Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2023)Volume 14, Issue 5
Aim: Attention deficits are revealed in amblyopic vision. It has been reported that selective visual attention is allocated preferentially toward the non-amblyopic fellow eye in adults with amblyopia. In this study, we examined whether training with dichoptic attention tasks, which is expected to improve selective visual attention to the amblyopic eye, improves contrast sensitivity in adults with amblyopia.
Methods: We used training stimuli, which included tasks that required significant attentional efforts from the amblyopic eye. Through a mirror stereoscope, participants were instructed to quickly search and count highly visible targets presented in the amblyopic eye, while simultaneously being presented with distractors in the fellow eye. Thirteen adults with amblyopia (six anisometropic and seven strabismic) between 22 and 66 years old participated in the study. Trainings were about two visits per week and two hours per visit for two months. Contrast response function and contrast sensitivity (1/contrast threshold, defined as the contrast at 75% correct orientation responses) in the amblyopic eye were measured with psychophysical procedures and compared before and after the training.
Results: Contrast response function and contrast sensitivity in the amblyopic eye improved for 10 of 12 participants after training (one strabismic amblyope withdrawn from the study). The group average of contrast sensitivity after the training was significantly higher than that before the training (p<0.01). Contrast sensitivity improved an average of 31.73% across all participants, which was correlated with the improvement of selective visual attention to the amblyopic eye (rho=0.55, p=0.04). There was no significant difference in contrast sensitivity improvement between subgroups of anisometropic and strabismic amblyopia (p=0.1495).
Conclusion: Amblyopic training with a dichoptic approach, incorporating attention demand tasks in the amblyopic eye, might be an effective way of treating amblyopia.
Amblyopia; Strabismus; Contrast sensitivity; Selective visual attention; Neural plasticity
Amblyopia is a developmental disorder of spatial vision and affects about 3% of the population during early childhood [1]. Amblyopia is commonly caused by strabismus (misaligned eyes), anisometropia (unequal refractive error in the two eyes), or a mixture of strabismus and anisometropia, and is clinically defined as visual acuity loss without abnormal findings in the eye. However, various perceptual deficits, including deficits in contrast sensitivity, stereoacuity, global motion sensitivity, illusory contour perception and contour integration, are also found in individuals with amblyopia [2-14]. In addition to perceptual deficits, there is converging evidence suggesting attention deficits in individuals with amblyopia. For example, several behavioral studies revealed deficits in performing attention tasks with the amblyopic eye. These tasks include object enumeration, object tracking, attentional blink and decision making [15-22]. Importantly, reported that dichoptic attentive motion tracking is biased to the fellow eye in strabismic amblyopes, indicating selective visual attention is allocated preferentially toward the non-amblyopic fellow eye [23]. Using Electroencephalography (EEG) Sourced Imaging (ESI), our previous work revealed degraded attentional modulation in the primary visual cortex (V1) and extra-striate cortex to input from the amblyopic eye compared to input from the fellow eye in strabismic amblyopes, consistent with attention deficits reported from behavioral studies [24]. These studies point to the view that improving selective visual attention to the amblyopic eye might be an important factor in amblyopic training.
The standard clinical treatment for amblyopia consists of patching the fellow eye to promote the use of the amblyopic eye. This treatment benefits most amblyopic children and teenagers, but more so in younger children than in older children [25]. Currently, there is no standardized clinical treatment available for adults with amblyopia. However, recent decades of research with perceptual learning (repeated practice on a demanding visual task, also referred to as training in the current study) in adults with amblyopia have shown improvements in various visual functions, including visual acuity and stereoacuity, position acuity and contrast sensitivity [26-31]. Using diverse methodologies, almost all studies with behavioral training have shown improvements in visual acuity and other visual functions in amblyopia over the past few decades, based on a meta-analysis that were performed on 24 amblyopic training studies in adults [32]. This meta-analysis also speculated that attention might be one of important factors for the success of amblyopic training.
