Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 3
Aim: To assess the Intra Ocular Pressure (IOP) profile in infants at the university teaching hospital of Yaoundé.
Materials and methods: We carried out a cross-sectional analytical study from December 2019 to April 2020 using an I-care rebound tonometer. All infants aged between 1 month and 24 months were included in the study
Results: A total of 992 eyes belonging to 496 infants of mean age 8.5 ± 5.9 months were examined. The mean gestational age was 39.5 ± 1.5 amenorrhea weeks, with a mean birth weight of 3311 ± 618 g. Of the 496 infants, 3% (n=15) had a family history of glaucoma and 17% (n=87) were receiving vitamin D supplementation. The mean intraocular pressure of the infants was 10.24 mmHg ± 3.7 in the right eye and 10.43 mmHg ± 3.9 in the left eye. It was found that age, term of pregnancy, and familial glaucoma all influenced the increase in IOP.
Conclusion: The mean IOP of Cameroonian infants at CHUY is 10.34 mmHg ± 3.7. Age, pregnancy duration, and family history of glaucoma have an independent association with IOP
Intraocular pressure; Infant; I-care rebound tonometer
Intra Ocular Pressure (IOP) remains an important tool in the diagnosis, treatment, and monitoring of glaucoma [1]. IOP measurement in children is challenging due to issues with cooperation, measurement technique, and the instruments used. Only the pulse tonometer allows non-contact measurement; however, their values are often overestimated, especially if the child blinks. All other techniques that require contact (Goldmann, Perkins, Tono-Pen) are also challenging when handling young children [2]. Several studies in newborn children have revealed variability in IOP figures based on tonometer type. Victoria et al, in Nigeria [3] reported a mean IOP of 11.93 ± 1.80 mmHg, while Radtke et al. [4], using the Perkins tonometer, found a mean of IOP of 11.4 ± 2.4 mmHg. Kim et al. [5] in Korea and Reddy et al. [6] in Malaysia used Tono-Pen and reported mean IOPs of 13 ± 3.4 mmHg and 15.99 ± 2.79 mmHg, respectively. Meanwhile, a mean IOP value of 9.59 ± 2.3 mmHg was found by Pensiero et al.in Italy, who used a non-contact tonometer [7]. The aim of the present study is to contribute to the determination of the normal IOP range in African infants.
This was a cross-sectional analytical study conducted between December 2019 and April 2020 in the Vaccination Department of the Yaoundé University Hospital Centre (CHUY). We included all infants aged between 1 month and 24 months who had been admitted into vaccination service of the Yaoundé University Teaching Hospital. Certain exclusion criteria were applied; three infants were excluded due to clinical signs of congenital glaucoma, such as lacrimation, photophobia, blepharospasm, corneal oedema, megalocornea, and buphthalmia. Any infant for whom the examination could not be performed due to irritability and/ or unsuccessful IOP measurement after three separate attempts were also excluded.
This study was approved by the Institutional Review Board of the Faculty of Medicine and Biomedical Sciences (FMSB) of the University of Yaoundé, and written informed consent was obtained from the parents or legal guardians of the infants
Each participant underwent an ophthalmological examination with a torch. Regarding the position, each child was either standing or sitting on their mother’s laps, and their head was upright. For each child, a new sterile disposable probe was inserted into the I-care tonometer. IOP was measured without contact anesthesia using the I-care IC100 rebound tonometer after gently opening the eyelids without pressure on the eyeball (Figure 1). Three measurements were taken in each eye, and an average value was considered for the analysis.
Figure 1: Measurement of intraocular pressure in a 2-month-old infant using the I care rebound tonometer.
The parameters analyzed included age, sex, perinatal history (birth weight and age at delivery), family history of glaucoma, vitamin D supplementation, and IOP. IOP measurement was performed by the same investigator between 10 am and 2 pm.
Statistical analysis
The data were analyzed using SPSS version 23.0. The quantitative variables were expressed as mean and Standard Deviation (SD). Furthermore, Pearson’s correlation coefficient was used to analyze the association between the IOP parameters and the children’s age, sex, birth weight, term of pregnancy, and family history of glaucoma. For all the tests, P values<0.05 were considered to be statistically significant.
A total of 496 infants, 258 boys (52%) and 238 girls (48%) with ages ranging from 1 month to 24 months were included in this study Table 1; the mean age was 8.5 ± 5.9 months. Most of the babies had a birth weight ranging from 2500 g to 3400 g (54.4%). Of the 496 infants, 88.7% were born after 37 weeks of pregnancy in Table 2 and 15 (3%) had a family history of glaucoma. Vitamin D supplementation was found in 87 (17%) cases. The IOP for the right and left eyes ranged from 5 to 21 mmHg (Table 3). There was no significant difference between the mean IOP for the right (10.24 ± 3.7 mmHg) and left eyes (10.43 ± 3.9 mmHg) (P=0,061).
