Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2023)Volume 14, Issue 1
Purpose: To evaluate the Verion™ image guided system compared with the axis registration method for toric Intraocular Lens (IOL) alignment in a Japanese population.
Methods: This retrospective, comparative case series study included eligible patients undergoing cataract surgery and toric IOL implantation (SN6AT3-6, Alcon) at a single Japanese surgical site (Miyata Eye Hospital, Miyazaki, Japan). Patients were divided into two groups based on the method used to determine axis alignment for toric IOL implantation; the image-guided group, with an intraoperative guidance system (Verion, Alcon), and the manual and topography-based axis registration group. At 1 month postoperatively, subjective cylindrical power and Uncorrected Distance Visual Acuity (UDVA) were evaluated.
Results: A total of 168 eyes of 143 patients were included in the study (image-guided group: 49 eyes; axis registration group: 119 eyes). For the image-guided and axis registration groups, the mean postoperative subjective cylindrical power was <0.8 D and similar percentages of patients in each group achieved postoperative subjective cylindrical power of ≤ 0.5 D, between >0.5 D and ≤ 1.0 D, and >1.0 D, with each toric IOL tested. For both groups, mean UDVA was ~ 0.0 logarithms of Minimum Angle of Resolution (logMAR) and a monocular UDVA of 0.1 logMAR or better was achieved by a similar proportion of patients in each group. There were no significant differences in cylindrical power and UDVA between the two groups (P>0.05 for both outcomes).
Conclusion: The image-guided system and topography based-axis registration marking were similar in effectiveness with regard to astigmatic correction effect and visual UDVA outcomes. The use of image-guided systems for toric IOL alignment may provide additional benefits, such as less patient discomfort, decreased surgical duration, and a more streamlined workflow.
Alignment; Astigmatism; Axis registration; Image-guided system; Toric intraocular lenses; Verion; Cataract surgery
Astigmatism should be addressed at the time of cataract surgery to achieve the best postoperative visual outcomes. Approximately 20% to 30% of patients who have cataract surgery have corneal astigmatism of 1.25 diopters (D) or higher, which when uncorrected during surgery, will result in postoperative spectacle dependency [1-3]. In patients who desire emmetropia and postoperative spectacle independence for distance vision, toric Intraocular Lens (IOL) implantation has been shown to be a safe and effective treatment option for correcting astigmatism [4-6]. Approximately 70% to 97% of patients are spectacle-independent for distance vision following toric IOL implantation [7-9]. Accurate positioning of a toric IOL is the most important factor in determining the efficacy of the astigmatism correction. Previous studies have shown that every degree of misalignment reduces the effectiveness of astigmatic correction by ~ 3.3%, while >30° of off-axis rotation will lead to a complete loss of cylinder correction from the IOL [10-13].
Accurate corneal marking is a critical step when orienting the axis of a toric IOL within the capsular bag. Since the introduction of the toric IOL, many manual marking techniques have been used for the alignment of toric IOLs [14,15]; however, most methods are at risk of misalignment due to the head tilt and cyclotorsion from patient postural changes occurring during measurement and horizontal meridian marking. Studies have found that the mean magnitude of this cyclotorsion was approximately 2° to 4°, with some patients having up to 14° of cyclotorsion [16,17]. Various marking methods have been described and of these, manual marking is commonly used at present. In a study by Visser et al. [14] the use of a 3-step ink-marker procedure led to a mean error of 4.9 ± 2.1° in toric IOL alignment. Popp et al. [15] compared slit-lamp, pendulum, bubble-marker, and tonometer manual methods for marking the eye and the mean errors ranged from 1.8 ± 2.2° (pendulum) to 4.7 ± 2.9° (tonometer). The alignment error may be larger in individual cases because of fading out of the ink markings, horizontal or vertical translocation of the ink marks, or even complete washout of the ink marks at the time of surgery. Additionally, because the IOL is smaller than the dimensions of these peripheral cornea marks, the surgeon must interpolate these points intraoperatively to estimate the final correct axis of alignment.
