Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Case Report - (2019)Volume 7, Issue 2
In patients where anticoagulation therapy is contraindicated, Inferior Vena Cava (IVC) filters are used as an option to prevent Pulmonary Embolism (PE). There are many classifications of Vena Cava filters the two main groups are; those intended for permanent implantation and the other temporary (which are to be retrieved at a later date). Permanent IVC filters are not designed to be removed, unless unexpected clinical circumstances arise. We describe a complex case of retrieval of a permanent IVC filter, though well documented; it is the first of its kind to be recorded in the Caribbean.
Pulmonary Embolism; Anticoagulation therapy; Inferior Vena Cava (IVC)
Pulmonary Embolism (PE) is a potentially life-threatening condition where an embolus after being formed in the deep veins of the legs or pelvis, travels to the lungs where it may occlude one or more of the pulmonary arteries. PE is therefore regarded as one of the manifestations of the condition venous thromboembolism, which is the third most common cardiovascular disorder in industrialized countries [1] including the United States [2,3]. The common treatment, once a diagnosis is confirmed, is to administer anticoagulants to resolve the clot. In patients where anticoagulation therapy is contraindicated Inferior Vena Cava (IVC) filters are used as an option to prevent PE.
However, the indications for placement of IVC filters still remain, somewhat controversial, where different groups having varying guidelines creating a “shades of grey area” for implantation. These devices however, prove to be effective in preventing fatal or massive PE in patients with deep venous thrombosis who have contraindications to systemic anticoagulation. There are many classifications of Vena Cava filters the two main groups are; those intended for permanent implantation and the other temporary (which are to be retrieved at a later date) [4]. These filters are known to come with their own set of risks, namely deep venous thrombosis, filter migration, filter-fracture, caval thrombosis [5] and filter erosion through the caval wall [6].
Permanent IVC filters were not designed to be removed. However, the US Food and Drug Administration in 2010 and 2014 have since issued safety communication encouraging the removal of optional IVC filters “as soon as protection from pulmonary embolism is no longer needed” [6-8]. In the developing world setting and certainly, in Trinidad and Tobago due to availability limitations, especially in the public hospital setting, patients do not always have both options available and sometimes the indications are for the use of a permanent IVC filter. We describe a complex case of retrieval of a permanent IVC filter, the first of its kind to be recorded in the Caribbean.
A 63 year old female patient, presented to our clinic with suspected Right DVT. History of two known episodes of Lower Limb Deep Vein Thrombosis (DVT) first occurring on the Left, nine years prior and then on the Right with near fatal PE, which indicated the need for a permanent IVC filter which was placed at a public institution where temporary filters were not available at the time. An abdominal X-ray showed the IVC filter in situ. Bilateral Venous Duplex Ultrasound showed no evidence of active DVT and no longer at risk for PE. Therefore, by the patient’s requests for its removal, given the inherent risks of leaving in the filter and the US Food and Drug Administration recommendation.
Two access sites were prepared- the Right Femoral and Right Jugular regions. Using Seldinger technique, two percutaneous accesses were obtained from the Right Femoral Vein and the Right Jugular vein. An injection of contrast via the Right Femoral sheath was then taken to assess the position of the filter and to ensure no perforation of the caval wall or other abnormalities or complications occurred (Figure 1).
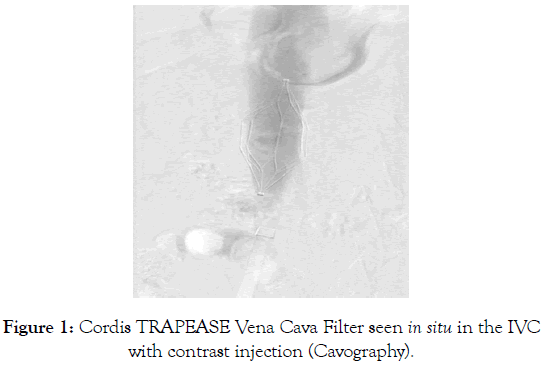
Figure 1: Cordis TRAPEASE Vena Cava Filter seen in situ in the IVC with contrast injection (Cavography).
A Cook 16F, 35 cm long, Introducer sheath was placed into each of the veins. A Cook 8 Fr × 70 cm Flexor Check-Flo Introducer, was advanced with a Cook 5 Fr VCF catheter loaded upon a Terumo Hydrophilic guide wire. This system was then used to pass the guide wire through the caudal struts of the IVC filter (Figure 2).
