Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research - (2021)
Background: To determine stages of glaucoma and to identify predictors of late presentation.
Methods: A cross-sectional study was conducted in a tertiary eye hospital for four months. All patients diagnosed with primary open angle glaucoma for the first time were inducted and data was collected through an interview-based questionnaire. Classification into stages (early or late) was done based on visual field parameters and optic disc findings. Multivariable logistic regression was conducted to identify predictors of late presentation of glaucoma.
Results: Out of total sample (n=325), 82.2% of the cases (n=267) presented in hospital at late stage of glaucoma. Multivariable logistic regression model explained 18% to 29.6% variation in outcome variable. Late presentation was more likely in individuals with chief complaint of lacrimation (OR=2.45, p-value=0.02) and individuals who had delayed ocular examination as a result of long appointment date in hospital (OR=2.64, p-value=0.01), and individuals living a far distance from the hospital (OR=1.01/km, p-value=0.01).
Conclusion: Geographical accessibility is an important predictor of advanced glaucoma and screening should be focused aggressively on remote areas. It is essential to focus on building the capacity of optometrists and community ophthalmologists to ensure early diagnosis and management of glaucoma at the district level.
Advanced glaucoma; Determinants; Delayed presentation; Factors
Glaucoma is a progressive optic neuropathy that irreversibly damages the optic nerve and thus may lead to a permanent visual loss [1]. It is a significant public health issue, with a global burden of 76 million in 2020, which is expected to increase to 111.8 million by the year 2040 if the current trend continues. According to a recent study, the global prevalence of glaucoma was estimated to be 3.54% [2]. Furthermore, regional differences were observed in the prevalence of different types of glaucoma. Primary Open-Angle Glaucoma (POAG) was the most prevalent type in Africa (4.20%). On the other hand, the region of Asia (1.09%) demonstrated the highest prevalence of Primary Angle- Closure Glaucoma (PACG) [3].
Glaucoma has been one of the major causes of irreversible visual impairment in Pakistan. In Pakistan, a recent meta-analysis has reported the prevalence of glaucoma to be 0.03% in the general population for all ages [4]. Moreover, the prevalence of glaucoma was higher in cohorts of low socioeconomic status as compared to individuals belonging to higher socioeconomic status [5]. A hospital-based study reported that the majority of the cases were diagnosed as primary glaucoma (77.2%) and the rest (22.8%) were classified as secondary glaucoma. 6 Even with the prevalence of less than 1% in the general population, the last national blindness survey conducted around 15 years ago demonstrated that glaucoma was responsible for 7.1% of the total blindness in adults (≥ 30 years) [6]. Furthermore, a hospital-based study reported that 36.5% of the total glaucoma cases had reported a visual acuity of less than 6/18 on the Snellen chart in their better eye [7]. POAG, the most common variant of glaucoma in the country has a significant relationship with non-communicable diseases like Hypertension and Diabetes [8]. Based on this relationship, the burden of glaucoma is expected to increase as non-communicable diseases are projected to increase massively in Pakistan in near future [9]. Another factor related to the increasing incidence of POAG is an increase in population in higher age cohorts of the country [10]. With such a high current and expected burden of glaucoma as well as visual impairment attributed to it, sustainable and evidence-based glaucoma treatment programs are an urgent health care need in the country.
Effective treatment of glaucoma revolves around maintaining the intraocular pressure in a range such that further damage to the optic nerve is either prevented or minimized [11]. The management of glaucoma at the primary level comprises of health education campaigns together with glaucoma screening programs for early detection [12] while secondary management is based on medical and surgical therapies that are aimed at reducing Intraocular Pressure (IOP) to prevent further optic nerve injury [11]. However, advanced treatment modalities may not restore the previously lost visual function. Therefore, early detection of glaucoma is crucial to prevent or minimize glaucoma-associated progressive visual impairment.
The progression of glaucoma is demonstrated by progressive optic nerve damage, which is accompanied by visual field loss, an inevitable sign that is subtle initially and often missed easily [13]. However, population-based screening for visual field abnormalities to diagnose glaucoma is not recommended, as structural damage usually precedes the visual field defects [14]. Alternatively, screening programs using Intraocular Pressure (IOP) measurement and slit lamp bi-microscopy examination for anterior chamber depth evaluation offer a more practical approach because of its convenience of conductance and assessment, especially for developing countries [15]. It has also been proven to be cost-effective in countries where a high visual impairment burden due to glaucoma has been reported [16]. Besides, screening by identifying risk factors such as the family history of glaucoma had also being utilized for glaucoma screening [17], and the effectiveness of this screening method had been established previously in multiple studies [18, 19]. In order to prevent permanent visual loss, population-based screening for the detection of clinical manifestations or risk factors, such as visual field irregularities, increased intraocular pressure, and positive family history of glaucoma, etc. is essential [1].
Despite efforts for early detection, glaucoma is plagued by the issues of late diagnosis owing to its insidious nature, and noncompliance to advised treatment [20]. Studies from South Asian and Middle Eastern countries highlight significant disparities in the presenting stage of glaucoma based on the status of optic nerve damage at the time of diagnosis [21-23]. Late presentation of glaucoma was found to be associated with ethnicity, family history, poor socioeconomic status, poor knowledge regarding disease, commitments associated with the current job, rural residence, and age [23,24]. Variations have been observed in the direction of the association between family history and late presentation of glaucoma. While the majority of the studies reported a relationship between positive family history and late presentation [17,25] studies also demonstrated a relationship between negative family history and delayed presentation [26]. A history of lack of regular eye examination has been observed as a major risk factor for diagnosis at an advanced stage of glaucoma [26]. Disparities have also been reported in the rate of progression and possible prognosis of glaucoma along with multiple factors associated with the progression rate and future medical prognosis [27]. The factors related to the progression and prognosis of glaucoma included the extent of glaucomatous damage at the time of diagnosis, non-compliance with medication, ocular and systemic co-morbidities like cataract, uveitis, optic neuropathies, diabetes, hypertension, and asthma [28].
