Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2023)Volume 14, Issue 1
Background: As an added high-risk group, ophthalmic Health Care Personnel (HCP) are actively providing emergency eye care services and enthusiastically participating in the prevention and control of the COVID-19 pandemic. Hence, this study aimed to assess the Knowledge, Attitude and Practice (KAP) level among ophthalmic HCP towards the COVID-19 pandemic.
Methods: A web-based cross-sectional study was conducted during the period of lockdown among ophthalmic HCP including consultant ophthalmologists, residents, optometrists, ophthalmic assistants, nursing staff, and other paramedics of eye care centers in Nepal. The KAP questionnaire was designed and distributed online. Data were analyzed using the Chi-square test, Pearson correlation, and binary logistic regression. All tests were performed at a 95% Confidence Interval (CI) and a p-value <0.05 was considered statistically significant.
Results: Of 694 participants, the majority was male (59.1%) in the age group 31-40 years (41.5%) and from tertiary eye centers (68.9%). Among ophthalmic HCP, there were 29.8% consultant ophthalmologists, 22.6% residents, 23.3% optometrists, 15% ophthalmic assistants, and 9.2% other ophthalmic paramedics, 11.7% working as front-liners in COVID-19 centers. Findings showed that 98.1% had good knowledge, 59.4% had a positive attitude and only 13.3% had good practice regarding COVID-19. Binary logistic regression analysis demonstrated the age of HCP to be a significant determinant of good knowledge (Crude Odds Ratio (COR)=0.72, 95%CI=0.62-0.82), positive attitude (COR=0.92, 95%CI=0.90-0.94) and good practice (COR=1.16, 95%CI=1.10-1.21). Lower odds of poor practice was seen among junior resident (COR=0.26, 95% CI=0.14-0.47) and higher odds of poor practice was seen among HCP with job experience of 5-10 years (COR=2.38, 95% CI=1.23-4.60) towards COVID-19 pandemic.
Conclusion: The majority of ophthalmic HCP have good knowledge, insufficient positive attitude, and inadequate evidence-based practice towards the COVID-19 pandemic in Nepal. Hence, this study conclusively recommends modifying existing guidelines and formulating new policies to improve KAP among ophthalmic HCP to effectively control the spread of COVID-19.
Knowledge; Attitude; Practice; COVID-19; Specialists
Mankind is amid a global pandemic at an unprecedented scale due to coronavirus disease 2019 (COVID-19). Initially called then Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) when it was first detected by the Center for Disease Control (CDC) China, it was, later designates COVID-19 by the World Health Organization (WHO) on January 7, 2020 [1,2].
Dr. Li Wenliang, a Chinese ophthalmologist was among the first to sound an alarm, about the possible emergence of a new and unusual type of pneumonia. On February 7, 2020, he died of respiratory failure as a complication of the same disease he had tried to warn the world about. Although labeled as a whistleblower. Initially, he was soon regarded as an international hero for his sincere efforts to make the world alert about a danger lurking ahead [3,4].
As compared to other critical care specialists, although ophthalmologists are less involved in lives saving procedures, they may be the first to see and diagnose new emerging diseases [5].
By January 30, WHO had declared COVID-19 as a Public Health Emergency of International Concern (PHEIC) due to its rapid spread to more than two hundred countries [6]. Then on March 11, 2020, the inevitable announcement roared throughout the planet-WHO announced a first global pandemic in over a hundred years [7]. As of mid-June 2020, there have been more than 7 million confirmed cases and 400,000 mortalities across the globe with still no signs of relief on the horizon [8].
Nepal has the most vulnerable geographical location for this global health crisis. Adding to its owes, is the fact that it is a landlocked country between China-the epicenter of the pandemic; and India-currently a hotspot with the 4th largest cluster in the world [8]. The vast porous border that Nepal shares with India have added more salt to the wound as a large number of unorganized migrations is occurring daily. The regions of both nations around the border have also currently been tagged as red zones as more and more cases are being diagnosed every day [9]. It was evident from the beginning when the first COVID-19 case was diagnosed in Nepal that much of the suffering will be due to imported cases. Many also indicated that it will be impossible to escape from COVID-19 and that great preparation will be required if we were to limit the suffering [10]. Till mid-June 2020, Nepal has more than 6000 confirmed cases and 19 mortalities.
Due to various restrictions and lockdown, COVID-19 has affected all services including eye care facilities. In Nepal, ophthalmic health care personnel are still actively providing emergency and not allowing much-needed services to falter. At the same time, they have also been enthusiastically participating in the prevention and control of COVID-19. Especially medical colleges and teaching hospitals that are also providing emergent eye care services have also been converted into special COVID-19 hospitals/centers. As a result, ophthalmic Health Care Personnel (HCP) have become directly or indirectly involved in the service of COVID-19 patients [11].