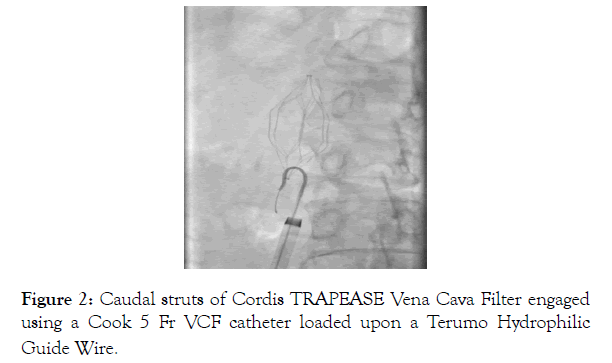
Figure 2: Caudal struts of Cordis TRAPEASE Vena Cava Filter engaged using a Cook 5 Fr VCF catheter loaded upon a Terumo Hydrophilic Guide Wire.
A Merit Medical EN Snare® Endovascular Snare System was then used to capture the hydrophilic guide wire, forming a loop through the caudal struts (Figure 3). The snared end of the hydrophilic guide wire was retrieved through the 8 Fr Introducer sheath and haemostatic valve of the femoral vein sheath (Figure 3).
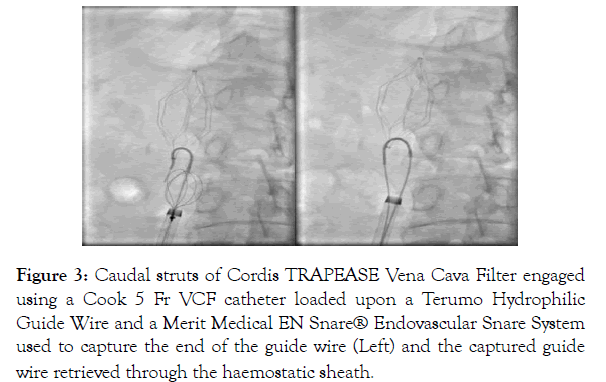
Figure 3: Caudal struts of Cordis TRAPEASE Vena Cava Filter engaged using a Cook 5 Fr VCF catheter loaded upon a Terumo Hydrophilic Guide Wire and a Merit Medical EN Snare® Endovascular Snare System used to capture the end of the guide wire (Left) and the captured guide wire retrieved through the haemostatic sheath.
A Cook 5 Fr VCF catheter loaded upon a Terumo Hydrophilic guide wire which was then passed through the cranial struts of the IVC filter as was done at the distal end. The Merit Medical EN Snare® Endovascular Snare System was again used to capture the hydrophilic guide wire, forming a loop through the cranial struts. The snared end of the hydrophilic guide wire was retrieved through the hemostatic valve of the jugular vein sheath (Figure 4).
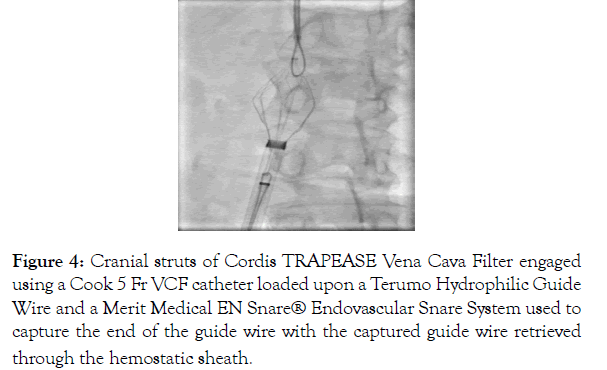
Figure 4: Cranial struts of Cordis TRAPEASE Vena Cava Filter engaged using a Cook 5 Fr VCF catheter loaded upon a Terumo Hydrophilic Guide Wire and a Merit Medical EN Snare® Endovascular Snare System used to capture the end of the guide wire with the captured guide wire retrieved through the hemostatic sheath.
With both ends of the IVC filter snared and guide wires through the hemostatic sheaths, continuous tension was applied simultaneously to the external guide wires. Both 16 Fr sheaths were then advanced to further collapse the IVC filter and dislodge the barbs form being imbedded in the IVC wall. Although the filter collapsed easily, the tissue that encapsulated the barbs of the filter, due to neo-intimal hyperplasia initially prevented it from being dislodged from the caval wall (Figure 4).
After numerous attempts at collapsing the filter without success, we employed a back and forth flossing like motion to dislodge the struts. This technique worked and the struts finally came free from the caval wall and the filter collapsed and successfully retrieved into the 16 Fr sheath in the Right Jugular vein and then removed from the body (Figure 5).