To the best of our knowledge, there is a lack of data about predictors associated with the presentation of patients at advanced stages of glaucoma in ophthalmology clinics of Pakistan. Different studies from developing countries highlight the factors that result in delayed presentation of glaucoma, such as low socioeconomic status and poor educational level, as well as geographical inaccessibility of healthcare facilities [27-29]. The purpose of this study is to report different stages of Primary Open-Angle Glaucoma POAG (early or late) at the time of the first consultation in a tertiary eye care centre and to determine predictors of its late presentation. This study will be valuable in risk stratification for glaucoma progression and can play a vital role in developing disease prevention strategies.
An exploratory and descriptive cross-sectional study was carried out from December 2019 to March 2020 to assess the presenting stage of POAG and its predictors in a tertiary eye care hospital, Rawalpindi, Pakistan. The glaucoma department of the hospital is fully equipped with specialized human resources as well as all the modern investigative facilities such as Humphrey visual field analyser (Carl Zeiss Ophthalmic Systems, Inc., Dublin, CA, USA), Specular microscopy (SP 2000p; Topcon Corporation, Tokyo, Japan), and Tonometry. Once an initial assessment has been done in the outdoor clinic, the patients were referred to the glaucoma department, if indicated. At that time a scheduled appointment time was provided to the patient who varies from one week to two months, having an average of 28 days.
Study selection criteria
The study population consisted of all individuals (above 16 years of age) presenting for the first time in the glaucoma department with a confirmed diagnosis of POAG in one or both eyes. However, all known glaucoma patients who had received medical treatment elsewhere (for the last one month or more) or had undergone any type of surgery for treatment of glaucoma were excluded from the study. In addition, the exclusion criteria also covered cases diagnosed with other types of primary glaucoma, secondary glaucoma, and ocular hypertension (defined as repeated intraocular pressure measurements of over 21 mmHg without evidence of glaucomatous nerve damage or visual field loss) [30-32]. The sample size was not pre-determined in the study as the researchers wanted to include all the patients presenting with confirmed glaucoma diagnosis during the defined time frame by utilizing consecutive non-probability sampling. This was done to capture disparities in presenting stages of glaucoma for all variables in as much detail as possible and to ensure that different subcategories of all variables have ample sample size for reliable calculation of Odds Ratio (OR). Individuals were recruited into the study based on the status of worse eye concerning the degree of glaucomatous damage.
The criteria to determine the stage of glaucoma (early or late) were selected based on the previously established definition for the presenting stage of glaucoma [28,33] and are described in detail (Table 1).
| Presenting stage of glaucoma* | Clinical findings |
|---|---|
| Cup to Disc Ratio (CDR) is ≥ 0.5 in the more affected eye or if the difference of CDR between two eyes is >0.2 | |
| Early stage | The Mean Deviation (MD) index is between 0dB and -12dB in the more affected eye. |
| No absolute scotomas present within 20° of the fixation point in the more affected eye. | |
| Cup to Disc Ratio (CDR) is ≥ 0.8 in at least one eye. | |
| Late stage | MD index of greater than -12dB in the more affected eye. |
| Field loss present within 5° of fixation and field defect extension present outside 30° in at least one eye. |
*Patients were classified in a certain category even if one of the given criteria for that specific category was fulfilled
Table 1: Presenting stages of glaucoma [24,29].
Data collection strategy
The study was conducted after the approval of the Institutional Review Board (IRB). Data for the study were collected from the participants after obtaining verbal informed consent. The confidentiality of participants was maintained at all stages of the study. A comprehensive clinical evaluation was performed which included slit-lamp bimicroscopy, Intraocular Pressure (IOP) measurement, fundus evaluation including optic disc assessment and evaluation of Cup to Disc Ratio (CDR), pachymetry (For correction of IOP), and automated visual field analysis, which was performed on Humphrey field analyzer (central 30-2 threshold). Intraocular pressure was measured with Goldmann applanation tonometer (GAT AT 900, Haag-Streit, Koeniz,Switzerland), however, Tono-pen (Tonopen XL, Mentor, Santa Barbara, California, USA) was used in cases where the accuracy of applanation tonometry was doubted. The visual field scans that showed fixation losses of greater than 20% or false positive error of greater than 33% were not used for assessment and those cases were graded based on CDR. Clinical examination and assessment of visual field scans were performed by two glaucoma consultants.
Diagnosis of glaucoma (early or late stage) was based on two clinical characteristics i.e. Visual Fields (VF) and CDR, with VF being the preferred attribute. However, CDR was the main choice in cases where results of visual field testing were unreliable because of advanced glaucomatous damage or poor visual status (visual acuity of less than 6/60) [34]. An interview-based questionnaire was used to collect data regarding different possible predictors. The questionnaire was developed based on the socio-ecological model [35] and previous literature [21,22,29]. Afterwards, a complete pilot assessment was done on 50 participants to determine the best way to pose different questions and to determine the average time spent in a single interview. Initially, the questionnaire was developed in the Urdu language (the official language of Pakistan) as the majority of the population was illiterate and understood Urdu conveniently. Later on, it was translated into the English language. On average, the complete questionnaire was filled in 10 minutes (Range=8-13 minutes).