We have previously reported that the axis registration method using topography identification of manual meridian marks may yield a more accurate axis alignment than conventional methods, which can be affected by postural changes [18]. Several image-guided modalities, such as the Verion™ image guided system (Alcon Vision LLC), have been developed for precise toric IOL alignment that obviate the need for preoperative axis marking and aim to decrease the subjectivity associated with manual marking [19-23]. Verion uses a preoperative high-resolution photograph and registration of the patient's eye based on iris landmarks, limbus, and scleral blood vessels to allow intraoperative digital guidance of toric IOL alignment. No study has compared the accuracy of an image-guided system with the axis registration marking technique for toric IOL alignment. We herein evaluated the impact of the Verion image guided digital marking technique and the axis registration marking technique on postoperative visual and refractive outcomes.
Patients and study design
This retrospective study evaluated outcomes in patients who underwent cataract surgery and toric IOL implantation from November 2011 to October 2018 at the Miyata Eye Hospital in Miyazaki, Japan. All enrolled patients provided informed consent and the study was approved by the institutional ethics committee and conducted in accordance with the Declaration of Helsinki. Patients included in the study did not display ocular diseases or conditions apart from cataract diagnosis. The exclusion criteria included previous ocular or intraocular surgery, acute or chronic corneal infection, and inflammatory ocular conditions, diabetic macular disease, and patients with postoperative corrected distance visual acuity of >0.15 logMAR.
Toric intraocular lenses
AcrySof® IQ aspheric toric IOLs (models SN6AT3-6, Alcon Laboratories, Inc.) were implanted with cylindrical powers ranging from 1.50 D (T3) to 3.75 D (T6), increasing in 0.75 D steps. The OA-2000 optical biometer was used to calculate axial length and the cylindrical power of the toric IOL was calculated using the Alcon® online Toric IOL calculator.
Surgical technique
All surgeries in this study were performed by 1 of 4 experienced surgeons at the same surgical center. The surgical technique, except the method of marking for toric IOL alignment, was standardized in each patient. In all cases, a standard divide and conquer phacoemulsification technique was performed through a superior clear sclerocorneal incision. The IOL was subsequently positioned in the capsular bag based on the IOL implantation axis determined using each alignment method.
Preoperative corneal marking and intraocular lens alignment
Patients were divided into two groups based on the method used to determine axis alignment for toric IOL implantation; the image-guided group with an intraoperative guidance system (Verion, Alcon), and the axis registration group. The axis registration technique consisted of preoperative marking of the patient’s eye under a slit-lamp microscope while the patient was in a seated position. In Figure 1A, marking was performed using an axis marker (AE-2748, ASICO LLC), which created a straight line and an impression from the temporal cornea to the conjunctiva (keratoconjunctival mark). Subsequently, an image of the eye including the keratoconjunctival mark was taken with a corneal topographer (TMS-4A, Tomey), and the angle between the steep meridian and the keratoconjunctival mark was determined. The axis for IOL implantation was calculated using a toric calculator and corrected for the corneal topographic angle based on the steep meridian. At the start of surgery, with the patient in a supine position, a securing ring with angle indices (AE-1591, ASICO LLC) was matched with the keratoconjunctival mark and fixed. Marking was performed at the incision position at 90° to the IOL implantation axis, corrected for the corneal topographic angle (Figure 1A).
