting edema. SAM is life-threatening causing globally about one million under-five deaths every year. Maternal common mental disorder is identified to be a significant health problem in low-and-middle-income countries. Maternal depression is a major public health problem that affects mother’s wellbeing and an attitude about life [1].
In Low and Middle-Income Countries (LMICs), most maternal depression remains unnoticed and untreated; this may be due to the reason that depressive symptoms often cannot be differentiate between normal physiological changes during pregnancy and other pathological changes and that screening of maternal depression is not part of service delivery in antenatal clinics in LMICs. Maternal mental illness has severed negative long-term effects on both mothers and infants. There is strong evidence that depression in the postnatal period and low maternal intelligence are also associated with malnutrition in children. A study from low-income and middle-income countries reported that maternal CMD affected 15.6% of women during the perinatal period and 19.8% of women during the postnatal period. Maternal depression is prevalent in lowand middle-income countries. Evidence is mounting up from middle income and low-income countries that the children of mothers with CMD have less optimal growth, cognitive and language development, even when taking social adversity into account. These studies were intended to investigate the association between young children’s nutritional status and maternal CMD by conducted unmatched case-control study to examine differences in maternal mental health issues in mothers with young children hospitalized for severe acute malnourished and mothers with young children hospitalized for other health problems. In 2020 paper assessed the association between maternal postnatal depression and impaired growth of infant. One of the leading causes of morbidity and mortality among children worldwide is malnutrition. It has been directly or indirectly accountable for 60% of the 10.9 million deaths of children under five that occur each year then, these deaths which are frequently linked to improper feeding habits, account for almost 23% of all infant deaths. SAM in children is a major public health problem in developing nations, including subSaharan Africa. According to results from the 2019 Ethiopian Mini-Demography and Health Survey (EMDHS) show that in Ethiopia 37% of children under 5 are stunted, 12% are severely stunted, 7% are wasted and 1% is severely wasted, 21% of all children are underweight and 6% are severely underweight. Regional variations exist, with the highest percentages of children who are wasted in Somali (21%), Afar (14%) and Gambela (13%) and the lowest percentages of wasted children in Addis Ababa (2%) and Harari 4%. In Oromia regional state, the percentage of children who were wasted is 4.7%, stunted 35.6% and underweight 16.1% in EDHS. However, the impact on child physical health and development has received less attention, especially in low- and middle-income countries where poor growth due to under nutrition is a major problem [2].
Women with symptoms of postnatal CMD may have a reduced capacity to practice childcare duties and miss cues for interactions with their children. Mother’s mental health problem, their children could have increased risk of behavioral and emotional problems, cognitive delays and psychiatric morbidity later in their life. Low in educational level, unintended pregnancy, younger in age, being unmarried, lacking intimate partner empathy and support, intimate partner violence, poor social support and having history of mental health problems were risk factors for maternal CMDs. Community determinants such as lack of maternal and child health services, lack of adequate and safe water supply and lack of improved environmental sanitation are other determinants. The nutritional status of children is impacted by a number of factors, including poverty, the absence of exclusive breastfeeding, maternal factors such as inadequate nutrition during pregnancy, inadequate weight gain and inadequate vitamin supplement consumption, illness, environmental factors, socioeconomic/ household factors and environmental factors.
Multiple studies have documented a correlation between maternal postpartum depression and SAM but there are no previously published studies about a possible association between maternal postpartum depression and sever acute malnutrition among children six up to fifty-nine months in the study area. The general district health office needs to have scientific bases on prevalence and possible determinants of sever wasting and maternal postpartum depression for which this study was supply valuable information. Therefore, the aim of this study was to investigate the association between maternal common mental disorder and sever acute malnutrition in children 6-59 months attended Saint Luke Catholic Hospital and Woliso 000 general Hospital south west Showa, Ethiopia.
Significance of the study
Sever acute malnutrition is preventable, treatable and reverse if effective management. Sever acute malnutrition is adverse children who have a mother with a common mental disorder are more likely to develop sever acute malnourished than children who have mothers with no common mental disorder according to this study. Early identification and treatment of maternal depression will have benefits for the mother and child. In health care systems struggling with competing priorities. Therefore, the finding of this study will help the community, government, policy maker, the stakeholders and other different researchers as baseline information, will also use for intervention for health minister, researcher and NGO [3].