Study variables
The main outcome variable was stages of glaucoma at the time of presentation in a tertiary eye care hospital, which was classified as the early and late stages. All the possible predictors (independent variables) were classified into different categories (Figure 1).
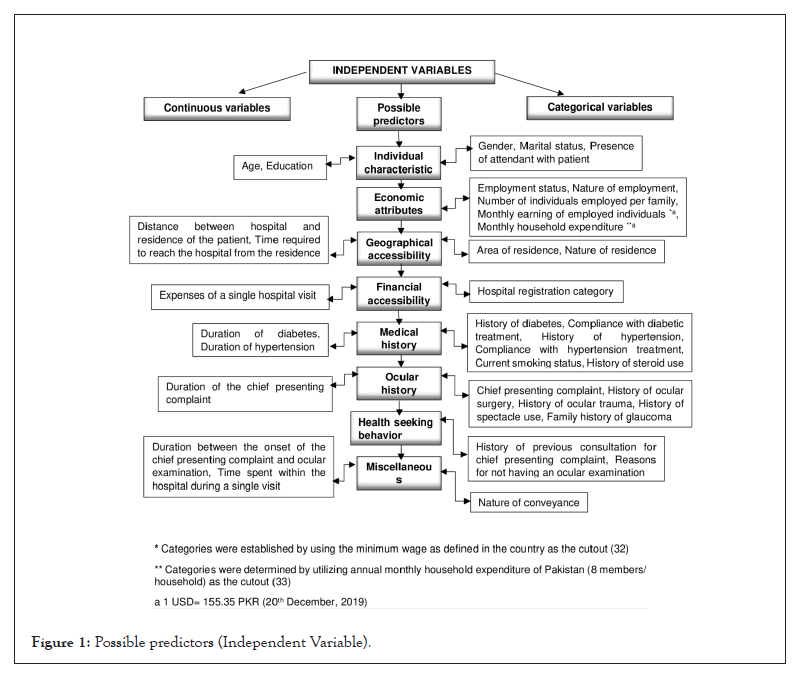
Figure 1: Possible predictors (Independent Variable).
All the analysis was carried out in Statistical Package for Social Sciences (SPSS) version 20. Rigorous data cleaning was carried out on the complete data set before the final analysis. Before the analysis, two of the continuous independent variables were converted using categorical variants for making the results more useful. These variables included monthly income and monthly household expenditure, which were converted by utilizing minimum monthly wages [36] and average household expenditure of Pakistan [37].
Data analysis was done at the individual patient level using data from the worst-seeing eye and conducted in two phases; descriptive analysis followed by inferential statistics. Descriptive statistics were generated for all variables. Categorical data were presented in the form of frequencies and percentages. Mean along with standard deviation and ranges were reported for continuous variables and the median and Interquartile Range (IQR) were the chosen measures for variables that were not normally distributed (heterogeneous). Furthermore, mean and standard deviation were reported in inferential analysis for all continuous variables (homogenous and heterogeneous). A significance level of 5% was used for all inferential statistics. Although the study was exploratory, Bonferroni adjustment values have been provided in multivariable analysis to address the issue of multiple comparisons.
The final significance level for univariable analysis was 5% and for multivariable analysis, it was 0.3% which was calculated by dividing the significance level at 95% confidence interval (0.05) by the number of variables involved in multivariable analysis (16). Binary logistic regression (forced entry method) was used for the univariable as well as multivariable analysis. Initially, the unadjusted odds ratio was calculated for all variables. Afterward, variables depicting statistical significance in univariable analysis were added in the final model for multivariable analysis to calculate the adjusted odds ratio.
The final sample size included in the study was 325. Distribution of the stages of POAG demonstrated that 82.2% (n=267) of total respondents presented at the late stage of glaucoma. More than half (n=213, 69.2%) of total patients had presenting visual acuity of less than 6/18 in the worse eye (Figure 2). The mean value of intraocular pressure in the worst eye was 26.2 ± 11.9 mm of Hg (mercury) ranging from 14 to 74 mm of Hg. Out of the 311 participants, (the rest of the respondents did not have clear media for optic disc evaluation) CDR of 1.0 was observed in 32.6% of cases in the worst eye (Figure 3).
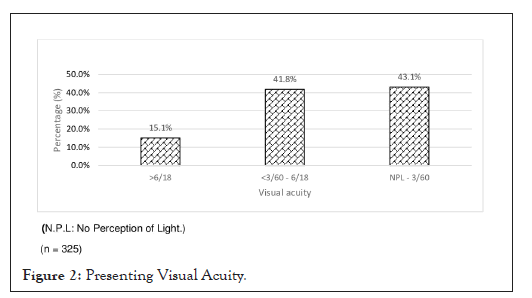
Figure 2: Presenting Visual Acuity.
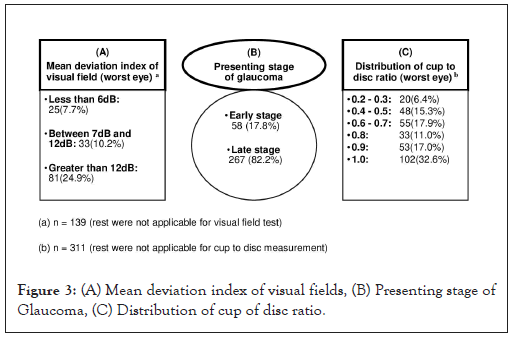
Figure 3: (A) Mean deviation index of visual fields, (B) Presenting stage of Glaucoma, (C) Distribution of cup of disc ratio.