Owing to the prerequisites and requirements in an ophthalmic examination, it is almost impossible to maintain a physical distance or time restrictions as recommended by the WHO or the Center for Disease Control (CDC). The distance between the patient and the ophthalmic HCP is as close as 20 centimeters in most circumstances and the time required for a comprehensive ocular assessment also easily surpasses the guidelines. Contact with the patient is inevitable [12].
Although the risk of transmission is low; acute viral conjunctivitis can be a feature of COVID-19 and tear film (ocular secretions) has the potential for viral transmission [13]. Ophthalmic health care personnel are at high risk compared to other health workers. Due to the frequent exposure to suspected or infected patients, HCP are at serious occupational health risk of COVID-19 [14]. Thus, HCP must have updated knowledge on the source, transmission, symptoms, and preventive measures which will help to impose a positive attitude and good practice to assure the safety and protection of not only themselves but also of their patients [15].
Various studies have shown that lack of knowledge and misunderstandings among HCP lead to delayed diagnosis, acceleration of the spread, and the establishment of a dangerous chain of transmission [16]. This will not only lead to infection in HCP but will make them a potential super spreader. Such missed events have already been documented around the globe.
A good knowledge, positive attitude, and evidence-based practice against COVID-19 are very important to fight against this pandemic. Hence, during the period of lockdown when social distancing was a must, this web-based study was designed to assess the level of knowledge, attitude, and practice among ophthalmic health personnel towards COVID-19.
We believe the results will enable us to assess the level of Knowledge, Attitude, and Practice (KAP) among ophthalmic health personnel, which is essential at the moment. With the help of the results of the study, we can ourselves know where stand-on in this crisis. This can further help to design essential plans required for training and interventions, subsequently providing optimum eye care services at the time of pandemic without compromising the protection and safety of the ophthalmic health care personnel and patients.
Study design and duration
A web-based cross-sectional study was conducted from May 20th to June 9th, 2020 during the period of lockdown in Nepal. There were an increasing number of COVID-19-positive cases, as it was not feasible to conduct a population-based study. So, following the norms of social distancing web-based online data collection method was selected.
Study population, sampling and data collection method
In the present study, ophthalmic Health Care Personnel (HCP) i.e. ophthalmologists, consultants, residents, optometrists, ophthalmic assistants and others (nursing staff, opticians, orthoptics) who were directly involved or not involved in the COVID-19 pandemic prevention and control, working in different eye care health centers of Nepal during this period of COVID-19 era were the study population.
The sample size was calculated using the Yamane formula. The total sample size was estimated to be 694 with a 5% margin of error at a 95% confidence interval. The study population unit was selected using a convenience method of sampling. The survey was started on 20th May and response acceptance was closed on 9th June 2020 after the required sample number achieved. A total of 694 participants were included in the final analysis of this study.
A structured questionnaire was self-designed with the help of a literature review of various studies on COVID-19. The questionnaire was created using the google-form platform and was distributed via online tools like Emails, Viber, WhatsApp, Facebook/Messenger, Twitter, and Instagram to all participants across the country. Instant online consent was taken from each participant before participating in the survey after a brief introduction to this survey. Pieces of information provided by participants were kept completely confidential and all the data collected in this research were anonymous. All participants’ responses were recorded on google-forms.
Measure
The questionnaire used in the present study consisted of 31 items for assessing knowledge (10 items), attitude (10 items), and practice (11 items) among ophthalmic health care personnel. The KAP questionnaire was developed based on the study by Ahmed Asaad towards the Middle East Respiratory Syndrome Coronavirus (MERS CoV) [17], the question and answer about COVID-19 in the webpage of WHO [18], COVID-19 ophthalmology practice guidelines by American Academy of Ophthalmology (AAO) and Nepal Ophthalmic Society (NOS) [19,20].
Questionnaire pretesting was done by the principal investigator in the presence of a public health expert and an eye specialist, among 10 ophthalmic health care personnel from B.P. Koirala Institute of Health Sciences (BPKIHS), (the same sorts of sample that is included in this study) using personal interview method through zoom, video-conferencing application. As per results and recommendations, questionnaires were further modified to increase their intelligence and validity. Validation was done by content validation method i.e. experts in the area of our topic (a public health expert and an eye specialist). Pre-tested data were not included in the final analysis of this study.
Questionnaires were divided into four different sections in google-form. The first section consists of socio-demographic characteristics of the study population i.e. age, gender, level of eye care center (i.e. primary, secondary, tertiary and medical college and teaching hospital), location of eye center according to provincial division, position/designation of HCP working in eye center and their job experience (<5years, 5-10 years and >10 years), whether eye center having any COVID-19 cases management facility, level of COVID-19 facility (level 1,2,3 or COVID-19 clinic as per Ministry of Health and Population (MoHP)) and whether ophthalmic HCP involved in COVID-19 cases management are front-liners or second-liners and not involved at all.