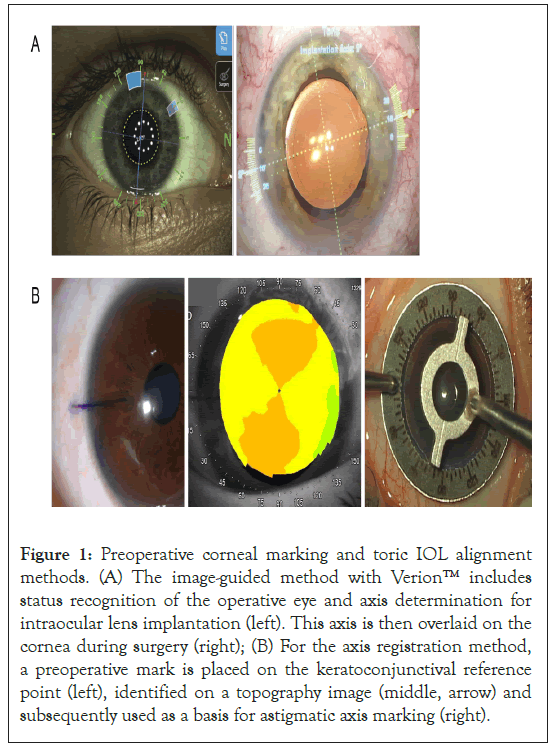
Figure 1: Preoperative corneal marking and toric IOL alignment methods. (A) The image-guided method with Verion™ includes status recognition of the operative eye and axis determination for intraocular lens implantation (left). This axis is then overlaid on the cornea during surgery (right); (B) For the axis registration method, a preoperative mark is placed on the keratoconjunctival reference point (left), identified on a topography image (middle, arrow) and subsequently used as a basis for astigmatic axis marking (right).
The Verion image guided system, which consists of a measurement module and a digital marker, was used to perform digital marking for toric IOL alignment. Preoperatively, a high-resolution color reference image of the patient’s eye was obtained using the measurement module with the patient in a seated position. The software auto-detects the limbus, the location of limbal vessels, the scleral vessels, and iris features, which were used for intraoperative image registration as shown in Figure 1B. Preoperatively, corneal radius of curvature, astigmatism, astigmatic axis, pupil diameter and corneal ring diameter are measured simultaneously. The measured features of the patient's eye are used to determine the target incision location and calculate the center of the anterior capsule incision. The preoperative images are transferred to the digital marker. Using multiple reference points on the conjunctiva and limbus, a digital overlay of the imported preoperative image and live-surgery image is created. Owing to the eye-tracking navigation of the system, cyclotorsion and eye movements are eliminated. Intraoperatively, the incision position, the guide to the anterior capsule incision, the toric axis and the IOL fixation position are displayed in the microscope field of view (Figure 1B).
Refractive and visual outcomes
At the 1 month postoperative follow-up visit, subjective cylindrical power and monocular Uncorrected Distance Visual Acuity (UDVA) were assessed. UDVA was measured using Landolt C optotypes at 5 m. Patients were asked to respond to the orientation of the gap in a C and start at the smallest row in which the orientations were easily distinguishable. Patients were asked to continue to respond to the gap orientations with smaller C’s until none were read correctly. The Landolt C visual acuity values were transferred into logarithm of Minimum Angle of Resolution (logMAR) values for use in the analyses.
Statistical analysis
All data are expressed as the mean ± standard deviation. Differences in outcomes between groups were analyzed using the MannWhitney U test and χ² test. In all tests, a threshold of statistical significance was assumed equal to a P value of 0.05.
Of the patients who underwent cataract surgery and toric IOL implantation at the Miyata Eye Hospital from November 2011 to October 2018, 168 eyes of 143 eligible patients were assigned to the image-guided group or the axis registration group based on the method used to determine axis alignment for toric IOL implantation. The image-guided group comprised 49 eyes and the axis registration group comprised 119 eyes. Study participants were of Japanese race. Patient demographics and baseline characteristics were similar between groups. Overall, the mean age of patients was 73.7 ± 12.0 years and 47.6% of eyes were from female patients as shown in Table 1. Preoperatively, there were no statistically significant differences in corneal astigmatism between the two groups for each toric IOL model evaluated (P>0.05) as shown in Table 2. No complications occurred during any surgery or postoperatively (Tables 1 and 2).