Study site
The study was conducted at south west Showa Saint Luke Catholic Hospital and Woliso General Hospital in Woliso town. It is one of the areas found in the south west Showa in Oromia regional state, Ethiopia. It is located along the main road from Addis Ababa to Jimma at a distance of 114 km from the capital city of the country Addis Ababa. Geographically, Dawo, Saden Sodo, Goro and Wenchi districts are the boundaries of this particular area. According to 2007 EC population census of Central Statistical B 6/.2,546 were urban whereas 140,485 were rural residents. There are 37 rural localities and three small towns in the district. According to Woliso district administrative report 30 % of the area is highland and 70% is with temperate ecological zone.
Study period
It conducted between January 12/2023 to March 5/2023.
Study design
It used unmatched case control study design.
The unmatched case-control study calculates the sample size recommended for a study given a set of parameters and the desired confidence level.
Sampling technique
Among children attended in selected hospitals the case and control were selected by lotter method. According to estimated sample from Saint Luke Catholic Hospital collected sample 29 case and 53 control and from Woliso general hospital 10 case and 20 control was collected.
Population
Source of population: All children 6-59 months with SAM or without SAM who was admitted to the pediatric ward and all mothers care givers with young children attended in selected hospitals during the study period.
Study population: For case; children 6-59 months admitted with severely acute malnourished determine by world health organization criteria, such as; Weight-for-height less than -3 SD and/or visible sever wasting and/or Mid Arm Circumference (MUAC) <11.5 cm and/or Edema of both feet and mother who are care taker. For control: Children 6-59 months with normal nutritional status and who was admitted with other health problems and mother who are care takers.
Inclusion criteria
For case: All children 6-59 months and all mothers who caregiver of the child during the attended. Cases was severed acute malnutrition as define in the World Health Organization child growth standard measurements [4].
For control: It was a visited to selected hospitals for other health problems but having normal nutritional status during the study period
Exclusion criteria
Children with physical disable, children with moderate acute malnutrition, if pregnant mother primary caregiver for child and mothers was not the primary caregiver of the child during the study.
Sample size determination
The sample size was estimated using the double population proportion formula by considering; 1.96 for 95% confidence interval and 0.84 for 80% power. By considering these assumptions, the sample size was estimated based on the proportion of similar previous studies.
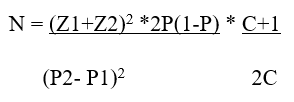
Z1=1.96 Confidence interval
Z2=0.84 power
P1=56.3% proportion of exposure among case
P2=27.3% proportion of exposure among control
P=A average of P1 and P2=0.563+0.273/2=0.418
N=Number of study participant
C=1:2 Ratio of case to control
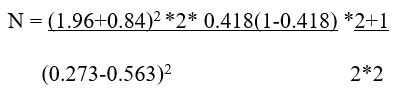
Number of cases 34
Number of controls=68
Total sample size, Number of cases+ umber of controls=102
Non response rate=10%
Total sample size=10% of 102=112 according to this assumption we were taken the final sample size was 112.
Variable
Dependent variable: Sever acute malnutrition.
Independent variable: Socio demographic characteristics, maternal postpartum depression, child caring practices or nutritional care and practice (exclusive breast-feeding practice, complimentary feeding practice and frequency of breast feeding), maternal characteristic (health status during pregnancy, ANC, place of birth and use of extra food during pregnancy and lactation) and environmental health condition (access to save water, access to health facilities).
Data collection instrument
The questionnaire for this study was adapted from the relevant literatures based on the study objective and documents with children identified from the health information management system register used medical record numbers. The data extraction format consisted of sociodemographic data (age, sex, residence), anthropometric measurements (height, weight, MUAC, types of SAM (marasmus, kwashiorkor or marasmuskwashiorkor) and frequency of feeding. Self-reporting questioner for mothers.
Procedure of measurement nutritional status for children
Anthropometry refers to measurements of the body such as; length or height, weight and head circumference length/height was measured without shoes, socks, hair head scurf and ornaments and positioning the subject at the Frankfurt plane by using wooden board inserted with a tape calibrated to read the nearest 0.1 cm. Length of the infants was measured in a recumbent (lying) position using a horizontal wooden length board and movable headpiece. Height was measured for children older than two years of age in standing position into the nearest 0.1 cm used a vertical wooden height board by placing the child on the measuring board and child standing upright in the middle of board and head held erect such that the external auditory meatus and the lower boarder of the eye were in one horizontal plane (Frankfurt plane).