How an attention factor relates to visual training has not been systematically studied. For example, the training tasks that are used in many previous studies included low-level visual features (e.g., discrimination of contrast orientation or spatial frequency, etc.), which might have been confounding variables with attention factors to the training results. The attention factors were either not evaluated or correlated to the training results. To evaluate the role of an attention factor in amblyopic training, we used training tasks in adults with amblyopia that required significant attentional efforts from the amblyopic eye but avoided low-level visual features under a dichoptic approach, and the results are reported in series. In our first report, we demonstrated how improving selective visual attention to the amblyopic eye reduced interocular suppression in adults with amblyopia. In this study, we reported how training with dichoptic attention tasks improved contrast sensitivity in adults with amblyopia.
Participants
Six anisometropic amblyopes and seven strabismic amblyopes between 22 and 66 years of age (five males) participated in this study. The participant S7 withdrew from the study with no post training contrast sensitivity measurement. Therefore, we did not include this participant in the data analysis. An advertisement of the study was used to recruit participants in the San Francisco Bay Area. All participants were given eye examinations by a pediatric ophthalmologist and were refracted under a non-cycloplegic condition. Amblyopia was defined as anisometropic amblyopia (≥ 1 D of refractive error interocular difference; referred to as Aniso), strabismic amblyopia, or mixed of both. We referred to strabismic or mixed amblyopia as Strab in this study. Visual acuity was measured with a logMAR chart (Bailey-Lovie) before training with best optical correction. Eligible participants had best-corrected visual acuity in the amblyopic eye of 0.20 logMAR (20/30) or worse and in the fellow eye of 0.00 logMAR (20/20) or better. Stereoacuity was evaluated with the random-dot stereo butterfly card (Stereo Optical, Chicago, IL, USA). General demographic and clinical information adapted from our first report are provided in Table 1. Note that although both S2 and S6 had minor exotropia, S2 had constant vertical deviation, and S6 had deviation that was residual strabismus after strabismic surgery. Individuals with other eye diseases (e.g., cataract, glaucoma, age-related macular degeneration, etc.), latent or manifest nystagmus and other types of amblyopia (e.g., secondary to congenital cataract) were excluded in this study. The study protocol was approved by the Institutional Review Board at the Smith-Kettlewell Eye Research Institute and was in accordance with the Declaration of Helsinki. Participants’ written and informed consent was gathered before commencing the study (Table 1).
| Participant | Diagnosis | Age | Gender | Visual Acuity (log MAR) | Refractive Errors | Stereoacuity | Deviation | History | ||
|---|---|---|---|---|---|---|---|---|---|---|
| ID | Fellow eye | Amblyopic eye | Fellow eye | Amblyopic eye | ||||||
| A1 | A | 49 | f | 0 | 0.24 | 0.50+0.50*90 | -1.50+2.25 × 130 | 70 | Ortho | Patching done |
| A2 | A | 27 | f | 0.04 | 0.46 | 38 | 42 | 200 | Ortho | No patching |
| A3 | A | 50 | f | -0.2 | 0.38 | 14 | 79.5 | 200 | Ortho | Patching done |
| A4 | A | 51 | f | 0 | 0.5 | -0.25 | 48 | 200 | Ortho | Patching done |
| A5* | A | 22 | m | -0.09 | 0.3 | 53.75 | 58.25 | 200 | Ortho | Patching done |
| A6* | A | 52 | f | 0.04 | 0.5 | 8.25 | 115 | 100 | Ortho | Patching done |
| S1 | S and A | 59 | m | -0.04 | 0.7 | 0.75 | 17.75 | n/a | XT 14, L/R 4 | Surgery and patching |
| S2 | S and A | 62 | m | 0 | 0.7 | 120 | 200 | n/a | XT 4, R/L 2 | Patching done |
| S3 | S and A | 40 | f | 0 | 0.518 | 343.25 | Plano | n/a | XT 8 | Surgery and patching |
| S4 | S and A | 28 | m | -0.09 | 0.62 | Plano | 46 | 400 | ET 16 | No patching |
| S5* | S | 38 | m | -0.09 | 0.3 | -1.5 | -1.5 | n/a | XT 12, R/L 4 | Patching done |
| S6* | S and A | 66 | F | -0.02 | 0.46 | 131.25 | 132.2222222 | n/a | XT 8 | Surgery and patching |
| S7# | S and A | 55 | f | 0 | 0.7 | -2.25+1.25 × 90 | -4.75+1.00 × 110 | n/a | XT 20 | No patching |
Note: A: Anisometropic amblyopia; S: Strabismic amblyopia; S and A: Mixed with strabismus and anisometropia; n/a: Non-measurable stereoacuity; XT: Exotropia; ET: Esotropia; L/R: Left eye hypertropia; R/L: Right eye hypertropia; *: Participant did not complete 16 visits; #: Withdrawal from the study
Table 1: Demographic and clinical characteristics of participants.