| Parameter | N=168 | |
|---|---|---|
| Mean age ± SD, years | 73.7 ± 12.0 | |
| Image-guided | Axis registration | |
| Total n (%) | 49(29.2%) | 119(70.8%) |
| Mean age ± SD, years | 75.3 ± 11.0 | 73.6 ± 11.0 |
| Age range, years | (21-91) | (15-92) |
| Sex n(%) | ||
| Male | 26(53.1%) | 62(52.1%) |
| Female | 23(46.9%) | 57(47.9%) |
| Race, n(%) | ||
| Asian (Japanese) | 49(100%) | 119(100%) |
| Toric IOL, n(%) | ||
| SN6AT3 (n=9) | 3 | 6 |
| SN6AT4 (n=42) | 11 | 31 |
| SN6AT5 (n=68) | 24 | 44 |
| SN6AT6 (n=49) | 11 | 38 |
Note: n: Number of eyes in the treatment group; SD: Standard Deviation; IOL: Intraocular Lens
Table 1: Baseline demographics and sample sizes of the patient study population.
| Astigmatism power (Mean D ± SD) | |||
|---|---|---|---|
| Toric IOL | Image-guided | Axis registration | P value |
| SN6AT3 | 1.50 ± 0.43 | 1.50 ± 0.39 | 1 |
| SN6AT4 | 1.70 ± 0.29 | 1.60 ± 0.36 | 0.39 |
| SN6AT5 | 1.96 ± 0.28 | 2.19 ± 0.62 | 0.56 |
| SN6AT6 | 2.43 ± 0.37 | 2.45 ± 0.92 | 0.25 |
Note: D: Diopters; IOL: Intraocular Lens; SD: Standard Deviation
Table 2: Preoperative corneal astigmatism (D).
At 1 month post-surgery, subjective cylindrical power results for image-guidance compared with axis registration toric IOL alignment demonstrated no significant differences for the 4 IOLs (P>0.05 for each lens). Postoperative subjective cylindrical power in the image-guided and axis registration group was 0.50 ± 0.00 D and 0.33 ± 0.41 D with SN6AT3; 0.73 ± 0.65 D and 0.65 ± 0.44 D with SN6AT4; 0.68 ± 0.56 D and 0.77 ± 0.47 D with SN6AT5; and 0.59 ± 0.41 D and 0.57 ± 0.49 D with SN6AT6, respectively as shown in Figure 2A.

Figure 2: Postoperative subjective cylindrical power at 1 month. (A) Mean astigmatism power (B and D) Percentage of patients achieving a cylindrical power of ≤ 0.5 D, between >0.5 D and ≤ 1.0 D, or >1.0 D. n numbers (eyes) for SN6AT3: image-guided (n=3), axis registration (n=6); SN6AT4: image-guided (n=11), axis registration (n=31); SN6AT5: image-guided (n=24), axis registration (n=44); SN6AT6: image-guided (n=11), axis registration (n=38).
 .
.
Figure 2B shows similar percentages of patients in the image-guided and axis registration groups achieved postoperative subjective cylindrical power of ≤ 0.5 D, between >0.5 D and ≤ 1.0 D, and >1.0 D with each toric IOL tested (Figures 2A and 2B).
No significant differences in visual acuity were observed between the groups for each toric IOL model (P>0.05) as shown in Figure 3A. At 1 month postoperatively, the mean monocular UDVA in the image-guided and axis registration group was –0.03 ± 0.05 logMAR and –0.02 ± 0.14 logMAR with SN6AT3; 0.04 ± 0.14 logMAR and 0.04 ± 0.12 logMAR with SN6AT4; 0.04 ± 0.19 logMAR and 0.08 ± 0.16 logMAR with SN6AT5; and 0.03 ± 0.16 logMAR and 0.01 ± 0.14 logMAR with SN6AT6, respectively. Figure 3B additionally shows a monocular UDVA of 0.1 logMAR or better was achieved by 100% and 83% of eyes with SN6AT3; 82% and 84% of eyes with SN6AT4; 75% and 59% of eyes with SN6AT5; 64% and 87% of eyes with SN6AT6; in the image-guided and axis registration group respectively (Figures 3A and 3B).