| Variables | Number (n) | Percentages (%) |
|---|---|---|
| Age (Month) | ||
| [1-6] | 158 | 31,9 |
| [6-12] | 200 | 40,3 |
| [12-18] | 97 | 19,6 |
| [18-24] | 41 | 8,3 |
| Total | 496 | 100 |
Table 1: Age distribution of the study population.
| Variables | Infants (n) | Percentage% |
|---|---|---|
| Birth weight (g) | ||
| <2500 | 35 | 7,1 |
| [2500-3500] | 270 | 54,4 |
| [3500-4000] | 124 | 25 |
| ≥ 4000 | 67 | 13,5 |
| Mean ± SD | 3311 ± 618 | |
| Gestational age (AW) | ||
| < 37 | 38 | 7,7 |
| [37-42] | 440 | 88,7 |
| ≥ 42 | 18 | 3,6 |
| Mean ± SD | 39,5 ± 1,5 | |
Table 2: Distribution of the study population according to perinatal history.
| Variables | Total | Right eye | Left eye | p-value |
|---|---|---|---|---|
| IOP | ||||
| Mean ± SD | 10,34 ± 3,8 | 10,24 ± 3,7 | 10,43 ± 3,9 | 0,061 |
| Min–Max | May-21 | 5-21 | May-21 |
Table 3: IOP distribution in both eyes.
The mean IOP was 10.39 ± 3.7 mmHg in boys and 10.28 ± 3.9 mmHg in girls; there was no significant difference between these values (P=0.66) (Table 4). For infants aged 1-5 months, the mean IOP was 9.3 ± 3.7 mmHg; for those aged 6-11 months, it was 10.3 ± 3.7 mmHg; for those aged 11-17 months, it was 10.4 ± 3.1 mmHg; and for those aged 18-24 months, it was 13.7 ± 4 mmHg (Table 5). The correlational analysis yielded the following results:
| Variables | Total | Male | Female | p-value |
|---|---|---|---|---|
| Mean IOP ± SD | 10,34 ± 3,8 | 10,39 ± 3,7 | 10,28 ± 3,9 | 0,667 |
| Min- Max | May-21 | 5-21 | May-20 |
Table 4: Mean IOP distribution according to gender.
| Variables | Age (Month) | P-value | |||
|---|---|---|---|---|---|
| [1-6] | [6-12] | [12-18] | [18-24] | ||
| Mean IOP ± SD | 9,35 ± 3,7 | 10,36 ± 3,7 | 10,47 ± 3,1 | 13,7 ± 4 | 10-4 |
| Min- Max | May-21 | Jun-20 | 5- 18 | Jul-20 | |
Table 5: Mean IOP distribution according to age groups.
-IOP increased significantly with age (r=0.312; P=0-4) (Figure 2).
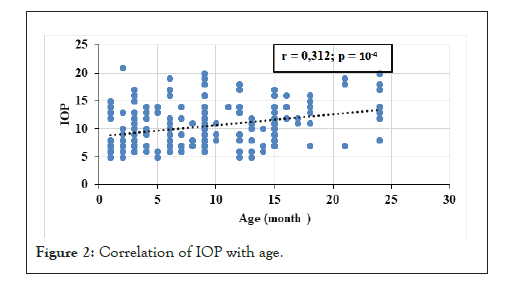
Figure 2: Correlation of IOP with age.
-Infants with a birth weight of less than 2500 g had an elevated mean IOP as compared to those with a birth weight of 2500-4000 g.
IOP increased in infants with a birth weight above 4000 g (P=0.008) (Table 6).
| Variables | Birth weight | P- value | |||
|---|---|---|---|---|---|
| <2500 | [2500-3500] | [3500-4000] | ≥ 4000 | ||
| IOP | |||||
| Mean ± SD | 11.09 ± 4.6 | 9.97 ± 3.6 | 10.65 ± 4.1 | 11.8 ± 3.3 | 0.008 |
| Min-Max | Jun-21 | 5-20 | 5-20 | Jun-17 | |
Table 6: Distribution of mean IOP according to birth weight.
Birth weight had no significant influence on IOP (correlation coefficient r=0.031, P=0.32). Infants with a gestational age of 37 to 41 weeks had a mean IOP of 10.43 ± 3.9 mmHg, whereas infants born before 37 gestational weeks had a mean IOP of 9.2 ± 2.6 mmHg. Infants born after 42 gestational weeks had a mean IOP of 10.33 ± 3.1 mmHg (P=0.025). The correlation coefficient (r) of IOP with gestational age was 0.057 (P=0.073), indicating there was no significant correlation between IOP and gestational age. Infants on vitamin D supplementation had a mean IOP of 9.22 ± 3.9 mmHg, while those not on vitamin D supplementation had a mean IOP of 10.57 ± 3.7 mmHg; this difference was statistically significant (P=0.001). Children with a family history of glaucoma had a mean IOP of 13.87 mmHg ± 5.3, whereas children without a family history of glaucoma had a mean IOP of 10.23 ± 3.7 mmHg (P=0.001). A multivariate analysis of the variables associated with IOP showed that age, term of pregnancy, and family history of glaucoma were independent factors significantly associated with IOP (Table 7).