Socioeconomic characteristics
Area of residence was a statistically significant predictor in univariable regression with individuals from rural areas (n=189, 58.2%) having a 2.29 (CI=1.29-4.08, p-value=0.005) higher risk of presenting at the late stage of glaucoma than individuals from urban areas. The median distance travelled to reach the hospital was 131 km (IQR=196 km) ranging from 4 to 811 km. On average, 3.7 ± 2.7 hours (1-18 hours) were spent by participants to reach the hospital. The median expenditure on one visit to ASTEH was 800 PKR (5.14 USD) with an interquartile range of 1150 PKR (7.40 USD), ranging from 50 PKR to 5000 PKR (0.32-32.18 USD). Univariable regression analysis showed that distance to hospital (OR=1.01 per km (1.00-1.02), p-value<0.001), time spent to reach hospital (OR=1.34 per hour (1.14-1.56), p-value<0.001), and expenses of a single visit (OR=1.01 per PKR (1.00-1.02), p-value<0.001) were statistically significant predictors of late presentation (Table 2a).
| Predictors | Frequency (n= 325) n (%) |
Early presentation (n= 58) n (%) |
Late presentation (n=267) n (%) |
Regression coefficient (B) | Unadjusted Odds Ratio (95% C.I.) (I=Reference) |
p-value |
|---|---|---|---|---|---|---|
| Sociodemographic variables | ||||||
| Gender | ||||||
| Male | 214 (65.8%) | 38 (17.8%) | 176 (82.2%) | 0.02 | 1.02 (0.56-1.85) | 0.95 |
| Female | 111 (34.2%) | 20 (18.0%) | 91 (82.0%) | 1 | ||
| Age (years)a | - | 52.2 ± 15.6 | 50.5 ± 16.4 | -0.01 | 0.99 (0.98-1.01) | 0.47 |
| Marital Status | ||||||
| Unmarried | 41 (12.6%) | 6 (14.6%) | 35 (85.4%) | 0.27 | 1.31 (0.52-3.27) | 0.57 |
| Married | 284 (87.4%) | 52 (18.3%) | 232 (81.7%) | 1 | ||
| Education (years)a | - | 10.3 ± 3.9 | 9.4 (3.5) | -0.07 | 0.93 (0.85-1.03) | 0.16 |
| Current employment status | ||||||
| Employed | 141 (43.4%) | 29 (20.9%) | 110 (79.1%) | -0.36 | 0.70 (0.40-1.24) | 0.22 |
| Unemployed | 184 (56.6%) | 29 (15.6%) | 157 (84.4%) | 1 | ||
| Nature of employment | ||||||
| Government | 18(12.8%) | 4 (22.2%) | 14 (77.8%) | -0.11 | 0.89 (0.27-2.95) | 0.85 |
| Private | 123(87.2%) | 25 (20.3%) | 98 (79.7%) | 1 | ||
| Individuals employed (Per household)a | - | 1.4 ± 0.6 | 1.5 ± 0.6 | 0.16 | 1.17 (0.72-1.90) | 0.522 |
| Monthly income (PKR) | ||||||
| ≤ 17,500 | 236 (72.6%) | 40 (16.9%) | 196 (83.1%) | 0.22 | 1.24 (0.67–2.31) | 0.49 |
| >17,500 | 89 (27.4%) | 18 (20.2%) | 71 (79.8%) | 1 | ||
| Monthly household expenditure (PKR) | ||||||
| ≤ 51,100 | 302 (92.9%) | 55 (18.2%) | 247 (81.8%) | -0.4 | 0.67 (0.19-2.35) | 0.54 |
| >51,100 | 23 (7.1%) | 3 (13.0%) | 20 (87.0%) | 1 | ||
| Hospital registration category | ||||||
| Non paying | 227 (69.8%) | 42 (18.5%) | 185 (81.5%) | -0.15 | 0.86 (0.46-1.62) | 0.64 |
| Paying | 98 (30.2%) | 16 (16.3%) | 82 (83.7%) | 1 | ||
| Area of residence | ||||||
| Rural | 189 (58.2%) | 24 (12.7%) | 165 (87.3%) | 0.83 | 2.29 (1.29-4.08) | 0.005* |
| Urban | 136 (41.8%) | 34 (25.0%) | 102 (75.0%) | 1 | ||
| Nature of residence | ||||||
| Ownership | 276 (84.9%) | 44 (15.9%) | 232 (84.1%) | 0.75 | 2.11 (1.05-4.24) | 0.04* |
| Rented | 49 (15.1%) | 14 (28.6%) | 35 (71.4%) | 1 | ||
| Nature of conveyance | ||||||
| Private transport | 249 (76.6%) | 44 (17.7%) | 205 (82.3%) | 0.05 | 1.05 (0.54-2.05) | 0.88 |
| Public transport | 76 (23.4%) | 14 (18.4%) | 62 (81.6%) | 1 | ||
| Presence of attendant | ||||||
| Yes | 261 (80.3%) | 41 (15.7%) | 220 (84.3%) | 0.66 | 1.94 (1.02-3.71) | 0.04* |
| No | 64 (19.7%) | 17 (26.6%) | 47 (73.4%) | 1 | ||
| Distance to hospital (kilometers)a | - | 81.8 ± 97.3 | 174.0 ± 150.7 | 0.01 | 1.01 (1.00-1.02) | <0.001* |
| Time spent to reach hospital (hours)a | - | 2.5 ± 2.1 | 3.9 ± 2.7 | 0.29 | 1.34 (1.14-1.56) | <0.001* |
| Expenses of a single hospital visit (PKR)a | - | 824.1 ± 781.6 | 1471.2 ± 1252.3 | 0.01 | 1.01 (1.00-1.02) | <0.001* |
*Statistically significant, aMean ± Standard deviation has been reported for continuous variables
Table 2a: Socioeconomic characteristics.