Stimuli and display
Two Sony Trinitron Multiscan G400 CRT monitors, each with a frame rate of 85 Hz, were used to present the stimuli at a viewing distance of 85 cm for training and contrast sensitivity measures. The stimuli were programmed in MATLAB (Mathworks, Natick, MA) with the psychophysics toolbox. The detailed description of the training stimuli can also be found in elsewhere [33,34]. In brief, our goal was to evaluate the role of attention in amblyopic training (e.g., whether improving selective visual attention to the amblyopic eye by training without spatial frequency-based or contrast sensitivity-based tasks improves visual functions). Therefore, we wanted to exclude the typical contrast sensitivity-based tasks that had been used in previous training studies. Our stimuli included highly visible Gabors (above 25% contrast with 2 cpd of low spatial frequency, 0.7° in size), allowing for them to be seen by the amblyopic eye with poor visual acuity as shown in Figures 1A and 1B. The stimuli consisted of three key factors (searching, counting and cueing targets) that implement selective visual attention to the trained eye. The tasks involved quickly searching and counting targets (vertical Gabors) presented in the trained eye while simultaneously being presented with distractors (horizontal Gabors) in the untrained eye. This was done under dichoptic viewing through a mirror stereoscope, in which both the horizontal and vertical deviations in strabismic amblyopes were adjusted by mirrors to align the nonius lines under the best optical correction. A 500 ms valid visual cue preceded each trial was used to guide attention to the trained eye, indicating which eye would get the targets. Presenting targets and distractors in different eyes was done to provide an experimental environment to engage the use of binocular vision with attention competition [35]. Targets were presented to the amblyopic eye in 90% of trials and to the fellow eye in 10% of trials with a random order within a block, so that the participants were not aware which eye saw the targets. Searching and counting features require rapid shifts in attention, and are therefore considered as high-attention demand tasks [36-38]. The visual field was 21° x 18° with white noise in the periphery, being large enough to encourage peripheral fusion. The central target area subtended 5.6° in diameter (Figures 1A and 1B).
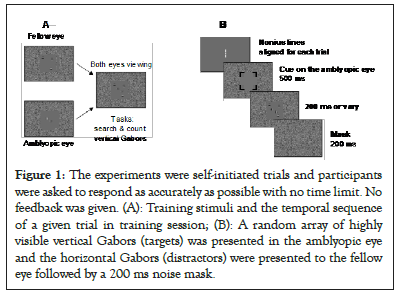
Figure 1: The experiments were self-initiated trials and participants were asked to respond as accurately as possible with no time limit. No feedback was given. (A): Training stimuli and the temporal sequence of a given trial in training session; (B): A random array of highly visible vertical Gabors (targets) was presented in the amblyopic eye and the horizontal Gabors (distractors) were presented to the fellow eye followed by a 200 ms noise mask.
Training protocol
The detailed training protocol can be found in our first report. In brief, the participants were requested to have about two visits per week and two hours per visit for two months (16 visits, 32 hours training, ~ 7000 trials of repetitive practice), because after 7000 trials, observers have shown that there is no further improvement [39]. Contrast response function and contrast sensitivity in the amblyopic eye were measured and compared before and after training (Figures 2 and 3).