Weight was measured with minimum clothing and no shoes used a hanging scale and electronic beam balance in kilogram for those 6-24 months and 24-59 months to the nearest of 0.1 kg. Children whose height for-age Z-score is below minus two Standard Deviations (-2 SD) from the median of the reference population is considered as stunted. If the weight-for-age Z-score is below minus two standard deviations (-2 SD) from the median of the reference population then the child is underweight. Children whose weight for height Z-score is below minus two Standard Deviations (-2 SD) from the median of the reference population were considered as wasted. Mid Upper Arm Circumference (MUAC) were measured used non-stretchable tape on left mid upper arm to the nearest 1 mm. MUAC below 11.5 cm red color indicates sever acute malnutrition. MUAC of between 11.5 cm and 12.5 cm orange color indicate moderate acute malnutrition and MUAC over 13.5 cm green color indicate child is well nourished.
Edema was assessed by applying medium thumb pressure on upper side of both feet for three seconds. It was diagnosed if a bilateral depression (pitting) remain after the pressure is release.
Measurement of maternal common mental disorder
Maternal common mental disorder is measured by Self Reporting Questionnaire-20 (SRQ-20) developed by WHO
screening tool for assessing maternal mental health. It is a recognized proxy measure for maternal depression and has been validated in multiple developing country settings. It is a scalebased score consisting of 20 yes or no questions which ask about multiple symptoms related to experiences of depression, anxiety, somatic and panic symptoms which have occurred within the preceding 30 days. When a symptom is present within the specified period, the individual is given a score of 1, while 0 represents the absence of symptoms within the same period. The sum of all the scores represents the overall SRQ-20 score and higher scores represent poorer maternal mental health. It considered a cut-off point maternal SRQ score of ≥ 8 to define maternal postpartum depression which was based on previously published work with similar analysis to ours. The questionnaire was developed in English and translated into local language and then back to English to check for its consistency [5].
Data collection technic
In order to data collected two nurses was data collected recruited for each hospital. Diagnosis of sever acute malnutrition was undertaken using WFH<70% and/or MUAC<11.5 cm (SAM) with or without bi-lateral pitting edema to identify eligible and non-eligible subjects as well as to classify those eligible children as cases and controls by experienced nurse who was assigned at each hospital during the study period.
After screening of cases and controls, data was collected using an interviewer-administered structured questionnaire. After informed verbal consent was obtained, data was collected from index mothers or care givers of children 6-59 months.
Data processing and analysis
Data was code, enter, clean and use SPSS version 24.0 software for analysis. Descriptive statistics calculate frequency and percentage by table and chart. Binary and multiple logistic regressions were done to identify independent predictors of sever acute malnutrition. All categorical variables that were associated with the outcome variable in bivariable analyses at 0.25 level of significance were entered into backward multiple logistic regression model and Chi-square (χ 2 ) test was used to test the statistical significance. Were determined for categorical variables using logistic regression analysis with the dependent variable being case or control status and the independent variables being mother’s depression at the time of admission. Variables which demonstrated an association with the outcome variable (SAM) after bivariable logistic regression analysis were inserted into a multivariable logistic regression model to estimate the Adjusted Odd Ratio (AOR) of association between maternal depression and SAM in children and other significant risk factors. A p-value ≤ 0.05 was considered to be significant for all purposes.
Operational definition
Maternal common mental disorder: A score of eight or more than SRQ-20 in the past 30 days was considered as having common mental disorders.
Cases: Were defined as any child between 6-59 months old presented with any of the following world health organization anthropometric indicators for wasted.
Wasted: Were children with weight-for-height z-score less than -2 SD.
Controls: Were defined as children between 6-59 months old considered having normal anthropometric indicators not wasted children with weight-for-height z-score greater than or equal to -2 SD.
Sever acute malnutrition: SAM is defined by the presence of bilateral pitting edema or severe wasting (MUAC<11.5 cm or a WFH<-3 z-score WHO standards in children 6-59 months old.
Bilateral pitting edema: It is defined by bilateral pitting edema of the feet and verified when thumb pressure applied on top of both feet for three seconds leaves a pit in the foot after the thumbs lifted. It is an abnormal infiltration and excess accumulation of serous fluid in connective tissue.
Sever wasting: Sever wasting is also called marasmus.
Bilateral pitting edema and sever wasting: A mixed form of bilateral pitting edema and severe wasting.
Data quality assurance: Data quality was assured by applied properly design and pre-test data collection tool. The tool was pretest used 5% of the sample size one week before the actual data collection period. The purpose of study and proper training of data collectors and supervisors were given.
Ethical consideration: The ethical approval and clearance for the study was obtained from institutional review board, Hawassa University College of Medicine and Health Science. An official letter of permission was obtained from each health facility included in the study. Informed verbal consent was obtained from the study participants after explaining the purpose of the study. To assure confidentiality, name of the participant was not written on the questionnaire.
