Journal of Bone Research
Open Access
ISSN: 2572-4916
ISSN: 2572-4916
Case Report - (2022)
Bone formation in tissues without ossification properties such as muscles and connective tissues can be defined as Heterotopic Ossification (HO). It is a relevant issue for surgeons performing TMJ reconstruction with TMJ prostheses. The objective of this study was to analyze and compare previous literature findings regarding etiology, diagnosis, prophylaxis and further treatment and management of heterotopic bone formation around TMJ prostheses. Besides, a 16-year-old male clinical-case with 19-years follow-up is reported. The search strategy of this scoping review was performed in three different databases (MEDLINE, ELSEVIER and Cochrane) by three independent reviewers (NJS, GST, PHAC), the selection and analysis of the scientific articles was performed according to the following criteria: specific studies that evaluated the presence of heterotopic bone formation in TMJ prosthesis; studies on humans and reported in English language. This study provides qualitative and quantitative reviews of information regarding etiology, diagnosis, prevention, and management of HO around TMJ prostheses. Several management protocols were proposed, ranging from simple HO resection and prosthesis removal to autologous fat graft and low dose radiation therapy, with varying success rates. Nevertheless, further investigation is required to formulate a standardized prevention/management protocol to aid surgeons obtain long-term success in TMJ replacement procedures in the future.
Heterotopic ossification; Temporomandibular joint; Ankylosis; TMJ prosthesis
Heterotopic ossification (HO) is the presence of bone in non- osseous tissues, or more accurately formation of ectopic lamellar bone in muscles or joint apparatus [1]. The outcome of such bone formation is limitation of muscular mobility and subsequent joint immobility. HO is most frequently associated with musculoskeletal trauma, amputations, spinal cord injury, tumors, vasculopathies, or central nervous system injury [2]. Furthermore, genetic disorders such as fibrodysplasia ossificans progressive and progressive osseous heteroplasia have been linked to HO [3].
TMJ prostheses have become an essential treatment option for reconstruction of ankylosed joint. They are a safe, reliable, and effective treatment option for selected TMJ disorders [4]. However, several immediate and long-term complications have been reported. Among the immediate complications are: Pain, swelling, facial ecchymosis, temporary or permanent facial paralysis (motor nerve), temporary or permanent paresthesia, hearing problems, Eustachian tube inflammation/infection, etc. [5]. Whereas delayed/long term complications comprise: heterotopic bone formation, dental malocclusion, TMJ prosthesis complications (foreign body reaction, fracture or loosening of implant components, functional compromise to contralateral TMJ), among others [6,7].
Several management options of HO have been suggested in the literature, including resection, a temporary spacer, and removal of the prosthesis with replacement at a second procedure. Also, atraumatic removal of the prosthesis, resection of the heterotopic tissue, replacement of the prosthesis into its previous position, and then packing of fat around the articulation represents a technique that both minimizes morbidity and reduces costs [2]. Moreover, radiation therapy in prophylaxis and management has been suggested with low rates of treatment-related toxicity [1,8]. This study was conducted to analyze and compare previous literature findings regarding etiology, diagnosis, prophylaxis and further treatment and management of heterotopic bone formation around TMJ prostheses.
Literature review
The search strategy of this scoping review was performed in MEDLINE (Medical Literature Analysis and Retrieval System Online, via PubMed), ELSEVIER (via Scopus), and Cochrane Library databases scanning the subjects using eight descriptors: “Heterotopic”; “bone” OR “ossification”; “TMJ” OR “temporomandibular joint”; “prosthesis” OR “replacement” OR “reconstruction”, in December 2018.
Three independent reviewers (NJS, GST, PHAC) performed the initial selection and analyzed titles and/or abstracts according to the following inclusion criteria: specific studies that evaluated the presence of heterotopic bone formation in TMJ prosthesis; studies on humans and reported in English language without time restriction regarding to publication date; and case series, retrospective or prospective clinical design. Studies in non-English language, animal studies or reviews were excluded. Assuming general results, the inclusion criteria were performed without specifying the type of prosthesis and technique, and quantify or qualify the heterotopic bone formed. Full-text reading was performed after initial selection according to inclusion criteria to define the final included studies. Reviewers to solve any disagreements performed additional discussion.