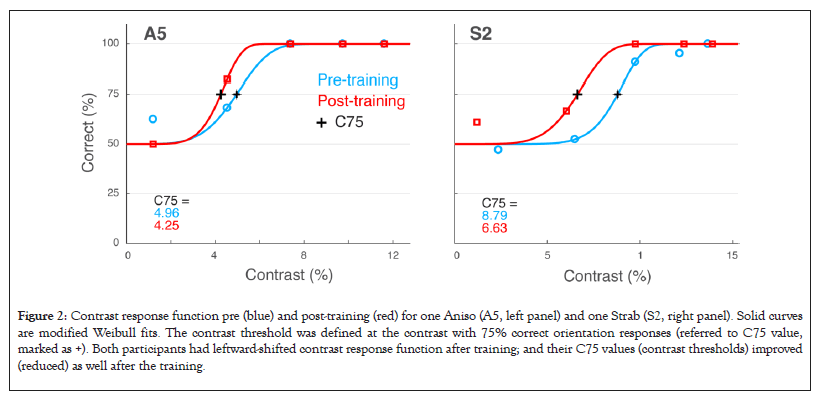
Figure 2: Contrast response function pre (blue) and post-training (red) for one Aniso (A5, left panel) and one Strab (S2, right panel). Solid curves are modified Weibull fits. The contrast threshold was defined at the contrast with 75% correct orientation responses (referred to C75 value, marked as +). Both participants had leftward-shifted contrast response function after training; and their C75 values (contrast thresholds) improved (reduced) as well after the training.
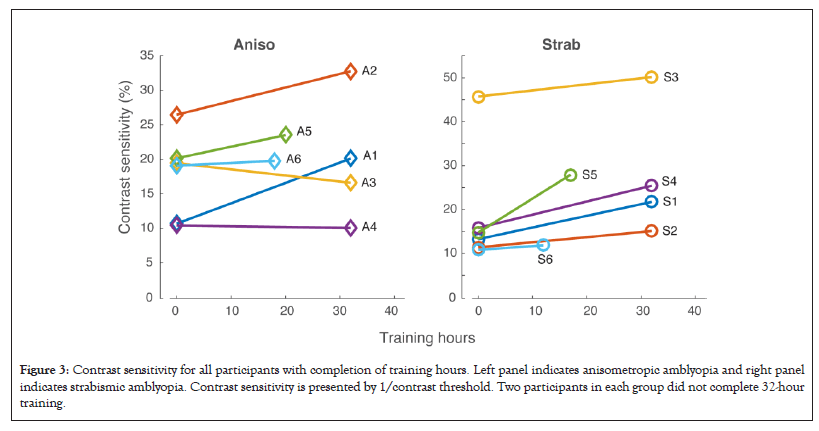
Figure 3: Contrast sensitivity for all participants with completion of training hours. Left panel indicates anisometropic amblyopia and right panel indicates strabismic amblyopia. Contrast sensitivity is presented by 1/contrast threshold. Two participants in each group did not complete 32-hour training.
Contrast response function and contrast sensitivity measurement
Contrast response function was measured in the amblyopic eye before and after training with a psychophysical procedure. Specifically, the orientation discrimination tasks of Gabor at various contrast levels were used via a procedure of constant stimuli while the fellow was covered, in which a single Gabor (2°, 2 cpd) was presented in the central area (2.5°) for 60 ms duration followed by a 200 ms noise mask. Participants were asked to report the orientation of the Gabor (horizontal or vertical). Contrast response function was revealed as the correct orientation responses against the contrasts. Then we used a modified Weibull function to fit the contrast response function.
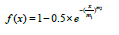
Where, x is the contrast and m1 and m2 are free scalar parameters.
Then, contrast threshold was defined as the contrast at 75% correct orientation responses.
Contrast Sensitivity (CS) was presented as 1/contrast threshold.
Statistical analysis
Significant differences between pre- and post-training as shown in Figures 4A and 4B were identified by two-tailed, Wilcoxon Signed-Rank Test for paired samples. Significant differences between improvement and pre- training baseline as shown in Figure 4C were identified by one-tailed Wilcoxon Signed-Rank Test for a single sample. Significant difference in improvement between subgroup of anisometropic and strabismic amblyopia was identified by two-tailed, Mann-Whitney Test for two independent sample. Correlation and significance in Figure 5 were calculated using one-tailed Spearman’s rho. The Real Statistics Resource Pack (RSSP) software was used for statistical analysis.