Socio-demographic and socio-economic characteristics of respondents
A total of 112 subjects 39 case and 73 controls were identified in the study. The response rate was 100%. Majority of mother’s care taker 28 (71.8%) case and 58 (79.5%) controls were married and mothers care takers 9 (23.1%) case and 34 (46.6%) among control were house wife with no occupation while farming 24 (64.1%) case and 23 (31.5%) among controls. Most of 20 (51.3) case and 29 (39.7%) control participants were orthodox religions followers. Regarding educational level majority of mothers are primary school 18 (46.2%) case and 32 (43.8%) control. Most of 31 (79.5%) case and 51 (69.9%) control participants were female. Majority of 25 (64.1%) case and 37 (50.7%) control mother was age less than thirty-five and most of 31 (79.5%) case 35 (47.9%) control were children between six to twenty-three months (Table 1).
| Variable | Case N (%) | Control N (%) |
| Marital status | ||
| Married | 28 (71.8%) | 58 (79.5%) |
| Single | 2 (5.1%) | 3 (4.1%) |
| Divorced | 6 (15.4%) | 7 (9.6%) |
| Widowed | 3 (7.7%) | 5 (6.8%) |
| Religion | ||
| Protestant | 10 (25.6%) | 23 (31.5%) |
| Muslim | 9 (23.1%) | 21 (28.8%) |
| Orthodox | 20 (51.3) | 29 (39.7%) |
| Occupational status of mother | ||
| Farmer | 24 (64.1%) | 23 (31.5%) |
| House wife | 9 (23.1%) | 34 (46.6%) |
| Employed | 4 (10.3%) | 5 (6.8%) |
| ÃÂÂ ÃÂÂ ÃÂÂ Businessmen | 1 (2.6%) | 11 (15.1%) |
| Education level of mother | ||
| Primary school | 18 (46.2%) | 32 (43.8%) |
| Secondary school | 5 (12.8%) | 24 (32.9%) |
| University | 2 (5.1%) | 5 (6.8%) |
| Not educated | 14 (35.9%) | 12 (16.4%) |
| Family size | ||
| One-two | 23 (58.9%) | 36 (49.3%) |
| Above three | 16 (41.1%) | 37 (50.7%) |
| Monthly income | ||
| Less than 1000 birr | 27 (69.2%) | 31 (42.5%) |
| 2000-3000 | 9 (23.1%) | 20 (27.4%) |
| More than 4000 | 3 (7.7%) | 22 (30.1%) |
| Sex of children | ||
| Female | 30 (76.9%) | 52 (71.2%) |
| Male | 9 (23.1 %) | 21 (28.8%) |
| Age of children | ||
| ÃÂÂ 6-23 months | 31 (79.5%) | 35 (47.9%) |
| 24-59 months | 8 (20.5%) | 38 (52.1%) |
| Age of mother’s caregivers | ||
| Less than 35 | 25 (64.1%) | 37 (50.7%) |
| Above 35 | 14 (35.9%) | 36 (49.3%) |
Table 1: Socio-demographic and socio-economic characteristics of respondents Saint Luke Catholic hospital and Woliso general hospital Southwest Showa, Ethiopia (N=112) December 2023.
Child caring practice and nutritional practice
All of the children’s mothers have been breast feed their child. Among these 28 (71.8%) of case and 65 (89.0%) control children had breast feeding that was initiated within one hour after birth and 11 (28.2%) of case and 8 (11%) control mother feed children after the first hour of delivery. Majority of mother’s care taker feed deprive colostrum among these 28 (71.8%) cases and 66 all of the children’s mothers have been breast feed their child. Among these 28 (71.8%) of case and 65 (89.0%) control children had breast feeding that was initiated within one hour after birth and 11 (28.2%) of case and 8 (11%) control mother feed children after the first hour of delivery. Majority of mother’s care taker feed deprive colostrum among these 28 (71.8%) cases and 66 (90.4%) control. About 18 (46.2%) case and 40 (54.8%) control children’s mother was exclusively breast feed their child for the first six months while mother does not feed exclusive breast feed 21 (53%) case and 33 (45.2%) among control. About 22 (56.4%) case and 27 (37.0%) control of the children started complementary feeding in addition to breast feeding at t less than six months while 6 (15.4%) case and 21 (28.8%) control of the children was started complementary feeding in addition to breast feeding at six months and 11 (28.2%) case and 25 (34.2%) for control of the children were started complementary feeding in addition to breast feeding after the six months. Regarding frequency of breast feeding within twenty-four-hour majority of the mothers feed child 3-8 times about 33 (84.6%) case and 48 (65.8%) control while mothers who feed above 8-time 6 (15.4%) case and 25 (34.2%) for control. Majority of children does not consume diversified foods among these children were consumed diversified food groups one to two 29 (74.4%) case and 56 (76.7%) for control. Concerning nutrition information 24 (61.5%) case and 38 (52.1%) control were mothers who taker child did not know about nutrition information (Table 2) [6].