Section two consisted of 10 items of questionnaires assessing knowledge of ophthalmic HCP towards COVID-19 pandemic with multiple choices answering options i.e. Yes, No and I don’t know. The correct response (Yes) was assigned 1 point while the incorrect response (No and I don’t know) were assigned zero points. Total maximum scores assigned were 10 with cut off level of greater than or equal to 7 for good knowledge, and less than 7 for poor knowledge.
Section three consisted of 10 items of questionnaires to assess the attitude of ophthalmic HCP towards the COVID-19 pandemic with multiple-choice options to answer. Responses were recorded on 5 points Likert scale as follows- strongly disagree (1 point), disagree (2 points), undecided/neutral (3 points), agree (4 points), and strongly agree (5 points). Total score ranged from 10 to 50 with an overall higher mean score indicates a positive attitude toward COVID-19.
Section four consisted of 11 items of questionnaires to assess the practice of ophthalmic HCP towards COVID-19 pandemic with multiple-choice options to answer (Yes, Sometimes and No). The correct response (Yes) was assigned 1 point while the incorrect response (Sometimes and No) were assigned zero points. Total maximum scores were 11, cut off level of greater than equal to 7 for good practice, and less than 7 for poor practice.
Statistical analysis
Responses recorded in google-form were exported to and cleaned in Microsoft Excel 2019 and later imported to SPSS Statistics for Windows, version 20 (SPSS Inc., Chicago, Ill., USA) for statistical analysis. The data were summarized in terms of frequency, percentage, mean and Standard Deviations (SD) and presented in the form of bar diagrams and tables. The confidence interval around the proportion was determined using the Clopper-Pearson method. Chi-square tests were applied to determine the association of knowledge (good vs. poor), attitude (positive vs. negative), and practice (good vs. poor) with socio-demographic characteristics. Pearson correlation was applied to determine the correlation between knowledge, attitude, and practice scores. To find possible determinants of good knowledge and practice, a binary logistic regression analysis was applied. Throughout the study, all tests were two-tailed and carried out at 95% CI and a p-value less than 0.05 was considered statistically significant.
Socio-demographic characteristics of participants
The socio-demographic characteristics of the participants were listed (Table 1).
| Characteristics (N=694) | n (%) or mean ± SD |
|---|---|
| Age (in years) | 34.6 ± 6.9 |
| 20-30 years | 272 (39.2) |
| 31-40 years | 288 (41.5) |
| 41-50 years | 122 (17.6) |
| 51-60 years | 12 (1.7) |
| Gender | |
| Male | 410 (59.1) |
| Female | 284 (40.9) |
| Ophthalmic Health Care Personnel (HCP) | |
| Consultant | 207 (29.8) |
| Junior resident | 157 (22.6) |
| Optometrist | 162 (23.3) |
| Ophthalmic assistant | 104 (15.0) |
| Others* | 64 (9.2) |
| Province | |
| Province 1 | 224 (32.3) |
| Province 2 | 119 (17.1) |
| Bagmati | 175 (25.2) |
| Gandaki | 45 (6.5) |
| Province 5 | 97 (14.0) |
| Karnali | 15 (2.2) |
| Sudur Paschim | 19 (2.7) |
| Level of the eye center | |
| Primary | 25 (3.6) |
| Secondary | 62 (8.9) |
| Tertiary | 478 (68.9) |
| Medical college and teaching hospital | 129 (18.6) |
| Job experience | |
| <5 years | 490 (70.6) |
| 5-10 years | 158 (22.8) |
| >10 years | 46 (6.6) |
| COVID-19 center | |
| Yes | 163 (23.5) |
| No | 531 (76.5) |
| Level of COVID-19 center (N=163) | |
| Level 1 | 0 |
| Level 2 | 4 (2.5) |
| Level 3 | 77 (47.2) |
| COVID-19 clinic | 82 (50.3) |
| Involvement in COVID-19 cases management | |
| Frontliners | 81 (11.7) |
| Second liners | 105 (15.1) |
| None | 508 (73.2) |
Note: n: Frequency; %: Percentage; SD: Standard Deviation; Others* includes nursing staff, optician and orthoptics
Table 1: Socio-demographic characteristics of participants.
Knowledge, attitude and practice
Figures below showed responses of ophthalmic health care personnel about questionnaires about knowledge, attitude and practice towards COVID-19 pandemic (Figures 1-3).