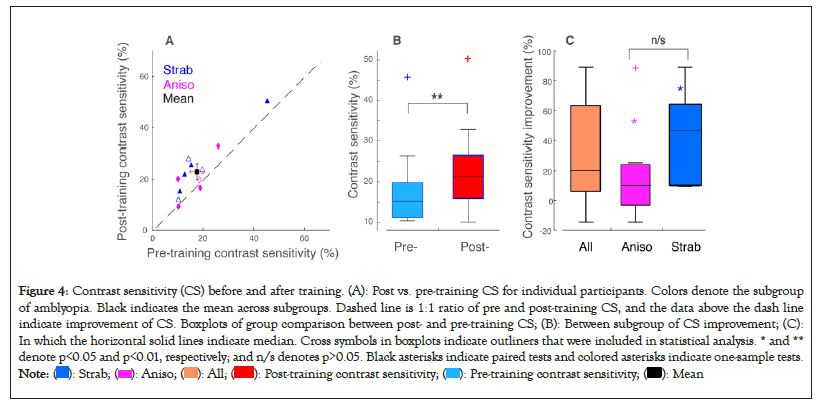
Figure 4: Contrast sensitivity (CS) before and after training. (A): Post vs. pre-training CS for individual participants. Colors denote the subgroup
of amblyopia. Black indicates the mean across subgroups. Dashed line is 1:1 ratio of pre and post-training CS, and the data above the dash line
indicate improvement of CS. Boxplots of group comparison between post- and pre-training CS; (B): Between subgroup of CS improvement; (C):
In which the horizontal solid lines indicate median. Cross symbols in boxplots indicate outliners that were included in statistical analysis. * and **
denote p<0.05 and p<0.01, respectively; and n/s denotes p>0.05. Black asterisks indicate paired tests and colored asterisks indicate one-sample tests.  .
.
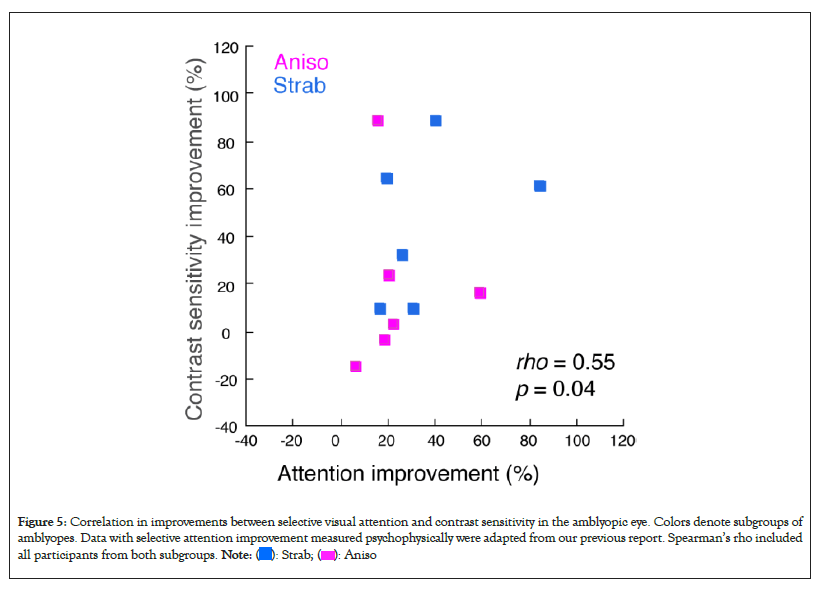
Figure 5: Correlation in improvements between selective visual attention and contrast sensitivity in the amblyopic eye. Colors denote subgroups of
amblyopes. Data with selective attention improvement measured psychophysically were adapted from our previous report. Spearman’s rho included
all participants from both subgroups.  .
.
Contrast response function improved after training
Contrast response function improved (shifted leftward) after training for the majority of participants (10 out of 12, S7 was excluded due to withdrawal from the study), compared to that before training, suggesting that training improves contrast response function in most adults with amblyopia. Figure 2 plots the sample data of the contrast response function from one of each amblyopic subgroup (Aniso: left panel; Strab: right panel). The correct orientation responses were plotted against the contrasts, in which the contrast threshold was defined at the contrast with 75% correct orientation responses (Figure 2).
Contrast sensitivity improved after training
We plot contrast sensitivity (1/threshold, referred to CS) for all participants with completion of training hours in Figure 3. Note that four participants (A5, A6, S5, S6) did not complete the training (32 hours, ~ 7000 trials of repetitive practice). Among these participants, S5 completed ~ 3700 trials (17 hours); S6 completed ~ 2600 trials (12 hours); A5 completed ~ 4500 trials (20 hours) and A6 completed ~ 4000 trials (18 hours). It appeared that these four participants, while they did not complete the whole training, also improved their CS after training. We took the contrast sensitivity measurement from their last visit as post-training contrast sensitivity (Figure 3).
