Journal of Phonetics & Audiology
Open Access
ISSN: 2471-9455
ISSN: 2471-9455
Case Report - (2022)Volume 8, Issue 6
An 86-year-old woman with diffuse large B-cell lymphoma developed left vocal fold immobility with dysphonia and aspiration after six cycles of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) therapy. The patient underwent injection laryngoplasty to prevent aspiration pneumonia approximately 5 h after the 7th cycle of chemotherapy. On the 3rd day after the procedure, she visited the emergency room with swelling of the anterior neck and dyspnea with stridor, which had gradually worsened since the previous day, and emergency hematoma removal was performed. On the 14th day after injection laryngoplasty, laryngeal examination performed to observe the vocal cord bruises revealed improvement of edema. Dyspnea and dysphonia observed before emergency surgery resolved completely one month after the operation. It is important to promptly evaluate patients with symptoms such as dyspnea and stridor after injection laryngoplasty and select a safe procedure time for patients receiving chemotherapy to avoid serious complications, such as hematomas.
Laryngoplasty; Dyspnea; Chemotherapy; B-cell lymphoma
Diffuse Large B-cell lymphoma (DLBCL) is the most common lymphoma, and accounts for 25% of non-Hodgkin lymphoid neoplasms [1]. Although Chemotherapy-Induced Vocal-Fold Motion Impairment (CIVFMI) was first reported in 1971, there are few reports of CIVFMI [2]. In most cases, CIVFMI resolved spontaneously after the cessation of chemotherapy, and the duration of symptoms ranged from 7 to 420 days, with a mean of 105.9 days. Injection Laryngoplasty (IL) using short acting injectable materials is a well-established procedure for the treatment of glottic insufficiency from laryngeal pathology, including vocal fold immobility, unilateral vocal fold paralysis, and presbylaryngis.
Herein, we describe a case in which life-threatening side effects occurred after IL for the treatment of CIVFMI accompanied by dysphonia and aspiration in a patient with DLBCL receiving R-CHOP treatment. Furthermore, we reviewed the literature regarding the timing of IL after CIVFMI to prevent potentially serious adverse effects of therapy in patients with lymphoma.
An 86-year-old woman was diagnosed with diffuse large B-cell lymphoma, and started on the R-CHOP regimen on December 11, 2020. On June 30, 2021, she was referred to the department of otolaryngology with complaints of dysphonia and dysphagia that occurred after the 6th cycle of R-CHOP. Flexible laryngoscopy revealed left vocal fold immobility. The left vocal fold was paramedian in position with an approximately 2 mm glottic gap (Figure 1). Laboratory examination showed serum hemoglobin, leukocyte, and platelet levels within normal ranges. She complained of dysphonia, dysphagia, and a high frequency of aspiration during meals; therefore, to prevent aspiration pneumonia, we planned IL on July 21, 2021, when she was scheduled to be admitted to the day-care center for the 7th cycle of R-CHOP. The patient was admitted to the hospital, received chemotherapy with R-CHOP, and approximately 5 h later, IL was performed. After percutaneous local anesthesia of the cricothyroid membrane, 0.6 mL (20 mg/mL) of small-particle stabilized hyaluronic acid (Restylane; Q-Med AB, Uppsala, Sweden), was injected into the left vocal fold (Figure 2). Postoperatively, the patient was discharged after her vital signs stabilized.
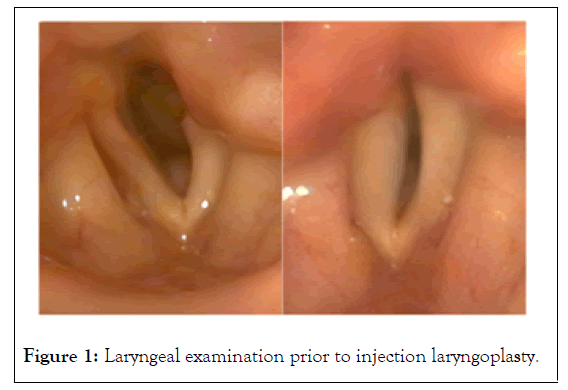
Figure 1: Laryngeal examination prior to injection laryngoplasty.