Medical and ocular history
Individuals with a positive family history (n=68) of glaucoma had 2.62 times (CI=1.07-6.39), p-value=0.03) higher risk of presenting at the late stage of glaucoma. Univariable analysis showed that chief complaint such as headache (OR=1.84, p-value=0.04), intermittent blurring (OR=1.86, p-value=0.03), lacrimation (OR=2.68, p-value=0.003), and severe vision loss (OR=2.03, p-value=0.02) were significant predictors. The most common reason for not having an eye consultation was negligence regarding the eye condition (n=257, 79.1%). Univariable analysis showed that participants with a delayed visit due to “long hospital appointment schedules” had a 2.01 (95% CI 1.02-3.99) times higher risk of reaching hospital with late stage of glaucoma as compared to patients who reported delay in the examination due to other reasons (Table 2b).
| Predictors | Frequency (n=325) n (%) |
Early presentation (n= 58) n (%) |
Late presentation (n=267) n (%) |
Regression coefficient (B) | Unadjusted Odds Ratio (95% C.I.) (I=Reference) |
p-value |
|---|---|---|---|---|---|---|
| Medical and Ocular history | ||||||
| Current smoking status | ||||||
| Negative | 259 (79.7%) | 39 (15.1%) | 220 (84.9%) | 0.82 | 2.28 (1.21-4.29) | 0.01* |
| Positive | 66 (20.3%) | 19 (28.8%) | 47 (71.2%) | 1 | ||
| Family history of glaucoma | ||||||
| Positive | 68 (20.9%) | 6 (8.8%) | 62 (91.2%) | 0.96 | 2.62 (1.07-6.39) | 0.03* |
| Negative | 257 (79.1%) | 52 (20.2%) | 205 (79.8%) | 1 | ||
| History of ocular surgery | ||||||
| Positive | 71 (21.8%) | 12 (16.9%) | 59 (83.1%) | 0.08 | 1.09 (0.54-2.18) | 0.81 |
| Negative | 254 (78.2%) | 46 (18.1%) | 208 (81.9%) | 1 | ||
| History of spectacle use | ||||||
| Positive | 122 (37.5%) | 25 (20.5%) | 97 (79.5%) | -0.28 | 0.75 (0.42-1.34) | 0.33 |
| Negative | 203 (62.5%) | 33 (16.3%) | 170 (83.7%) | 1 | ||
| Duration of chief complaint (months)a | - | 12.8 ± 10.0 | 12.2 ± 9.6 | -0.01 | 0.99 (0.96-1.02) | 0.65 |
| History of ocular consultation | ||||||
| Positive | 165 (50.8%) | 23 (13.9%) | 142 (86.1%) | 0.55 | 1.73 (0.97-3.08) | 0.06 |
| Negative | 160 (49.2%) | 35 (21.9%) | 125 (78.1%) | 1 | ||
| Suggestion for ocular examination | ||||||
| Positive | 240 (73.8%) | 43 (17.9%) | 197 (82.1%) | 0.02 | 1.02 (0.53-1.94) | 0.96 |
| Negative | 85 (26.2%) | 15 (17.6%) | 70 (82.1%) | 1 | ||
| Delay between onset of complaint and ocular consultation (months)a | - | 9.2 ± 8.2 | 7.8 ± 6.4 | -0.03 | 0.97 (0.91-1.03) | 0.35 |
| Chief presenting complaints | ||||||
| Decrease of Vision | ||||||
| Yes | 288(88.6%) | 53 (18.4%) | 235 (81.6%) | -0.37 | 0.69 (0.26-1.86) | 0.47 |
| No | 37(11.4%) | 5 (13.5%) | 32 (86.5%) | 1 | ||
| Ocular pain | ||||||
| Yes | 188 (57.8%) | 34 (18.1%) | 154 (81.9%) | -0.04 | 0.96 (0.54-1.71) | 0.89 |
| No | 137 (42.2%) | 24 (17.5%) | 113 (82.5%) | 1 | ||
| Headache | ||||||
| Yes | 169 (52.0%) | 23 (13.6%) | 146 (86.4%) | 0.61 | 1.84 (1.03-3.27) | 0.04* |
| No | 156 (48.0%) | 35 (22.4%) | 121 (77.6%) | 1 | ||
| Intermittent blurring | ||||||
| Yes | 170 (52.3%) | 23 (13.5%) | 147 (86.5%) | 0.62 | 1.86 (1.04-3.32) | 0.03* |
| No | 155 (47.7%) | 40 (17.4%) | 115 (82.6%) | 1 | ||
| Lacrimation | ||||||
| Yes | 137 (42.2%) | 14 (10.2%) | 123 (89.8%) | 0.99 | 2.68 (1.40-5.13) | 0.00* |
| No | 188 (57.8%) | 35 (22.4%) | 153 (77.6%) | 1 | ||
| Reasons for delay in ocular consultation | ||||||
| Family/personal issues | ||||||
| Yes | 158 (48.6%) | 27 (17.1%) | 131 (82.9%) | 0.1 | 1.11 (0.63-1.95) | 0.73 |
| No | 167 (51.4%) | 31 (18.6%) | 136 (81.4%) | 1 | ||
| Long appointment dates in hospitals | ||||||
| Yes | 104 (32.0%) | 12 (11.5%) | 92 (88.5%) | 0.7 | 2.01 (1.02-3.99) | 0.04* |
| No | 221 (68.0%) | 46 (20.8%) | 175 (79.2%) | 1 | ||
| Negligence | ||||||
| Yes | 257 (79.1%) | 53 (20.6%) | 204 (79.4%) | -1.19 | 0.30 (0.12-0.80) | 0.01* |
| No | 68 (20.9%) | 5 (7.4%) | 63 (92.6%) | 1 | ||
| Poor income | ||||||
| Yes | 196 (60.3%) | 43 (21.9%) | 153 (78.1%) | -0.8 | 0.49 (0.25-0.88) | 0.01* |
| No | 129 (39.7%) | 15 (11.6%) | 114 (88.4%) | 1 | ||
| Unavailability of conveyance | ||||||
| Yes | 124 (38.2%) | 15 (12.1%) | 109 (87.9%) | 0.68 | 1.98 (1.05-3.74) | 0.0* |
| No | 201 (61.8%) | 43 (21.4%) | 158 (78.6%) | 1 | ||
*Statistically significant, aMean ± Standard deviation has been reported for continuous variables
Table 2b: Medical and ocular history.