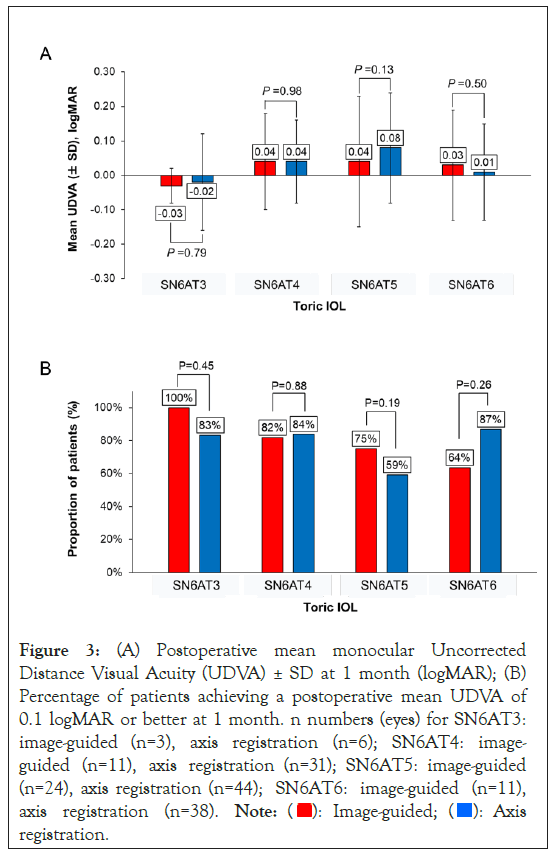
Figure 3: (A) Postoperative mean monocular Uncorrected Distance Visual Acuity (UDVA) ± SD at 1 month (logMAR); (B) Percentage of patients achieving a postoperative mean UDVA of 0.1 logMAR or better at 1 month. n numbers (eyes) for SN6AT3: image-guided (n=3), axis registration (n=6); SN6AT4: image-guided (n=11), axis registration (n=31); SN6AT5: image-guided (n=24), axis registration (n=44); SN6AT6: image-guided (n=11), axis registration (n=38). 
 .
.
In the present retrospective study, we compared two methods of toric IOL alignment. One was a Verion image guided system that uses a preoperative high-resolution photograph and intraoperative registration of the patient's eye based on scleral/limbal vessels to allow digital surgical guidance and alignment of the toric IOL. The second was a corneal topography-based axis registration marking method that comprises three steps: placing a mark and impression on the cornea and conjunctiva, identifying this mark in the topographic image, and aligning the IOL based on the location of the mark. No previous studies have compared the refractive and visual outcomes of these two marking techniques. In the 168 eyes of 143 patients that were evaluated, the results were good with both methods, with subjective cylindrical power <0.8 D and mean UDVA of ~ 0.0 logMAR at 1 month postoperatively. There were no significant differences in subjective cylindrical power or UDVA between the two groups with each toric IOL tested.
These results are in line with previous studies comparing digital and manual marking, which showed comparable visual outcomes between methods [24]. The prior studies also demonstrated superior alignment of the toric IOL with the image-guided systems. For example, Webers et al. [20] showed that IOL misalignment was significantly reduced with Verion digital marking than with manual marking; but this did not result in improved UDVA or lower residual refractive astigmatism. Similarly, a prospective study by Elhofi et al. [22] showed that at 3 to 5 weeks post-surgery, the UDVA was similar for the Verion and manual-marking groups; however, the IOL misalignment and the mean deviation from targeted induced astigmatism was significantly higher in the group that underwent manual marking. Comparable UDVA outcomes and improved toric IOL alignment have also been demonstrated with the Callisto eye image-guided system against conventional manual marking methods. Interestingly, Titiyal et al. [24] demonstrated improved visual quality outcomes with the Callisto eye system, as evidenced by higher internal Strehl ratio and modulation transfer function. Future comparative studies using different marking techniques (conventional, digital, or axis registration) should evaluate the alignment errors of toric IOLs and effects on visual quality.