| Variable | Case N (%) | Control N (%) |
| Time of breast-feeding initiation | ||
| Within the first hour of delivery | 28 (71.8%) | 65 (89.0%) |
| After the first hour of delivery | 11 (28.2%) | 8 (11%) |
| Child deprive colostrum | ||
| Yes | 28 (71.8%) | 66 (90.4%) |
| No | 11 (28.1%) | 7 (9.6%) |
| Exclusive breast feed of child during the first six month | ||
| Yes | 18 (46.2%) | 40 (54.8%) |
| No | 21 (53%) | 33 (45.2%) |
| Time of starting complementary food | ||
| Less than six months | 22 (56.4%) | 27 (37.0%) |
| At six months | 6 (15.4%) | 21 (28.8%) |
| After six months | 11 (28.2%) | 25 (34.2%) |
| Frequency of breast feeding within 24 hours | ||
| 3-8 times | 33 (84.6%) | 48 (65.8%) |
| Above 8 times | 6 (15.4%) | 25 (34.2%) |
| A group diversified food feed for child within twenty-four hours | ||
| One-two | 29 (74.4%) | 56 (76.7%) |
| Three-four | 6 (15.4%) | 9 (12.3%) |
| Above four | 4 (10.3%) | 8 (11.0%) |
| Source of nutrition information | ||
| Mass media | 2 (5.1%) | 3 (4.1%) |
| Friends | 2 (5.1%) | 2 (2.7%) |
| Health institute | 11 (28.2%) | 30 (41.1%) |
| None | 24 (61.5%) | 38 (52.1%) |
Table 2: Child caring practices and nutritional practice in Saint Luke Catholic hospital and Woliso general hospital Southwest Showa, Ethiopia (N=112) December 2023.
Maternal characteristic of study participant
Among the study participant 25 (64.1%) case and 37 (50.7%) control of mother’s care givers of children were in the age group less than 35 years and antenatal follow up were practiced in 38 (97.4%) case and 65 (89.0%) control of the mothers. Majority of mothers 31 (79.5%) case and 42 (57.5%) control were did not take extra meal during pregnancy.
Maternal common mental disorder
Maternal common mental disorder among mothers having child with sever acute malnourished was 30.8% CI 1.516,13.028 case while among mothers having children with normal nutritional status was 12.3% control [7].
| Variable | Case N (%) | Control N (%) |
| ANC visit | ||
| Yes | 38 (97.4%) | 65 (89.0%) |
| No | 1 (2.6%) | 8 (11.0%) |
| Maternal extra meal during pregnancy | ||
| None | 31 (79.5%) | 42 (57.5%) |
| One | 5 (12.8%) | 23 (31.5%) |
| Two | 3 (7.7%) | 8 (11.0%) |
| Maternal extra meal during lactation | ||
| None | 13 (33.3%) | 6 (8.2%) |
| One | 18 (46.2%) | 23 (31.5%) |
| Two | 7 (17.9%) | 34 (46.6%) |
| Three | 1 (2.6%) | 10 (13.7%) |
| Maternal common mental disorder | ||
| Yes | 12 (30.8%) | 9 (12.3%) |
| No | 27 (69.2%) | 64 (87.7%) |
| Place of delivery | ||
| Home | 8 (20.5%) | 7 (9.6%) |
| Health institute | 31 (79%) | 66 (90.4%) |
Table 3: Maternal characteristic of study participant in Saint Luke Catholic hospital and Woliso general hospital Southwest Showa, Ethiopia (N=112) December 2023.
Environmental health condition
A majority of participants used latrine availability were 33 (84.6%) case and 65 (89.0%) control. Regarding water utilization majority of mother were used protect spring 23 (59%) case and 47 (64.4%) control (Table 4).
| Variable | Case N (%) | Control N (%) |
| Latrine availability | ||
| Yes | 33 (84.6%) | 65 (89.0%) |
| No | 6 (15.4%) | 8 (11.0%) |
| Domestic waste disposal | ||
| Open field pit | 33 (84.6%) | 59 (80.8%) |
| For other | 6 (15.4%) | 14 (19.2%) |
| Domestic house hold waste disposal | ||
| Open field pit | 32 (82.1%) | 52 (71.2%) |
| Burning | 7 (17.9%) | 21 (28.8%) |
| Source of drinking water | ||
| Covered well | 6 (15.4%) | 4 (5.5%) |
| Open well | 10 (25.6%) | 22 (30.1%) |
| Protect spring | 23 (59%) | 47 (64.4%) |
Table 4: Environmental health condition characteristics study participant in Saint Luke Catholic hospital and Woliso general hospital Southwest Showa, Ethiopia (N=112) December 2023.