Predictors of late presentation of glaucoma
In multivariable analysis, the multiple regression models were constructed by utilizing the 16 variables which demonstrated statistical significance during univariable analysis. The overall model explained 18% (Cox & Snell R2=0.180) to 29.6% (Nagelkerke R2=0.296) of the variation in outcome variable and was statistically significant (χ2 (df)=64.45 (16), p-value<0.001). Presenting with late stage glaucoma was more likely in those living farther from the hospital (OR=1.01 per km, 95% CI=1.00- 1.02; P=0.01), although this finding was not significant at the study’s pre-specified significance level. A chief complaint of lacrimation was also more common in those with late stage glaucoma (OR=2.45, 95% CI=1.15-5.20; P=0.02), although this did not reach the level of statistical significance as well (Table 3).
| Risk factors | Unadjusted Odds Ratio (95% C.I.)* (I=Reference) |
Adjusted Odds Ratio | P-value |
|---|---|---|---|
| Sociodemographic variables | |||
| Area of residence | |||
| Rural | 2.29 (1.29-4.08) | 1.15 (0.53-2.49) | 0.73 |
| Urban | 1 | 1 | |
| Nature of residence | |||
| Ownership | 2.11 (1.05-4.24) | 1.47 (0.64-3.37) | 0.36 |
| Rent | 1 | 1 | |
| Presence of attendant | |||
| Yes | 1.94 (1.02-3.71) | 1.44 (0.68-3.05) | 0.34 |
| No | 1 | 1 | |
| Distance to hospital (kilometers) | 1.01 (1.00-1.02) | 1.01 (1.00-1.02) | 0.01 |
| Time spend to reach hospital (hours) | 1.34 (1.14-1.56) | 0.72 (0.50-1.03) | 0.07 |
| Expenses of a single hospital visit (PKR) | 1.01 (1.00-1.02) | 1.00 (1.00-1.01) | 0.49 |
| Current smoking status | |||
| Negative | 2.28 (1.21-4.29 | 1.69 (0.81-3.50) | 0.16 |
| Positive | 1 | 1 | |
| Chief complaint | |||
| Headache | |||
| Yes | 1.84 (1.03-3.27) | 1.52 (0.76-3.01) | 0.23 |
| No | 1 | 1 | |
| Intermittent blurring | |||
| Yes | 1.86 (1.04-3.32) | 1.57 (0.79-3.11) | 0.19 |
| No | 1 | 1 | |
| Lacrimation | |||
| Yes | 2.68 (1.40-5.13) | 2.45 (1.15-5.20) | 0.02 |
| No | 1 | 1 | |
| Reasons for delay in ocular examination | |||
| Long appointment dates in hospital | |||
| Yes | 2.01 (1.02-3.99) | 2.64 (1.20-5.78) | 0.01 |
| No | 1 | 1 | |
| Negligence | |||
| Yes | 0.30 (0.12-0.80) | 0.48 (0.16-1.42) | 0.19 |
| No | 1 | 1 | |
| Poor income | |||
| Yes | 0.49 (0.25-0.88) | 0.50 (0.25-1.03) | 0.06 |
| No | 1 | 1 | |
| Unavailability of conveyance | |||
| Yes | 1.98 (1.05-3.74) | 1.68 (0.80-3.52) | 0.17 |
| No | 1 | 1 | |
| Family history of glaucoma | |||
| Positive | 2.62 (1.07-6.39) | 2.11 (0.77-5.84) | 0.15 |
| Negative | 1 | 1 | |
*CI based on Bonferroni adjustment=99.7%
Table 3: Multivariate regression analysis.
The objectives of this exploratory study were to segregate the total glaucoma burden of a tertiary eye care hospital into two stages based on the progression of the disease and to determine the predictors associated with patients arriving in tertiary eye care hospitals at a relatively advanced stage of glaucoma. Because of the exploratory nature of the study, Bonferroni adjustment was used to determine the criteria for statistical significance to cater to the problem of multiple comparisons. Although none of the variables included in the final multivariable analysis showed statistical significance based on the criteria of Bonferroni adjustment, the study did identify few variables which can be utilized to plan the screening services and to conduct more focused studies to understand these predictors.