Figure 4A plots contrast sensitivity improvement after training. As seen in Figure 4A, the majority of participants improved contrast sensitivity after the training (i.e., 10 out of 12 participants were above the dashed line). The mean difference between pre and post-training contrast sensitivity was significant (t=3.256, p<0.01). Significant differences between improvement and pre-training baseline were also identified, as shown in Figure 4C (All, t=3.106, p<0.01; Aniso, t=2.571, p<0.05; Strab, t=3.363, p<0.05). Contrast sensitivity improved an average of 31.73% across all participants, and there was no significant difference in contrast sensitivity improvement between subgroups of anisometropic and strabismic amblyopia (t=1.5495, p=0.1495), which might be due to the small sample size in our study. Previous studies also reported no clear difference in the training outcome between these subgroups (Figures 4A-4C) [40].
Correlation in improvements between selective attention and contrast sensitivity
After two months of training with dichoptic attention tasks, selective visual attention to the amblyopic eye for all participants improved significantly, which was measured both psychophysically and electrophysiologically and had been reported in our first study. To learn whether there is a correlation in improvements between selective attention and contrast sensitivity in the amblyopic eye, we plot CS improvement against attention improvement measured psychophysically in Figure 5, in which the attention improvement data were adapted from our first report. Spearman’s rho revealed significant correlation between CS improvement and attention improvement, suggesting that improving selective visual attention to the amblyopic eye correlates to the contrast sensitivity improvement in the amblyopic eye (Figure 5).
This study is the first to correlate selective visual attention improvement with contrast sensitivity improvement in amblyopic training. We demonstrated that training with dichoptic attention tasks that excluded low-level visual features (i.e., discrimination of contrast orientation or spatial frequency) improved contrast sensitivity in the amblyopic eye for both anisometropic and strabismic amblyopes, in which the magnitude of contrast sensitivity improvement significantly correlated with selective attention improvement. These findings suggest that selective visual attention to the amblyopic eye in training plays an important role in the success of amblyopic training.
Attention mechanisms in amblyopic training
There is converging evidence suggesting attention deficits in individuals with amblyopia. Attention commonly selectively biases to the non-amblyopic fellow eye of strabismic amblyopes and their visual input from the amblyopic eye seems to be ignored. These observations are likely the consequences of interocular suppression in amblyopia trying to prevent visual confusion caused by double vision (strabismus) or visually blur (anisometropia). Therefore, improving selective visual attention to the amblyopic eye might be an important factor in amblyopic training. This speculation was proved from our studies. In our first report, we found significant correlation between interocular suppression and the bias of attention between the two eyes of amblyopes. We found that improving attentional deployment in the amblyopic eye by training with attention tasks linearly correlated to a decrease of interocular suppression and improvement of visual acuity across training sessions. Because visual acuity is linked with interocular suppression in amblyopia [41,42], it is not surprising that alleviating suppression resulted in visual acuity improvement in amblyopes. In the current study, we demonstrated how training with dichoptic attention tasks improved contrast sensitivity in adults with amblyopia. Contrast sensitivity relates the visibility of a spatial pattern to both its size and contrast that reflect primarily V1 functions and is therefore a more comprehensive assessment of visual function than visual acuity that only determines the smallest resolvable pattern size [43].
Why does improving selective attention to the amblyopic eye result in contrast sensitivity improvement? In addition to the mechanism of a relationship between interocular suppression and attention bias between the two eyes of amblyopes as described above, another mechanism might be a close link between attention and contrast gain as we proposed and examined in the current study [44]. In a widely accepted framework, attention increases contrast sensitivity via increasing contrast gain, an effect akin to an increase of contrast in the physical contrast stimulus [45,46]. Therefore, it seems plausible to think that implementing selective attention tasks to the amblyopic eye in training works by improving contrast gain in the primary visual cortex (V1), which reflects the improvement in contrast sensitivity as we observed in our study.