| Variables | Coefficient beta | 95% CI of Beta | Adjusted P-value |
|---|---|---|---|
| Age (month) | 0.19 | 0.1-0.2 | < 0.001 |
| Gender | -0.225 | -0.7-0.2 | 0.324 |
| Weight birth (g) | -0.019 | -0.02-0.001 | 0.582 |
| Gestational age (AW) | 0.283 | 0.1-0.457 | 0.002 |
| family history of glaucoma | -2.9 | -4.3-(-1.7) | < 0.001 |
| vitamin D supplementation | 0.023 | (-0.6)-0.7 | 0.945 |
Table 7: Multivariate analysis (Multiple Linear Regression) of factors associated with IOP.
This study aimed to determine the IOP profile of healthy Cameroonian infants using the I-care rebound tonometer; this tonometer was chosen as it can be used without topical or general anesthesia and without blepharostat. The mean age of the infants was 8.5 ± 5.9 months; this may be because we conducted our study in an immunization service, where the expanded immunization program covers up to 15 months of age and consists of vaccines administered free of charge. In contrast, Shihota et al. in India, found a mean age of 6.68 years [8].
The mean IOP values found in our study (10.24 ± 3.7 mmHg for the right eye and 10.43 ± 3.9 mmHg for the left eye) were lower than those reported by other authors. For instance, Victoria et al., in Nigeria, reported IOPs of 11.93 ± 1.80 mmHg for the right eye and 11.84 ± 1.77 mmHg for the left eye in children born at term [3]. Radtke et al. [4], found a mean IOP of 11.4 ±2.4 mmHg in newborns. In Korea, Kim et al. [5] studied newborns on the second day of life and found a mean value of 13 ± 3.4 mmHg. Reddy et al. in Malaysia [6], reported a mean IOP of 15.99 ± 2.79 mmHg using Tono-Pen in neonates. Pensiero et al. [7] in Italy found a mean low IOP of 9.59 ± 2.3 mmHg among children at birth. Low IOP values were also reported by other authors [8,9]. This variability may exist because our study was conducted on infants, while the other studies were conducted on neonates. Other factors contributing to the variability may include the method of examination (under general anesthesia), variation in the instruments used for IOP measurement, the use of blepharostat, the time of measurement, and, possibly, ethnicity.
We found an increase in IOP with age (r=0.312; P=10-4). A similar variation was also reported by Bresson et al. [2]. However, we found no significant influence of gender, birth weight, or gestational age on IOP. Victoria et al. has also found a nonsignificant relationship of gender, birth weight and gestational age on IOP [3,6-10]. In contrast to our results, Ng et al. [11] in Hong Kong found a strong negative association between IOP and birth weight in a longitudinal study of pre-term infants. Vitamin D supplementation is routinely prescribed for newborns up to the age of 2 years in Cameroon. Infants taking vitamin D supplements at the time of the study had lower IOP values than those not taking it. Kutuzova et al. [12], in the United States, conducted a study of mice that showed vitamin D decreased the expression of several genes related to IOP regulation; they also found that vitamin D applied topically to the eye reduced IOP in non-human primates. This may suggest that vitamin D plays a role in the regulation of IOP in humans as well. However, Krefting et al. [13], who carried out a case-control study and randomized controlled trial in Norway with intravenous administration, did not report that vitamin D played a role in IOP regulation. These different results may be explained by the different routes of vitamin D administration in the three studies. Infants with a family history of glaucoma exhibited elevated IOP (P=0.001). This finding corroborates those of studies conducted by Wu et al. and Chang et al. [14-16] in Barbados, India, and Maryland, United States, respectively.
Similarly, an Australian observational study by Le et al. which involved 3271 subjects, showed that the relative risk of developing glaucoma when one had a family history of it was 2.1/95% CI=1.03-4.2. The mean intraocular pressure of infants is 10.34 ± 3.8 mmHg. Age, gestational age and family history of glaucoma significantly increase IOP. Gender and birth weight had no influence on IOP. This study provides useful normative data on IOP in Cameroonian’s infants that can be considered for the assessment of glaucoma.
The authors thank the parent of the child patient for allowing the case to be published.
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
[CrossRef] [Pubmed] [Google Scholar].
Citation: Nanfack CN, Kamga BG, Kalla C, Bilong Y, Noche CD, Kagmeni G (2022) Intraocular Pressure Profile in Infants at the University Teaching Hospital of Yaounde. J Clin Exp Ophthalmol. 13:913
Received: 26-Jan-2022, Manuscript No. JCEO-22-15651; Editor assigned: 28-Jan-2022, Pre QC No. JCEO-22-15651 (PQ); Reviewed: 11-Feb-2022, QC No. JCEO-22-15651; Revised: 16-Feb-2022, Manuscript No. JCEO-22-15651 (R); Published: 23-Feb-2022 , DOI: 10.35248/2155-9570.22.13.913
Copyright: © 2022 Nanfack CN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.