It has been established that presenting at an advanced stage of POAG is an important and common risk factor for permanent visual loss [38]. Our study demonstrated that a greater proportion (82.2%) of glaucoma patients present at the late (advanced) stage of glaucoma in Pakistan. According to recent reports, 50%-90% of glaucoma cases remain undiagnosed in the community [39]. In the absence of proper screening facilities, these cases present in hospitals at relatively advanced stages of the disease. In light of these facts, it can be stated that community-based screening programs for glaucoma are a huge need and inevitable for the effective prevention of blindness in a country. In the context of the overwhelmed health system of Pakistan, screening of highrisk communities is a more viable option than general population screening [40]. Although studies have been conducted in other countries regarding the predictors of the late stage of POAG, understanding these predictors from a local perspective is imperative to identify high-risk communities.
More than 80% of the cases in our study presented at an advanced stage. This finding is very alarming as Pakistan has a higher rate of late presentation of glaucoma in health facilities as compared with other developing countries like Iran (60.2) [29] and Tanzania (58.1%) [41]. Contrarily, studies from developed countries have a much lower proportion of individuals presenting at an advanced glaucoma stage as percentages of 21% and 14% were reported from Canada [42] and England [41] respectively in this regard. A recently published review provided an estimate of 25% [27] for the cases which present at an advanced stage of glaucoma based on multiple studies throughout the world. The comparative assessment shows that situation is very disturbing in Pakistan with respect to the proportion of glaucoma cases presenting late and very serious consideration is required towards this issue in the future.
It was reported in our study that men had 1.02 times higher risk of presenting at a late stage as compared to women, although statistical significance was not achieved. Albeit conservative cultural practices have seen the male gender avail a greater proportion of health care services in the last few decades, currently a rise has been seen in health care utilization [43] and seeking [44] in female gender in Pakistan. This was also evident in our study, as a relatively lesser percentage of females presented at the late stage as compared to males and similar results have been reported in studies of neighbouring countries [38]. Significant differences in the age distribution were not observed with respect to stages of glaucoma (52.2 years in early stage vs. 50.5 years in late stage) in this study. However, the presentation of patients at a relatively lesser age in the advanced stage might be attributed to responsibilities related to employment as an association of perceived job insecurity and poor health care utilization has been established [45]. Further studies to explore this relationship in the local conditions should be conducted.
Similar to age and gender, none of the variables belonging to individual characteristics showed any statistically significant relationship with presenting the stage of glaucoma. This finding in the case of marital status can be attributed to the small sample size in one of the subgroups. However, a lack of relationship between education and the present stage of glaucoma can be because of the generalized poor literacy conditions of the country [46].
In our study, although a greater proportion of unemployed individuals (84.4%) were observed presenting at a late stage as compared to employed individuals (79.1%), no statistically significant relationship was observed between current employment status and presenting stage of glaucoma. Furthermore, nature of employment (p-value=0.22), number of employed individuals per household (p-value=0.52), monthly income (p-value=0.49), monthly household expenditure (p-value=0.54), and hospital registration category (p-value=0.64) did not have any statistically significant relationship with presenting stage of glaucoma. A possible explanation of this can be the ongoing partnership of this tertiary eye hospital with the government in which the government provides financial resources, thereby facilitating the hospital to cater eye health needs of financially weak individuals [30]. The government of Pakistan has been thriving to promote and introduce programs based on public private partnerships in health like the Sehat Sahulat program in the last few years for improving the financial accessibility of the population [47]. Similar initiatives targeting eye health care service delivery at a larger scale can assist in reducing disparities of eye care service utilization associated with employment status which can be vital in ensuring early case detection of glaucoma. It was also reported in this study that the mean expenses of a single hospital visit were 1356 PKR (8.72 USD). Furthermore, the patients presenting at a late stage (1471.2 ± 1252.3 PKR) spent around 650 PKR (4.18 USD) more on average than the patients presenting at early stages of disease (824.1 ± 781.6 PKR) and univariable analysis showed that the risk of presenting late increased by 100 times for an increase of every 100 PKR (0.64 USD) in expenses of a single hospital visit (OR=1.01, p-value<0.001). In developing countries, individuals belonging to low income communities spent 61.5% of their monthly income on glaucoma treatment reducing their financial capacity [48]. To address this kind of issue, the global initiative of Universal Health Coverage (UHC) was announced which implies that all individuals should be able to obtain quality health services as per their need irrespective of their economic background and without facing any financial hardship [49]. Although the goal of UHC is still a long shot for a country like Pakistan and reduction of indirect costs is difficult due to multiple reasons, developing strategies to reduce direct costs by risk pooling, increasing fiscal space, and decreasing out of pocket expenditures in glaucoma treatment can be significant in reducing glaucoma associated visual impairment in the country.
Geographical accessibility was associated with late stage glaucoma in the univariable but not multivariable analysis. Additionally, it was depicted in the univariable analysis that individuals living in rural areas were roughly at two-fold higher risk of presenting at late stage (OR=2.29, p-value=0.005) This was also supported by the evidence that house ownership (OR=2.11, p-value=0.04) is a significant predictor of late presentation, as house ownership has been found to be more common in rural areas as compared to urban areas [50]. This relationship of distance from health facility to individual’s residence and presenting stage of glaucoma can be very effective to focus screening programs in regards to coverage and annual schedules. While rural areas should also be the main focus, more remote areas even in the urban vicinities should also be prioritized in screening projects. However, complete reliance on screening services cannot produce the desired outcomes without strengthening eye care services at the local tehsil and district headquarter hospital to improve opportunistic case detection. An interesting comparison of mass screening services with opportunistic case finding for glaucoma has been provided by Song et al. [51]. The positive predictive value was higher in opportunistic case finding (52.4%) as compared to mass screening (25.5%). Additionally, the cases identified in screening were at a more early stage than opportunistic case finding based on the structural and functional findings. Therefore, while the costeffectiveness of mass screening [14,52] as well as opportunistic case detection [53] for glaucoma has been established for developing countries, a holistic approach integrating both of these methods can massively enhance the proportion of early case detection. The incorporation of tonometry and ophthalmoscopy as a necessary component of comprehensive eye examination along with automated visual field testing has been advocated in Pakistan to improve opportunistic case detection [54]. While the availability of automated visual field analyser is limited in the government sector, there is a need to enforce the application of procedures like tonometry and ophthalmoscopy for optic disc examination to improve case detection of glaucoma suspects along with the establishment of a proper referral pathway for such cases.