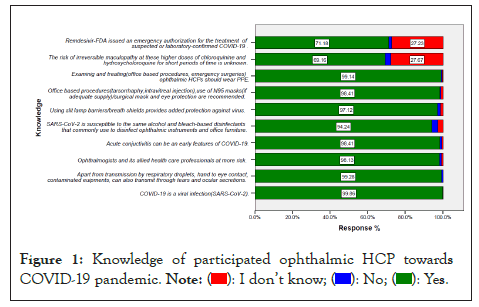
Figure 1: Knowledge of participated ophthalmic HCP towards COVID-19 pandemic. 
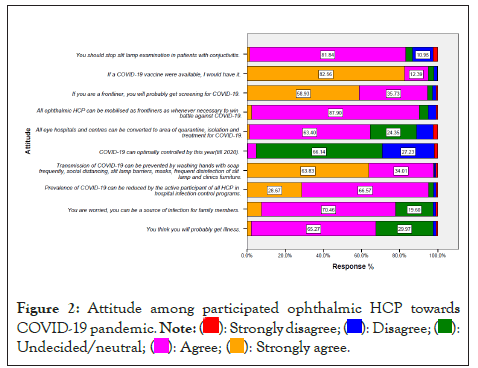
Figure 2: Attitude among participated ophthalmic HCP towards COVID-19 pandemic. 
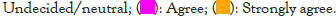

Figure 3: Practice of participated ophthalmic HCP towards COVID-19 pandemic. 
In this study, the majority of respondents 98.1% (95% CI: 96.8-99.0) had good knowledge regarding COVID-19. Among all participants, 59.4% (95% CI: 55.6-63.0) participants had a positive attitude towards COVID-19. To our most surprise, only 13.3% (95% CI: 10.8-16.0) following good practice regarding COVID-19 pandemic (Figure 4).
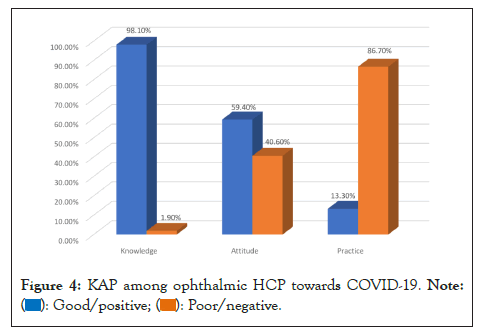
Figure 4: KAP among ophthalmic HCP towards COVID-19. 
Factors associated with KAP
Tables 2 and 3 presents the factors associated with knowledge, attitude and practice among ophthalmic HCP. Knowledge was significantly associated with age (p=0.019), designation HCP (p<0.001), involvement in COVID-19 case management (p<0.001) and association with COVID-19 center (p=0.001). Attitude towards COVID-19 was significantly associated with age (p<0.001), designation HCP (p<0.001), job experience (p=0.005), level of eye center (p<0.001) and involvement in COVID-19 case management (p<0.001). Practice was significantly associated with age (p<0.001), designation HCP (p<0.001), job experience (p=0.029), level of eye center (p<0.001), involvement in COVID-19 case management (p<0.001) and affiliation to COVID-19 center (p=0.001) (Tables 2 and 3).
| Characteristics | Knowledge* | Attitude** | Practice*** | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N=694 | Good | Poor | P | Positive | Negative | P | Good | Poor | P |
| Age | |||||||||
| 20-30 years | 262 (96.3) | 10 (3.7) | 0.019 | 135 (49.6) | 137 (50.4) | <0.001 | 57 (21) | 215 (79) | <0.001 |
| 31-40 years | 286 (99.3) | 2 (0.7) | 170 (59) | 118 (41) | 29 (10.1) | 259 (89.9) | |||
| >40 years | 133 (99.3) | 1 (0.7) | 107 (79.9) | 27 (20.1) | 6 (4.5) | 128 (95.5) | |||
| Gender | |||||||||
| Male | 402 (98) | 8 (2) | 0.855 | 247 (60.2) | 163 (39.8) | 0.803 | 57 (13.9) | 353 (86.1) | 0.547 |
| Female | 279 (98.2) | 5 (1.8) | 165 (58.1) | 119 (41.9) | 35 (12.3) | 249 (87.7) | |||
| Designation HCP | |||||||||
| Consultant | 206 (99.5) | 1 (0.5) | <0.001 | 158 (76.3) | 49 (23.7) | <0.001 | 19 (9.2) | 188 (90.8) | <0.001 |
| Junior resident | 156 (99.4) | 1 (0.6) | 93.2 (71.3) | 63.8 (28.7) | 44 (28) | 113 (72) | |||
| Optometrist | 159.0 (99.4) | 3.0 (0.6) | 135 (83.3) | 27 (16.7) | 12 (7.4) | 150 (92.6) | |||