Nutritional status of children
Among 39 malnourished children, sever wasted 17 (43.6%), bilateral pitting edema 13 (33.3%) and mixed bilateral pitting edema and sever wasted 9 (23.1%). Majority of malnourished children a MUAC score had between 9.5-11.5 cm. About children 29 (74.4%) case and 68 (93.2% control who are develop diarrhea the past one-week while 31 (79.5%) case and 59 (80.8%) control are develop vomiting (Table 5 and Figure 1).
|
Variable |
Case (N%) |
Control (N%) |
|
Weight in Kg |
||
|
4-6 kg |
29 (74.4%) |
33 (45.2%) |
|
6.1-15 kg |
10 (25.6%) |
40 (54.8%) |
|
Height in cm |
||
|
50-70 cm |
34 (87.2%) |
32 (43.8%) |
|
71-90 cm |
5 (12.8%) |
41 (56.2%) |
|
MUAC score |
||
|
9.5 -11.5 mm |
31 (79.5%) |
0 |
|
11.5- 12.5 mm |
8 (20.5%) |
14 (19.2%) |
|
Above 13 mm |
0 |
59 (80.8%) |
|
Diarrhea in the past one week |
||
|
Yes |
29 (74.4%) |
68 (93.2% |
|
No |
10 (25.6%) |
5 (6.8%) |
|
Vomiting in the past one week |
||
|
Yes |
31 (79.5%) |
59 (80.8%) |
|
No |
8 (20.5%) |
14 (19.2%) |
Table 5: Nutritional status of among children admitted in Saint Luke Catholic hospital and Woliso general hospital Southwest Showa, Ethiopia (N =112) December 2023.
Figure1: Case classification of sever acute malnutrition.
Binary logistic regression analysis
According to crude analysis maternal common mental disorder, educational level of mother, time of breast feeding initiation, sex of children, age of children, monthly income, maternal extra meal during pregnancy, exclusive breast feeding, frequency of breast feed within 24 hour and diarrhea the past one week, deprive colostrum, height of children, weight of children and place of delivery significantly associated with sever acute malnourished children and the variables selected to be included in the multiple linear regression models (Table 6).
| Variable | Category | Case (N%) | Control (N%) | COR (95% CI) | P-value | AOR (95% CI) | P-value |
| Educational level of mothers | Primary school | 18 (46.2%) | 32 (43.8%) | 0.503 (0.19,1.3) | 0.167 | 0.584 (0.171,1.99) | 0.39 |
| Secondary school | 5 (12.8%) | 24 (32.9%) | 0.241 (0.073,0.794) | 0.019 | 0.338 (0.072,1.59) | 0.171 | |
| University or college | 2 (5.1%) | 5 (6.8%) | 0.369 (0.060,2.274) | 0.283 | 0.527 (0.060,4.65) | 0.564 | |
| Not educated | 14 (35.9%) | 12 (16.4%) | |||||
| Monthly income | Less than 1000 birr | 27 (69.2%) | 31 (42.5%) | 4.266 (1.300,13.992) | 0.017 | 5.414 (1.224,23.95) | 0.026* |
| 2000-3000 | 9 (23.1%) | 20 (27.4%) | 2.362 (0.626,8.910) | 0.204 | 1.868 (0.384,9.07) | 0.439 | |
| More than 4000 | 3 (7.7%) | 22 (30.1%) | |||||
| Sex of children | Female | 30 (76.9%) | 52 (71.2%) | 1.346 (0.547,3.314) | 0.518 | 0.757 (0.206,2.78) | 0.675 |
| Male | 9 (23.1 %) | 21 (28.8%) | |||||
| Age of children | 6-23 months | 31 (79.5%) | 35 (47.9%) | 4.207 (1.706,10.376) | 0.002 | 1.695 (0.432,6.649) | 0.003* |
| 24-59 months | 8 (20.5%) | 38 (52.1%) | |||||
| Weight of children in Kg | 4-6 kg | 29 (74.4%) | 33 (45.2%) | 3.515 (1.497,8.256) | 0.004 | 1.742 (0.226,13.454) | 0.595 |
| 6.1-15 kg | 10 (25.6%) | 40 (54.8%) | |||||
| Height of children in cm | 50-70 cm | 34 (87.2%) | 32 (43.8%) | 6.667 (2.491,17.842) | 0 | 5.335 (0.514,55.375) | 0.161 |
| 71-90 cm | 5 (12.8%) | 41 (56.2%) | |||||
| Time of breast-feeding initiation | Within the first hour of delivery | 28 (71.8%) | 65 (89.0%) | 0.313 (0.114,0.863) | 0.025 | 0.237 (0.051,1.097) | 0.065 |