The axis registration method has the advantage of impression identification using topography, which acts to confirm the geographic relation between the mark and the steep meridian and also resolves the issues of washout or fadeout of marking during surgery. Thus, it is aimed at avoiding misalignment of the steepest meridian induced by head tilting and cyclotorsion during examination, meridian marking, and surgery. Furthermore, the axis registration method reportedly reduced variations in the astigmatic correction effect during limbal relaxing incision surgery compared with conventional corneal marking methods. The limitations of manual marking are effectively addressed by image-guided systems, which are integrated with the surgical microscope and the graphic overlay simplifies the process of toric IOL alignment and enhances its accuracy. The use of image-guided systems for toric IOL alignment also eliminates patient discomfort associated with manual marking. Furthermore, a faster preoperative procedure, toric IOL alignment time, and in turn, overall surgical duration time, has been observed with the use of image-guided systems, which has several benefits including a more streamlined workflow and decreased risk of complications such as anterior chamber bacterial contamination.
AcrySof® toric IOLs are some of the most commonly used toric IOLs in cataract surgery. A previous study by Kim et al. [25] showed that the AcrySof® SA60T toric IOL, which utilizes a design similar to the toric IOL used for this study, is effective in reducing refractive astigmatism, providing good uncorrected visual outcomes and maintaining rotational stability up to approximately 13 months after implantation. Additionally, data from Weinand et al. [26] showed excellent rotational stability for the AcrySof® SA60AT IOL; median postoperative rotation was 0.7° (range, 0.1° to 1.8°) in 17 eyes at 6 months and no IOL rotated ≥ 1.8°.
The standardized Landolt C optotype chart was used to assess visual outcomes in this Japanese study population, in contrast to the Early Treatment of Diabetic Retinopathy Study (ETDRS) chart, which has been used in similar studies [27]. The Landolt C test uses a single optotype placed in different positions; up, down, left, right, and 45° positions in between. Because there is only one optotype, patients must gesture which position they see the optotype facing, making it helpful for testing patients that are not familiar with the Roman alphabet. Importantly, studies have shown that the Landolt C test and the ETDRS test yield comparable results in visual acuity and test-retest reliability [28,29].
Limitations of the present study include the retrospective study design, a short follow-up period of 1 month, and the unequal group sample sizes. The lack of alignment error assessment and not direct measurement of posterior corneal astigmatism are additional limitations and makes cross-study comparisons more difficult. Future trials should evaluate the comparative long-term effectiveness and outcomes of the Verion intraoperative image guided system, as well as patient and physician preference.
In conclusion, both the image-guided and axis registration marking methods showed good and similar postoperative outcomes in toric IOL recipients. Although this study did not show significant advantages in terms of UDVA and refractive astigmatism using the digital marking system, potential advantages of image-guided systems include less patient discomfort, a more streamlined workflow, and decreased surgical duration. Further studies will be required to determine whether there are differences in the alignment error between the marking methods and whether potential differences are clinically relevant in a patient population with higher levels of preexisting corneal astigmatism.
We thank the participants of the study. The authors thank Aarti Shah for editorial assistance in the preparation of the manuscript, with funding from Alcon Japan Ltd.
This study was supported by Alcon.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kinoshita K, Mori Y, Nejima R, Nagai N, Minami K, Miyata K (2023) Image-Guided System versus Axis Registration Technique for Toric Intraocular Lens Alignment in Cataract Surgery. J Clin Exp Ophthalmol. 14:940.
Received: 28-Dec-2022, Manuscript No. JCEO-22-20757 ; Editor assigned: 30-Dec-2022, Pre QC No. JCEO-22-20757 (PQ); Reviewed: 13-Jan-2023, QC No. JCEO-22-20757 ; Revised: 20-Jan-2023, Manuscript No. JCEO-22-20757 (R); Published: 30-Jan-2023 , DOI: 10.35248/2155-9570.23.14.940
Copyright: © 2023 Kinoshita K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.