| Ophthalmic assistant | 97 (93.3) | 7 (6.7) | 4 (3.8) | 100 (96.2) | 10 (9.6) | 94 (90.4) | |||
| Others | 61 (95.3) | 3 (4.7) | 3 (4.7) | 61 (95.3) | 7 (10.9) | 57 (89.1) | |||
| Job experience | |||||||||
| <5 years | 479 (97.8) | 11 (2.2) | - | 272 (55.5) | 218 (44.5) | 0.005 | 74 (15.1) | 416 (84.9) | 0.029 |
| 5-10 years | 158 (100) | 0 | 110 (69.6%) | 48 (30.4%) | 11 (7%) | 147 (93%) | |||
| >10 years | 44 (95.7%) | 2 (4.3%) | 30 (65.2%) | 16 (34.8%) | 7 (15.2%) | 39 (84.8%) | |||
| Province | |||||||||
| Province 1 | 220 (98.2) | 4 (1.8) | - | 98 (43.8) | 126 (56.2) | <0.001 | 27 (12.1) | 197 (87.9) | <0.001 |
| Province 2 | 114 (95.80 | 5 (4.2) | 81 (68.1) | 38 (31.9) | 10 (8.4) | 109 (91.6) | |||
| Bagmati | 172 (98.3) | 3 (1.7) | 118 (67.4) | 57 (32.6) | 41 (23.4) | 134 (76.6) | |||
| Gandaki | 44 (97.8) | 1 (1.7) | 25 (55.6) | 20 (44.4) | 9 (20) | 36 (80) | |||
| Province 5 | 97 (100) | 0 | 65 (67) | 32 (33) | 5 (5.2) | 92 (94.8) | |||
| Karnali | 15 (100) | 0 | 10 (66.7) | 5 (33.3) | 0 | 15 (100) | |||
| Sudur Paschim | 19 (100) | 0 | 15 (78.9) | 4 (21.1) | 0 | 19 (100) | |||
| Level of eye center | |||||||||
| Primary | 23 (92) | 2 (8) | - | 5 (20) | 20 (80) | <0.001 | 9 (36) | 16 (64) | <0.001 |
| Secondary | 62 (100) | 0 | 22 (35.5) | 40 (64.5) | 9 (14.5) | 53 (85.5) | |||
| Tertiary | 470 (98.3) | 8 (1.7) | 312 (65.3) | 166 (34.7) | 37 (7.7) | 441 (85.5) | |||
| Medical college and teaching hospital | 126 (97.7) | 3 (2.3) | 73 (56.6) | 56 (43.4) | 37 (28.7) | 92 (71.3) | |||
| Involvement in COVID-19 case management | |||||||||
| Frontliners | 75 (92.6) | 6 (7.4) | <0.001 | 36 (44.5) | 45 (55.6) | <0.001 | 49 (60.5) | 32 (39.5) | <0.001 |
| Second liners | 103 (98.1) | 2 (1.9) | 50 (47.6) | 55 (52.4) | 19 (18.1) | 86 (81.9) | |||
| None | 503 (99) | 5 (1) | 326 (64.2) | 182 (35.8) | 24 (4.7) | 484 (95.3) | |||
| COVID-19 center | |||||||||
| Yes | 155 (95.1) | 8 (4.9) | 0.01 | 92 (56.4) | 71 (43.6) | 0.385 | 57 (35) | 106 (65) | 0.001 |
| No | 526 (99.1) | 5 (0.9) | 320 (60.3) | 211 (39.7) | 35 (6.6) | 496 (93.4) | |||
Note: n: Frequency; %: Percentage; *Knowledge: Total maximum scores assigned were 10, cut off level of greater than or equal to 7 for good knowledge, and less than 7 for poor knowledge; **Attitude: Total score ranges from 10-50, with an overall higher mean score indicates a positive attitude toward COVID-19; ***Practice: Total maximum scores were 11, cut off level of greater than equal to 7 for good practice, and less than 7 for poor practice.
Table 2: Association of KAP with different factors.