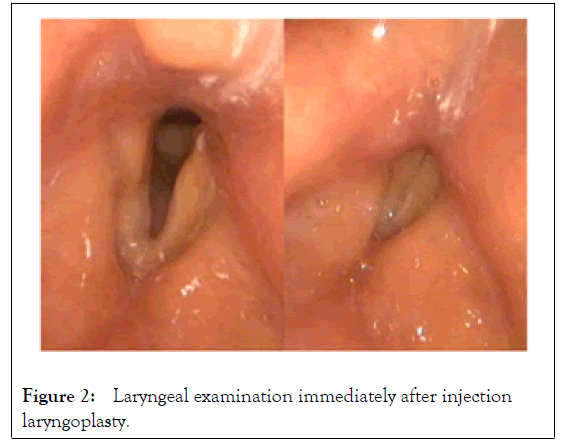
Figure 2: Laryngeal examination immediately after injection laryngoplasty.
Three days after IL, the patient visited the emergency room with anterior neck swelling and dyspnea with stridor that began on the second postoperative day and gradually worsened. Fiberoptic laryngoscopic examination showed bruising and edema of the right vocal fold (Figure 3). Hematological examination revealed thrombocytopenia with a platelet count of 43,000/mcL. Moreover, contrast-enhanced computerized tomography demonstrated acute hematoma with extravasation of contrast agent suggesting active bleeding in the visceral space to the left anterior cervical triangle. In addition, diffuse swelling with infiltration of the bilateral paraglottic space, left anterior cervical triangle, and left lateral neck was noted (Figure 4). The patient was promptly referred to the operating room, and emergency neck exploration under general anesthesia was performed. There was no active bleeding focus, but oozing of blood oozed was observed between the cricothyroid membrane and the bilateral strap muscles. The hematoma was removed, and bleeding was controlled using bipolar and absorbable hemostatic products. We did not perform tracheostomy and completed the operation by inserting a hemovac on both sides of the neck. The patient was observed in the intensive care unit for two days while receiving blood transfusions and filgrastim, a hematopoietic agent for thrombocytopenia control, and was then transferred to the general ward. On the 14th day after IL, laryngoscopic examination to observe her vocal cord bruises revealed improvement of edem. The dyspnea and dysphonia observed before emergency surgery resolved completely within one month postoperatively. Three months after IL, the glottic gap was <2 mm without aspiration or dysphonia (Figure 5). The patient died of lymphoma on December 26, 2021.
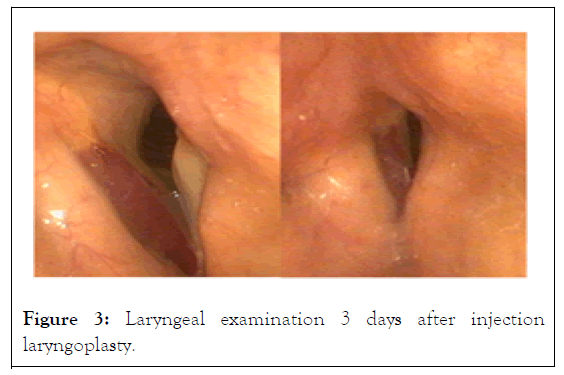
Figure 3: Laryngeal examination 3 days after injection laryngoplasty.
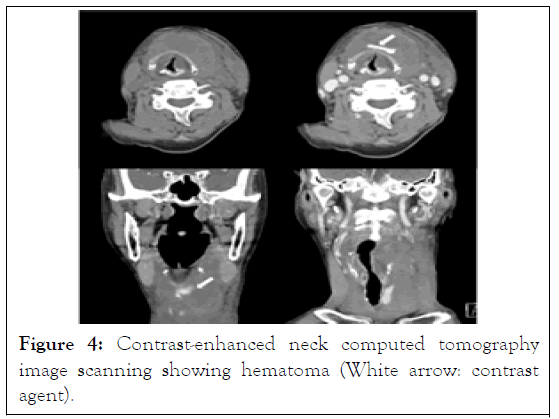
Figure 4: Contrast-enhanced neck computed tomography image scanning showing hematoma (White arrow: contrast agent).