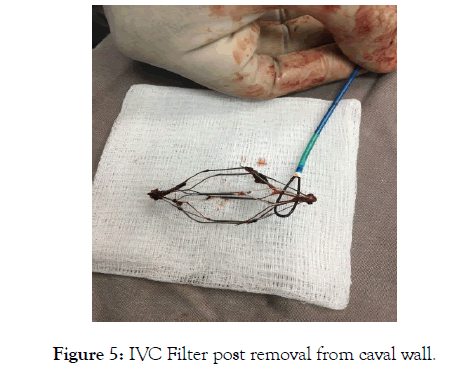
Figure 5: IVC Filter post removal from caval wall.
A post removal control venogram showed a large thrombus which occluded the IVC and was successfully aspirated. Final venogram showed continuous flow without extravasation of contrast indicating an intact vessel wall and successful Permanent IVC Filter removal.
The Cordis TRAPEASE Permanent Vena Cava Filter was in situ for approximately 2 years. This dwell time posed an increased level of complexity as one of the difficulties encountered in removing permanent IVC filters implanted for 6 months is the extensive neointimal hyperplasia that develops along the struts [4]. Taking the following into consideration
(i) The patient was no longer at risk for PE,
(ii) FDA encouraging the removal of optional IVC filters as soon as protection from PE is no longer needed [6-8],
(iii) The patient requested its removal,
(iv) In carefully selected patients, percutaneous removal of permanent IVC filters can be performed safely despite prolonged filter dwell times [9], a decision was made to attempt the removal of the Cordis TRAPEASE Permanent Vena Cava Filter.
The retrieval technique employed for the Cordis TRAPEASE Permanent Vena Cava Filter is directly related to an understanding of its construction. According to the Cordis catalogue this filter is made of Nitinol (Nickle and Titanium metal alloy), closed cage design with long side struts to allow for self-centering and opposing cranial and caudal fixation barbs to reduce filter migration (Figure 6). In our case it was these fixation barbs that posed the greatest challenge. In an effort to ensure non migration the barbs are intended to be lodged into the caval wall. Due to the extended dwell time (possibly over 2 years), it facilitated the progression of neo-intimal hyperplasia which contributed to it being immovable and also almost impossible to be retrieved.
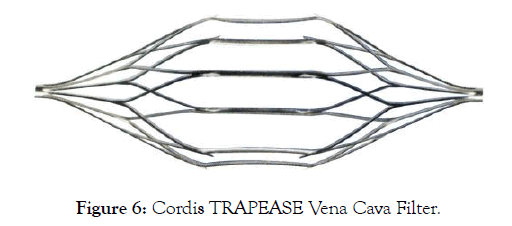
Figure 6: Cordis TRAPEASE Vena Cava Filter.
The back and forth pulling and pushing motion (similar to flossing) allowed for the dislodging of the barbs by forming or creating ‘tracks’ in the intima and loosening of the neo-intimal hyperplasia formed. From the design, the cranial pull would dislodge the cranial barbs and caudal barbs would be dislodged by the caudal pull. Once dislodged it was possible to collapse the permanent IVC filter and retrieve it through the sheath without complication. Other methods used to remove Permanent IVC filters are similar to what was described up to where the sheaths were advanced to collapse the filter. If the filter could not be freed, clamshell forceps were inserted in tandem with an in situ snare or endo-bronchial forceps and used to dissect neo-intimal tissue away from the filter where the struts contact the wall [8].
This case represents the first successful Permanent IVC filter retrieval using the Kissing Sheath technique in Trinidad and Tobago. This case proves that, in carefully selected patients, percutaneous removal of permanent IVC filters can be performed safely despite prolonged filter dwell times. It signals new opportunities for patients with Permanent IVC filters who are no longer at risk for PE, according to the advice by the FDA, to have these filters removed. This spared the possible complications of leaving the IVC filter such as deep venous thrombosis, filter migration, filterfracture, caval thrombosis and filter erosion through the caval wall.
Special thanks to David Richards (RR) for his help with venogram images.
Citation: Mor R, Maharaj D, Calderas C, Rampersad R (2019) Kissing Sheath Technique for Permanent Inferior Vena Cava. Angiol Open Access 7:228
Received: 13-May-2019 Accepted: 12-Jun-2019 Published: 21-Jun-2019 , DOI: 10.35248/2329-9495.19.7.228
Copyright: © 2019 Mor R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.