| Variables (N=694) | Knowledge | Attitude | Practice | |||
|---|---|---|---|---|---|---|
| COR (95% CI) | P | COR (95% CI) | P | COR (95% CI) | P | |
| Age | 0.72(0.62-0.82) | <0.001 | 0.92(0.90-0.94) | <0.001 | 1.16(1.10-1.21) | <0.001 |
| Gender | ||||||
| Male | 1.11 (0.36-3.43) | 0.856 | 0.92 (0.67-1.25) | 0.572 | 0.87 (0.55-1.37) | 0.547 |
| Female(ref) | 1 | 1 | 1 | |||
| Designation HCP | ||||||
| Consultant (ref) | 1 | 1 | 1 | |||
| Junior resident | 1.32 (0.082- 21.277) | 0.845 | 1.30 (0.81-2.07) | 0.282 | <0.001 | |
| Optometrist | 1.280 (0.079-20.613) | 0.862 | 0.645 (0.38-1.09) | 0.1 | 1.26 (0.59-2.69) | 0.543 |
| Ophthalmic assistant | 14.87 (1.80-122.51) | 0.012 | 80.61 (28.22-230.25) | <0.001 | 0.95 (0.43-2.12) | 0.901 |
| Others | 10.13 (1.04-99.16) | 0.047 | 65.57 (19.70- 218.24 | <0.001 | 0.82 (0.33-2.06) | 0.823 |
| Job experience | ||||||
| <5 years (ref) | 1 | 1 | 1 | |||
| 5-10 years | 0 | 0.996 | 0.54 (0.37-0.80) | 0.002 | 2.38 (1.23-4.60) | 0.01 |
| >10 years | 1.98 (0.43-9.21) | 0.384 | 0.67 (0.35-1.25) | 0.207 | 0.99 (0.43-2.30) | 0.983 |
| Level of the eye center | ||||||
| Primary | 3.65 (0.58-23.08) | 0.168 | 5.21 (1.84-14.75) | 0.002 | 0.72 (0.29-1.76) | 0.466 |
| Secondary | 0 | 0.997 | 2.37 (1.27-4.43) | 0.007 | 2.37 (1.06-5.29) | 0.035 |
| Tertiary | 0.72 (0.19-2.73 | 0.624 | 0.69 (0.47-1.03) | 0.07 | 4.79 (2.88-7.97) | <0.001 |
| Medical college and teaching hospital (ref) | 1 | 1 | 1 | |||
| Involvement in COVID-19 case management | ||||||
| Front-liners | 8.0 (2.40-27.03) | 0.001 | 2.24 (1.40-3.60) | 0.001 | 0.03 (.02-0.06) | <0.001 |
| Second-liners | 1.95 (0.37-10.21) | 0.427 | 1.97 (1.29-3.01) | 0.002 | 0.22 (0.12-0.43) | <0.001 |
| None(ref) | 1 | 1 | 1 | |||
| COVID-19 center | ||||||
| Yes | 5.43 (1.75-16.84) | 0.003 | 1.21 (0.85-1.72) | 0.293 | 0.13 (0.08-0.21) | <0.001 |
| No (ref) | 1 | 1 | 1 | |||
Note: COR: Crude Odds Ratio; CI: Confidence Interval; HCP: Health Care Personnel
Table 3: Logistic regression analysis for factors associated with knowledge, attitude and practice towards COVID-19.
Binary logistic regression analysis shown in Table 3 revealed that the odds of having poor knowledge and poor attitude decreased by 0.72 (0.62-0.82) and 0.92 (0.90-0.94) times respectively, and the odds of poor practice increased by 1.16 (1.10-1.21) times, with the increment of one year age.
The odds of having poor knowledge among front-liners were 8.0 (2.40-27.03) times more compared to those who were not involved. The odds of poor practice among front-liners and second-liners were 0.03 (0.02-0.06) and 0.22 (0.12-0.43) times less, and the odds of poor attitude among front-liners and second-liners were 2.24 (1.40-3.60) and 1.97 (1.29-3.01) times more compared to those who were not involved.
The odds of having poor practice and poor attitude among participants with experience of 5-10 years was 0.54 (0.37-0.80) times less and 2.38 (1.23-4.60) times more respectively compared to participants with experience of fewer than five years.
Pearson correlation tests revealed a statistically significant moderate positive correlation between knowledge-attitude (r=0.609, p<0.001) and weak positive correlation between knowledge-practice (r=0.300, p<0.001), and attitude-practice (r=0.124, p=0.001) (Table 4).
| Variables | Correlation coefficient (r) | p-value |
|---|---|---|
| Knowledge-attitude | 0.609** | <0.001 |
| Knowledge-practice | 0.300** | <0.001 |
| Attitude-practice | 0.124** | 0.001 |
Note: **: Correlation is significant at the 0.05 level (2-tailed)
Table 4: Correlation between KAP scores.
To the best of our knowledge, this is the first study that has been conducted aimed to determine the level of knowledge, attitude, and practice among ophthalmic health care personnel in Nepal towards the COVID-19 pandemic. Even we assumed this might be the first KAP study that has been done among ophthalmic health care personnel even across the world about the COVID-19 pandemic.