| After the first hour of delivery | 11 (28.2%) | 8 (11%) | |||||
| Child deprive colostrum | Yes | 28 (71.8%) | 66 (90.4%) | 0.27 (0.09,0.076) | 0.014 | 0.417 (0.097,1.792) | 0.24 |
| No | 11 (28.1%) | 7 (9.6%) | |||||
| Exclusive breast feed of child during the first six months | Yes | 18 (46.2%) | 40 (54.8%) | 1.658 (0.757,3.631) | 0.206 | 1.508 (0.613,3.709 | 0.372 |
| No | 21 (53%) | 33 (45.2%) | |||||
| Frequency of breast feeding within 24 hours | 3-8 times | 33 (84.6%) | 48 (65.8%) | 2.694 (0.993,7.305) | 0.052 | 2.483 (0.771,7.996) | 0.127 |
| Above 8 times | 6 (15.4%) | 25 (34.2%) | |||||
| Place of delivery | Home | 8 (20.5%) | 7 (9.6%) | 2.433 (0.810,7.313) | 0.113 | 1.923 (0.561,6.594) | 0.298 |
| Health institute | 31 (79%) | 66 (90.4%) | |||||
| Maternal extra meal during pregnancy | None | 31 (79.5%) | 42 (57.5%) | 1.221 (0.328,4.543) | 0.766 | 1.232 (0.248,6.114) | 0.799 |
| One | 5 (12.8%) | 23 (31.5%) | 0.380 (0.080,1.817) | 0.226 | 0.521 (0.087,3.133) | 0.476 | |
| Two | 3 (7.7%) | 8 (11.0%) | |||||
| Maternal common mental disorder | Yes | 12 (30.8%) | 9 (12.3%) | 3.160 (1.193,8.373) | 0.021 | 4.444 (1.516,13.028 | 0.007* |
| No | 27 (69.2%) | 64 (87.7%) | |||||
| Diarrhea in the past one week | Yes | 29 (74.4%) | 68 (93.2% | 0.213 (0.067,0.679) | 0.009 | 0.137 (0.036,0.526) | 0.004* |
| No | 10 (25.6%) | 5 (6.8%) |
Table 6: Multivariate analysis of factor association with sever acute malnutrition among the child’s attended Saint Luke Catholic hospital and Wliso general hospital Southwest Showa, Ethiopia, (N=112). December 2023.
Multivariate logistic regression
According to logistic regression from total variable four variable are were found to statically significant at the level of p ≤ 0.05. Maternal common mental disorder, monthly income, diarrhea in the past one weeks and children between 6-23 months of study participants have demonstrated a statistically significant association with sever acute malnourished children [8].
Over all maternal common mental disorder
Maternal postpartum depression was including depression, anxiety and somatoform disorders are a public health problem in developed as well as developing countries. This study aims to investigate the association between maternal common mental disorder and sever acute malnutrition in children 6-59 months attended Saint Luke Catholic Hospital and Woliso General Hospital South West Showa, Ethiopia. This study showed that used a cut-off point ≥ 8 of SRQ-20 questionnaire for mother with postpartum depression. Over all percentage of maternal common mental disorder in this study was 30.8% among case and 12.3% control.
Factor associated with sever acute malnutrition
According to this study showed maternal common mental disorder are associated with sever acute malnutrition. Children who have a mother with a maternal postpartum depression are 4.444 times (AOR=4.444,95%CI 1.516,13.028) more likely to develop sever acute malnourished than children who have mothers with no maternal common mental disorder. This study was lower than previous a case control study from Mekelle Ethiopia children who have a mother with a common mental disorder are 6.1 times AOR=6.11, 95% CI (1.18,31.71) more likely to develop acute malnutrition than children who have mothers with no common mental disorder a case control study in Kenya children who maternal depression was markedly higher in cases than in controls (adjusted OR=53.5, 95% CI=8.5-338.3).