Implications and limitations
The proposal of implementing selective attention tasks to the amblyopic eye in amblyopic training described above applies to any training tasks, including low-visual feature-based tasks (e.g., spatial frequency-based or contrast sensitivity-based tasks). This is because any tasks, even the simplest of tasks, require three components: a stimulus representation area, a decision unit (e.g., attention at intraparietal sulcus; decision making at prefrontal cortex) and a connection pathway between them [47]. Implementing tasks in the amblyopic eye is key for promoting attention to the amblyopic eye. Although our study is limited with a small sample size (12 with one participant who withdrew), it acts as a hypothesis driven pilot study because of novel and complex study design. All of the participants had MRI-informed EEG source imaging to evaluate whether attentional deployment truly improved at the intraparietal sulcus (a region known to be involved in visual attention) by attention training [48,49]. We also performed psychophysical procedures to evaluate contrast response function and contrast sensitivity before and after training. Our robust results demonstrate the importance of implementing attention tasks to the amblyopic eye in amblyopic training. The outcomes we discovered from this study can be used in future designs for amblyopic training paradigms for both adults and children.
Other factors in amblyopic training
In the current study, it appeared that four participants (A5, A6, S5 and S6), who did not complete all training sessions, also improved their contrast sensitivity after training. In general, perceptual learning follows fast-learning and slow-learning phases. Fast-learning usually happens within the first two to four sessions (roughly 1000-2000 trials), quickly followed by a slow-learning phase that slowly reaches asymptotic performance [50]. After 7000 trials, naïve observers show no further improvement. Most previous studies have used either a fixed duration of practice (typically 10-20 hours) or 4000-8000 trials [51-53]. These four participants who did not complete the training (the least training was S6, who had 12 hours of training with about 2600 trials of practice) had still performed over 2500 trials. This was considered past the fast-learning phase, and so they had likely moved into the slow-learning phase, therefore they still showed contrast sensitivity improvement. This finding is in line with previous amblyopic studies.
We should also point out that most participants (eight out of twelve) in our study were between the ages of 49-66 years old, which were older than the participants in previous studies that included attention factors. For example, the three participants in Ooi, et al. [54] study were 24, 26 and 38 years old. In general, younger individuals have more neuroplasticity for recovering visual functions [55,56]. This effect of age was also evident in our study. In two participants (S2 and S4) who had both completed 7000 trials, the younger participant (S4, 28 years old) had greater CS improvement (60%), as compared to 35% of CS improvement for the older participant (S2, 62 years old). It was surprising and also encouraging for clinical application that contrast sensitivity improvement was even seen in participants around 60 years of age (S1=59, S2=62 and S6=66). This is robust evidence that amblyopic training with a dichoptic approach incorporating high-attention demand tasks in the amblyopic eye is an effective way of treating amblyopia, even in older adults.
Amblyopia is often considered irreversible in adults. We found significant contrast sensitivity improvement in amblyopic adults, even around 60 years of age, following the practice of high-attention demand tasks. Although this work is limited with a small sample size, taken as a pilot study, this work suggests that training with dichoptic attention tasks improves contrast sensitivity, indicating that selective visual attention to the amblyopic eye in training plays an important role in the success of amblyopic training. Training with a dichoptic approach that incorporates attention demand tasks in the amblyopic eye, might be an effective way of treating amblyopia.
The authors thank Xie Jie Lai for contributing to the study design, programming the stimuli and data collection. The authors also thank Spero C. Nicholas for programming the stimuli and data analysis, Terence Tyson for data collection and Margaret Q. McGovern for assistance in recruiting the participants.
This work was supported by NIH grants R01- EY025018 (C.H.) and R01- EY035346 (C.H.) and grants from The Smith-Kettlewell Eye Research Institute and Pacific Vision Foundation to C.H.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Munares GA, Uner IJ, Hou C (2023) Improvement of Contrast Sensitivity in Adults with Amblyopia through Dichoptic Attention Task Training. J Clin Exp Ophthalmol. 14:956.
Received: 28-Aug-2023, Manuscript No. JCEO-23-25902; Editor assigned: 30-Aug-2023, Pre QC No. JCEO-23-25902 (PQ); Reviewed: 13-Sep-2023, QC No. JCEO-23-25902; Revised: 20-Sep-2023, Manuscript No. JCEO-23-25902 (R); Published: 29-Sep-2023 , DOI: : 10.35248/2155-9570.23.14.956
Copyright: © 2023 Munares GA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.