Data extraction were performed including the following variables: study design; number of patients, age and gender; motive of first intervention for prosthesis installation; number of prostheses for each patient; prosthesis affected on each patient; post-operative time until heterotopic bone formation after prosthesis installation; signs and symptoms; type and success of treatment; and further relevant information. Again, disagreements between reviewers were solved by further discussion. Data were analyzed by descriptive statistics.
A 16-years-old male presented to the department of OMFS at Dental School at Araraquara São Paulo State University in May 2000, with a history of mandibular trauma due to a bicycle accident 2 years earlier. The patient described a progressive reduction of Maximum Interincisal Opening (MIO) after the accident. He had an open reduction surgery performed on the left Temporomandibular Joint (TMJ) at the time of the accident, with prolonged intermaxillary fixation, for duration of 60 days. During evaluation, he presented with 3 mm maximal incisor opening, without excursive movements and an anterior open bite. Computerized Tomography (CT) examination showed bilateral TMJ ankylosis.
In July 2000, he was submitted to a surgical procedure under general anesthesia to remove the ankylotic bone bilaterally along with coronoidectomy via pre-auricular incision, with simultaneous costochondral graft using 02 thoracic ribs. Immediate post- operative maximal incisor opening was 40 mm, and physical therapy was indicated in the immediate post-operative period to maintain MIO.
In January 2001 ankylotic recurrence was noted at left TMJ. In January 2004, he was submitted to surgical procedure under general anesthesia for the removal of ankylotic bone formation in TMJ bilaterally, with simultaneous installation of bilateral bone distractors in the area between lateral incisor and first molar bilaterally with vertical corticotomies and subsequent distractors activation. In May 2005 and due to local infection of the bone distractors, they were removed surgically under local anesthesia. In December 2006, the patient was submitted to surgical installation of bilateral total TMJ prostheses (Walter Lorenz/Biomet TMJ Prostheses, Jacksonville, FL, USA), where he presented a mouth opening of almost 17 mm in 02 years post-operative time. In February 2010, the patient presented with facial deformity (micrognathia), 15 mm maximal incisor opening and anterior open bite. CT showed ankylosis over the prosthesis bilaterally (Figure 1A). In August 2016, he was submitted to bilateral prosthesis removal with simultaneous autogenous abdominal fat graft (Figure 1B). The future planning is TMJ reconstruction with custom- made prosthesis bilaterally, along with orthognathic surgery. The rationale is that advancement of the mandible with the prosthesis will allow more freedom of movement to the mandible and help to prevent reankylosis.
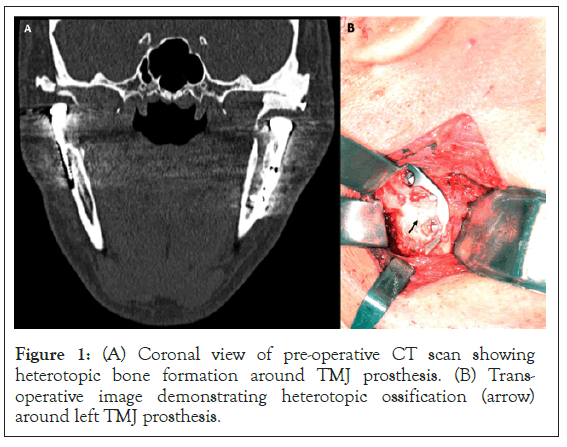
Figure 1: (A) Coronal view of pre-operative CT scan showing heterotopic bone formation around TMJ prosthesis. (B) Trans- operative image demonstrating heterotopic ossification (arrow) around left TMJ prosthesis.
The electronic search resulted in 68 articles (35 from PubMed; 33 from Scopus; none from Cochrane). After title and abstracts reading, 19 articles were selected (11 from PubMed; 8 from Scopus). These nineteen articles were grouped and the duplicated ones were removed resulting in 12 articles. After full-text reading of these 12 articles, 5 were considered relevant for this study. Seven papers were excluded after full-text reading due to irrelevant content, unavailable data or discussing heterotopic bone formation in TMJ without TMJ prosthesis.