In the present study, 98.1% have good knowledge towards COVID-19 pandemic in Nepal, our findings were consistent to the studies conducted by Alanzi et al. [21], Nepal et al. [22] in Chitwan (Nepal), Saqlain et al. [23] in Pakistan, Zhang et al. [24] in China and Giao Huynh et al. [25] in Vietnam which reported good knowledge among 82.2%, 93.2%, 89%, and 88.4% participants respectively towards COVID-19. In contrast to our findings, a study conducted among nurses reported that 56.5% of respondents had sufficient knowledge regarding the transmission, symptoms, and treatment of COVID-19. This awareness has got more significance in the current scenario when no vaccine has been available till now and various kinds of research are ongoing. So all ophthalmic and non-ophthalmic HCP must be aware of all the updates and should take precautions regarding treatment and prevention of COVID-19 infection.
In this study, 1.9% had poor knowledge regarding COVID-19, this mostly accounted because of the incorrect answer of questions regarding the risk of irreversible maculopathy at the higher doses of chloroquine and hydroxychloroquine for short periods (30.8% incorrect responses) and use of Food Drug Administration (FDA) issued remdesivir, an emergency authorization for the treatment of suspected or laboratory-confirmed COVID-19 (28.8% incorrect responses). The role of chloroquine and hydroxychloroquine in COVID-19 is still under investigation; many trials are going on all over the world as per WHO [26]. Since these drugs can cause ocular toxicity but its use for small duration has not been extensively studied, hence it is controversial. Also, remdesivir [27] being a new promising and emerging drug, found effective against COVID-19. Hence, public health practitioners must be updated on the most promising potential therapeutic drugs that are under investigation. These might be reasons behind the incorrect response to these questions.
Alanzi et al. [21] (70-80%), Nepal et al. [22] (90.93%), Saqlain et al. [23] (60-80%) and Huynh et al. [25] (more than 80%) reported positive attitude among the higher proportion of participants compared to the present study which reported positive attitude among 59.4%. This might be due to good knowledge which is directly proportionate to a positive attitude towards COVID-19. Similarly, in a KAP study related to Ebola virus disease by Iliyasu et al. [28] a negative attitude was related to a lack of knowledge about the use of Personal Protective Equipment (PPE) and the shortage of PPE. At the present context in our country, there is both a lack of knowledge about the use of PPE as well as a shortage of PPE. Other causes might be lack of specific treatment and vaccine for COVID-19, incompetency of central government, lack of overall scientific policies towards combating COVID-19, lack of preparedness of hospitals of our country, lack of adequate testing for COVID-19, lack of work incentives, insurance policy, job security, provision for families of Health care workers, appropriate training, lack of skilled human resources, provision of treatment if tested positive and long and hectic duty hours.
In this study,13.3% had good practice regarding COVID-19 pandemic which was much lower compared to Alanzi et al. [21] (more than 80%), Nepal et al. [22] (83.57%), Saqlain et al. [23] ( 88.7%), and Albarrak et al. [29] (more than 80%). This might be due to a lack of active participation of ophthalmic HCP in the management of COVID-19 at the time of the pandemic.
Nepal et al. [22] and Saqlain et al. [23] reported a significant association between age and good knowledge in agreement to the present study but Giao Huynh et al. [25] failed to find a significant association between knowledge and age. Similar to this study, Nepal et al. [22] reported a significant association between age and positive attitude, and in contrast Saqlain et al. [23] and Albarrak et al. [29] failed to find a significant association.
There was no statistically significant difference in knowledge, attitude, and practice among males and females which was similar to the findings of Saqlain et al. [23] and Giao Huynh et al. [25] and was different from Nepal et al. [22] and Albarrak et al [29].
In this study, there was no significant difference of knowledge about COVID-19 according to their position and designation of ophthalmic HCP in accordance with Saqlain et al. [23] and contrast to Nepal et al. [22], Giao Huynh et al. [25], and Albarrak et al [29]. However, there was a significant difference in attitude as consultants, junior residents and optometrists have a positive attitude whereas ophthalmic assistants and other paramedics have a negative attitude towards COVID-19 but positive attitude were found in doctors, nurses and other paramedics in the study done by Nepal et al. [22], Hyunh et al. [25], and Albarrak et al. [29]. This might be due to the lack of practical awareness regarding COVID-19 infection, which has no fixed guidelines till now.
Regarding practice, junior residents, have overall good practice as compared to other participants which were statistically significant (p<0.001) and as per the study conducted by Saqlain et al. [23] but contradictory with the study by Nepal et al. [22], Hyunh et al. [25], and Albarrak et al. [29] in which the position of HCP is associated with good practice. As ophthalmic residents from various medical colleges and teaching hospitals, besides providing emergency and essential eye care services are also involved in COVID-19 cases management as front-liners. At this time of global health crisis, they are performing their duties very cautiously and with full responsibility as a role model for other paramedics to combat this pandemic.