To the contrary the current prevalence is higher than the study done in Uganda a case-control study, reported that 42% of mothers of malnourished children were depressed, compared to 12% of mothers of normal weight children admitted to hospital for chronic illness (OR=2.4; 95% CI=1.18-4.79) a cross sectional study in Bangladesh mothers with CMD were approximately two times more likely to have wasted children than mothers with no CMD (adjusted OR=2.25, 95% CI=1.15-4.43. Another a case control study in Sudan children of depressed mothers have 3- fold increased odds for having SAM compared to children of non-depressed mothers (AOR=3.09, p=0.002). Maybe the difference is due to study population and measuring tool or cut of point used for maternal depression.
Both groups of mothers reported low levels of monthly income less than one thousand birr in months. Although 27 (69.2%) of the mothers of cases and 31 (42.5%) control was monthly income less than one thousand birr while about mother care givers monthly income less than 1000 birr 5.414 times (AOR=5.414, 95% CI 1.224,23.950) more exposure to mother who have malnourished children were compare to mothers wellnourished children more than 4000 monthly incomes. This result lower than a case control study done in Kenya having very low income (adjusted OR=77.6 95% CI=5.8-1033.2). May be low financial resource is effect on maternal depression or child nutritional status. Our study finding indicated that SAM among children was significantly associated with diarrhea; as a result, (AOR=0.137, 95% CI 0.036, 0.526). The risk of diarrhea is reduced by 86.3% in children malnourished than were compare to well-nourished children. Malnourished children are vulnerable to diarrhea; diarrhea usually results in weight loss or failure to gain weight [9].
Regarding age of children, children have age between 6-23 months are 1.695 times (AOR=1.695, 95% CI (0.432, 6.649) are more likely to develop acute malnourished than children who have age between 24-59 months. SAM can occur in all age groups, but the impact is more sever among children aged 6-23 months, as this period is extremely important for the child’s optimal growth and development, due to this mental and physical damages that are difficult to reverse can occur due to nutritional deficiencies. Brain and nervous system development begin early in pregnancy and is largely complete when the child reaches the age of two. The timing, severity and duration of nutritional deficiencies during this period affect brain development, physical growth and overall health of the child. Globally, 83% of children less than two years are not getting enough nutritious food appropriate for their age, this denies the infant and young children the nutrients they need at the most critical time in their physical and mental development. Infants and young children especially up to two years of age have the highest nutrient needs than any time in life [10].
According to this study children’s exposure to malnourished are high in between 6-23 months and high percentage of admitted children are female. The percentage of maternal common mental disorder in mothers of admitted children who are hospitalized for sever acute malnutrition was significantly and markedly higher than in mothers of children hospitalized for other health problem. Sever acute malnutrition were significantly associated with maternal common mental disorder, monthly income, diarrhea the past one week and children between six up to twenty-three months. The SRQ-20 used to assess maternal common mental disorder was based on some symptoms in the previous 30 days. Therefore, this study was assessed the association of maternal common mental disorder with sever acute malnutrition among children six up to fifty-nine months.
The burden of maternal common mental disorder is significantly high among mothers of malnourished children, therefore recommended as;
For health institute
•Care for families with malnourished infants should learn to recognize and treat maternal mental health conditions that can impede attainment of desired nutritional goals.
•To asses’ maternal depression before pregnancy and after delivery.
For agricultural institution
•Improving agricultural practice and adapt several crops production; because of majority of respondents doesn’t available diversified crop production in the area. •Promote the production and consumption of culturally accepted, diversified and nutrient-rich foods.
For nutritionist
•Promote optimal breastfeeding while taking necessary precautions during various infectious disease outbreaks. •Promote complementary feeding while ensuring recommended hygiene.
•Wash hands at all critical moments: before eating, handling food or feeding a child, after visiting the toile. •Intervention to address knowledge of nutrition information.
This study may have recall biases since some respondents may not answer truthfully. May not be comfortable to disclose sensitive information during interview. This was hospital-based study, making it difficult to generalize the results to the general population. Moreover, a hospital setting may have influenced the results due to maternal distress associated with the child’s sickness.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Abdet B, Anato A (2025) Maternal Common Mental Disorder and its Associated with Sever Acute Malnutrition Among Children 6-59 Months in South West Showa, Ethiopia: A Case-Control Study. Matern Pediatr Nut. 10:248.
Received: 04-Jul-2024, Manuscript No. mpn-24-32651; Editor assigned: 09-Jul-2024, Pre QC No. mpn-24-32651 (PQ); Reviewed: 23-Jul-2024, QC No. mpn-24-32651; Revised: 13-Jan-2025, Manuscript No. mpn-24-32651 (R); Published: 20-Jan-2025 , DOI: 10.35248/2472-1182.25.10.248
Copyright: © 2025 Abdet B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.