Multivariable analysis demonstrated that a positive chief complaint of lacrimation was a predictor of late presentation as individuals who reported lacrimation as a chief complaint had 2.45 times (p-value=0.02) higher risk of presenting at late stage as compared to individuals without this complaint. Although statistical significance was not achieved, this is a unique finding which has not been reported in the literature to the best of our knowledge. A reduction in steady state tear turnover has been reported in newly diagnosed and untreated glaucoma patients, but this was not associated with an increase in the reflex lacrimation sufficient to cause epiphora [55]. While we cannot rule out that this finding was due to chance alone given the large number of risk factors assessed in the present study, lacrimation has been reported as a presenting chief complaint of glaucoma in literature [56]. Although further studies to investigate this relationship are recommended, we also propose the inclusion of glaucoma screening in clinical guidelines for examination and investigation of epiphora and excessive lacrimation as it can be of great significance in early glaucoma detection with very limited resource exemption.
It has been shown in different studies that positive family history contributes to the risk of developing glaucoma. Hypertension and diabetes are also considered as significant risk factors for the incidence of glaucoma [1]. However, our results showed no significant association with these factors. It would seem logical that these patients are more likely to have regular medical examinations which give an opportunity of early referral to ophthalmic setups for their ocular problems which might explain a lack of association of medical and family history of glaucoma with presenting stage. Some researchers have found that cigarette smoking could be a risk factor for Glaucoma [1], while others dispute this association. Univariable analysis showed that individuals who did not have a history of smoking had a 2.28 times higher risk of presenting at an advanced stage of glaucoma.
On average, patients visited hospitals for ocular examination 8 months after the onset of their chief complaint. Long appointment scheduling in tertiary eye hospital was one of the reasons for delayed ocular examination after the onset of ocular complaints. The final multivariable analysis showed it to be a predictor of late presentation of glaucoma as people who had delayed ocular examination because of the appointment schedule of the hospital had 2.64 times (p-value=0.01) higher risk of presenting late in a tertiary hospital. Specialized ophthalmic services for glaucoma are not widely available in Pakistan [57]. Furthermore, over-referral of glaucoma suspects is a significant burden on the hospital services which hinders the early detection of true cases [58]. This signifies the importance of modifying the screening criteria for glaucoma referral especially for developing countries like Pakistan to minimize false positives and over referral.
Establishing rural screening centres as well as strengthening eye care services at the rural level would also help in reducing over-referral and long appointment scheduling in tertiary care centres. More programs like the Sehat Sahulat program should be introduced by the government so that every glaucoma patient can be treated effectively irrespective of their socioeconomic status and without having to face any financial difficulty. Lastly, further research-based studies must be conducted to investigate lacrimation as the chief complaint in the late stage of glaucoma and to use this clinical knowledge in screening centers which can be helpful in the early detection of glaucoma. The costs for the examination and treatment of glaucoma should be decreased so that patients from every socioeconomic background can get the benefit.
This study had certain strengths as well as limitations. The results should be generalizable to the hospital-based studies in Pakistan as well as other geographically and socioeconomically similar countries. However, a limited sample size because of the limited time duration for completion can hamper the generalizability of this study. A possible limitation is the influence of recall bias as patients had to answer different questions. Lastly, studies conducted in subspecialty departments are usually affected by selection bias because of a limited number of patients. Although selection bias was an issue in this study it was not a major one. This is because a confirmed diagnosis and treatment of glaucoma require sophisticated visual field testing as well as other diagnostic facilities that are not available in local community ophthalmologists’ clinics. Therefore, the majority of the cases are referred as suspected glaucoma patients to the tertiary eye care centres.
Significant disparities were reported regarding the stage of presentation of POAG in this study. There is no comprehension of the disease nature among masses, leading to a non-serious attitude towards the severity of this disease and non-compliance with treatment. It is essential to focus on building the capacity of optometrists and community ophthalmologists in the diagnosis and management of glaucoma at the district level. There is a need to develop screening programs in rural areas, equipping basic health units and rural health centres with appropriate tools for glaucoma screening to detect cases at an early stage as patients. Considering the low literacy rate of Pakistan, we should direct our attention towards simplifying glaucoma education so that the general population can have a better idea about this disease.
Ethical approval
The study was conducted in accordance with the Guidelines for Good Clinical Practice after approval of protocol by the ERB of Al-Shifa Trust Eye Hospital, Rawalpindi, Pakistan.
Acknowledgments
None
Funding
None
Competing interests
None declared
Citation: Arshad H, Ali M, Khan AS, Akhtar F, Mueed A (2021) Late Presentation of Primary Open Angle Glaucoma and Its Predictors at a Tertiary Eye Care Hospital in Pakistan. J Clin Exp Ophthalmol. 12:899.
Received: 26-Oct-2020 Accepted: 09-Nov-2021 Published: 16-Nov-2021
Copyright: © 2021 Arshad H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.