No significant association was found regarding knowledge among ophthalmic HCP based on their job experience which was in accordance with findings by Nepal et al. [22], Saqlain et al. [23], Albarrak et al. [29] and Hyunh et al. [25]. Job experience was significantly associated with attitude scores in a study by Nepal et al. [22] which is different from the present study and studies by Saqlain et al. [23], Hyunh et al. [25] and Albarrak et al. [29]. There was no association of job experience with practice in our study but, it was found significantly associated in a study done by Nepal et al. [22] (p=0.013) and Saqlain et al. [23] (p=0.012). This might be due to a lack of active involvement in the management of COVID-19 patients.
Similar to present study, Nepal et al. [22] reported a significant correlation of practice scores with knowledge score (r=0.476, p<0.001) and attitude scores (r=0.238, p<0.001); and Saqlain et al. [23] reported significant correlation between knowledge-attitude (r=0.106, p-value=0.030), knowledge-practice (r=0.142, p=0.016), and attitude-practice (r=0.174, p=0.004). This finding inferred that ophthalmic HCP with a positive attitude are more interested in seeking knowledge and then put knowledge into practice. This correlation could also be explained by the Reasoned Action Theory (RAT) which stated, a person’s intention to a specific behavior is a function of their attitude towards that behavior [30].
Binary logistic regression analysis demonstrated the age of HCP to be a significant determinant of good knowledge (COR=0.72, 95% CI=0.62-0.82), positive attitude (COR=0.92, 95% CI=0.90-0.94) and good practice (COR=1.16, 95% CI=1.10-1.21) which similar to Nepal et al. [22] and Saqlain et al [23]. Odds of having positive attitude were higher among HCP with job experience of 5-10 years (OR=1.838, p=0.002), which was as per the study of Nepal et al [22]. Similarly, higher odds of good practice were seen among junior resident (OR=3.846, p<0.001) and HCP with job experience of 5-10 years (OR=0.420, p=0.010) as found in the study by Nepal et al. [22] and Saqlain et al. [23] towards COVID-19 pandemic.
Regression analysis also indicated that experienced health care professionals have good practice in following recommended guideline such as wearing a face mask as it is evident that the use of personal protective equipment might help reduce the spread of the virus in hospitals and protect others from infection [31]. Patients with SARS-CoV-2 infection may be asymptomatic, and shedding seems to be highest in the earliest stage. Thus, asymptomatic carriers of SARS-CoV-2 may confer a particular risk to ophthalmologists during the examination. Specific factors may place ophthalmologists at increased risk of infection during the examination of patients compared with the risk experienced by clinicians in other disciplines [32].
This study highlighted the less explored area where scarce current literature on COVID-19 was available to identify the current status of ophthalmic HCP knowledge, attitude, and practice; an important aspect in a successful response to an epidemic. The questionnaire was developed by using WHO published materials, guidelines, and recommendations from AAO and NOS, and pretesting validation which increase the reliability of the current analysis. High response rate as compared to other similar studies and participation from various eye centres across the country which is representative of ophthalmic HCP. These all constitute the strength of this study. Being an online survey, responses mainly depend upon honesty and partly affected by recall ability and thus may subject to recall bias, potential sample clustering and statistical errors due to multiple significance testing may limit the generalization (external validity) of the results, non-probability sampling method and those who don’t have internet facility, could not get the chance to enroll in the study are its limitation.
Though the majority of ophthalmic HCP have good knowledge, they are lack of sufficient positive attitude and satisfactory level of evidence-based practice towards the COVID-19 pandemic. Hence, this study can be taken as a reference during this COVID-19 era to modify existing guidelines; formulate new policies and guidelines for eye care service; and guide concerned authorities for effective implementation of initiatives like motivation, incentives, insurance policy, job security and provision for families of HCP, to combat this battle against COVID-19. This study has also highlighted the need to uplift our preparedness by the provision of sustained supply of PPE while augmenting awareness on infection prevention and training programs for control measures.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ansari Z, Adhikari S, Chaurasiya BD, Prakash UC, Adhikari B, Khatoon S (2023) Knowledge, Attitude and Practice among Ophthalmic Health Care Personnel (HCP) Towards COVID-19 Pandemic in Nepal: A Web-Based Cross-Sectional Study. J Clin Exp Ophthalmol. 14:937.
Received: 28-Dec-2022, Manuscript No. JCEO-22-19070; Editor assigned: 30-Dec-2022, Pre QC No. JCEO-22-19070 (PQ); Reviewed: 13-Jan-2023, QC No. JCEO-22-19070; Revised: 20-Jan-2023, Manuscript No. JCEO-22-19070 (R); Published: 30-Jan-2023 , DOI: 10.35248/2155-9570.23.14.937
Copyright: © 2023 Ansari Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.