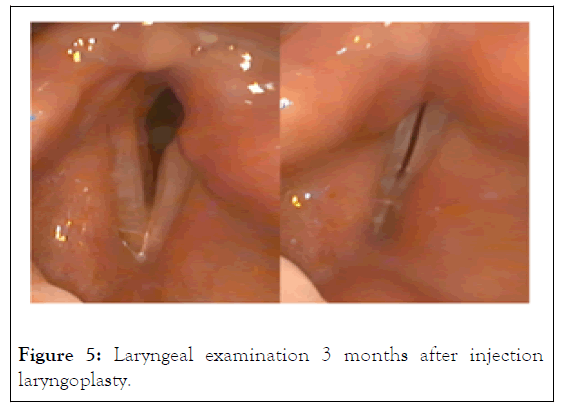
Figure 5: Laryngeal examination 3 months after injection laryngoplasty.
In patients undergoing chemotherapy, motor neuropathy is relatively uncommon compared to sensory neuropathy, and often results from mitotic arrest and subsequent cell apoptosis [3]. CIVFMI is an uncommon complication, with few reports of neurotoxic effects of anticancer agents, such as peripheral neuropathy [2]. Although adverse effects resolve spontaneously after the cessation of chemotherapy in most cases, CIVFMI can present with a variety of aerodigestive symptoms, including dysphagia, dysphonia, and dyspnea [4]. These symptoms are not specific to CIVFMI, but are similar to those associated with vocal-fold motion impairment.
Our patient presented with unilateral CIVFMI with dysphonia and aspiration that was diagnosed as DLBCL and developed after six cycles of the R-CHOP regimen. To prevent aspiration pneumonia, which is highly fatal in patients undergoing chemotherapy, we planned IL. The patient received the 7th cycle of R-CHOP, and approximately 5 h later, IL was performed according to the classical procedure. There were no specific findings during the procedure. After the procedure, the patient's vital signs were stable, and she was discharged. Three days after IL, a life-threatening hematoma with thrombocytopenia with a platelet count of 43,000/mcL developed, and emergency surgery was performed.
To the best of our knowledge, there are no reports of IL in patients undergoing chemotherapy, and there is no literature on the timing of IL. The frequency of thrombocytopenia differs depending on the regimen used, and is 5%-9% with R-CHOP [5]. Thrombocytopenia caused by chemotherapy can cause complications after major surgery as well as simple procedures such as IL. The onset of thrombocytopenia is generally between 7 and 10 days, and it can persist for 30-60 days [6]. The appropriate time interval between chemotherapy and surgery has not been described well in previous studies; however, surgery should be performed when the neutropenic window has passed, which is generally between 3 and 4 weeks.
This case highlights that dysphonia and aspiration may be signs of CIVFMI. Early identification of CIVFMI and appropriate surgical intervention are essential for managing this disorder. IL avoids open surgical procedures such as tracheostomy, has fewer complications, and improves the quality of life in patients with CIVFMI. However, it is important to promptly evaluate patients with symptoms such as dyspnea and stridor after IL and select a safe procedure time for patients receiving chemotherapy to avoid serious complications such as hematomas.
[Crossref] [Google Scholar] [PubMed].
[Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Google Scholar] [PubMed].
Citation: Jeon SY, Jung AR, Gong SJ, Yoon RG (2022) Life-Threatening Event after Injection Laryngoplasty in a Patient Undergoing Chemotherapy: A Case Report. J Phonet Audiol. 8:190.
Received: 15-Nov-2022, Manuscript No. JPAY-22-20122; Editor assigned: 18-Nov-2022, Pre QC No. JPAY-22-20122 (PQ); Reviewed: 02-Dec-2022, QC No. JPAY-22-20122; Revised: 09-Dec-2022, Manuscript No. JPAY-22-20122 (R); Published: 16-Dec-2022 , DOI: 10.35248/2471-9455.22.08.190
Copyright: © 2022 Jeon SY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.