The demographic information is shown in Table 1. Table 2 presents’ data regarding the initial intervention for prosthesis installation, for how long these prostheses were maintained without issues, and which were the signs and symptoms that led to heterotopic formation diagnosis. Table 3 refers to type and success of treatment; furthermore, shows relevant information for this study.
| Year | Authors | Study design | Number of patients | Age avg | Gender | Number of prosthesis | Prosthesis affected | ||
|---|---|---|---|---|---|---|---|---|---|
| 2016 | Selbong, et al. [2] | Case report | 3 | 55.4 (48-68) | 1F | 2M | 6 | 4 | |
| 2016 | Gerbino, et al. [9] | Retrospective | 38 | 45.1 | 29F | 9M | 55 | 1 | |
| 2014 | Sanovich, et al. [11] | Retrospective | 36 | 49.4 +/- 11.9 | 36F | 62 | 2 | ||
| 2014 | Guarda-Nardini, et al.[6] | Case report | 1 | 45 | 1F | 1 | 1 | ||
| 2010 | Jensen, et al. [11] | Retrospective | 12 | 35.25 (27-57) | 8F | 4M | 18 | 18 | |
Table 1: Study design, number of patients, and demographic aspects.
| Year | Authors | Cause of first intervention (prosthesis) | Time after prosthesis installation | Signs and symptoms |
|---|---|---|---|---|
| 2016 | Selbong, et al. [2] | restricted mouth opening and pain (3) | 9 years (2); 20 years (1) | restricted mouth opening – pain (3) |
| 2016 | Gerbino, et al. [9] | 12 bony and fibrous ankylosis | NI | reankylosis - restricted mouth opening pain |
| 13 degenerative joint disease | ||||
| 4 autoimmune systemic disease | ||||
| 3 pathology resection | ||||
| 1 substitution of previous prosthesis | ||||
| 5 congenital deformity or previous surgery | ||||
| 2014 | Sanovich, et al. [11] | 15 degenerative joint disease | 30 months | Decreased pain score and increased quality of life |
| 7 fibrous and bony ankylosis | ||||
| 6 previous failed TMJ prostheses | ||||
| 4 rheumatoid arthritis | ||||
| 3 trauma resulting in fracture | ||||
| 1 pathology | ||||
| 2014 | Guarda-Nardini, et al.[6] | Ankylosis | 10 years | Mouth opening limitation |
| 2010 | Jensen, et al. [12] | heterotopic ossification | >16 years | NI |
NI: Not Informed.
Table 2: Cause of intervention, time after prosthesis installation, and signs and symptoms.
| Year | Authors | Type of treatment | Success of treatment | Further relevant observations |
|---|---|---|---|---|
| 2016 | Selbong [2] | 2007 prosthesis removal and spacer insertion/2008 prosthesis insertion and additional resection with fat graft; prosthesis removal, heterotopic bone resection, bilateral coronoidectomy, prosthesis reinstallation;prosthesis removal, heterotopic bone resection, bilateral coronoidectomy, prosthesis reinstallation with fat graft | 5 y PO, MIO 26 mm, no pain; 18 months PO, MIO 26 mm, no pain; 16 months PO, MIO 25 mm, with dysaesthetic pain | NI |
| 2016 | Gerbino, et al. [9] | heterotopic bone resection, temporary prosthesis removal, packing of autogenous fat graft | NI | pre-op MIO 8.3mm ; PO MIO 35.7mm |
| 2014 | Guarda-Nardini, et al.[6] | Ankylotic block resection and TMJ prosthesis repositioning | 12 months PO, MIO 41 mm with no pain recurrence 10 years PO, MIO limitation and recurrent HO formation | Assessment of pre-operative risk factors for re-ankylosis and a within intervention prevention should be better standardized |
| 2010 | Jensen, et al. [12] | NI | radiation therapy | NI |
Abbrevations: NI: Not Informed; PO: Post-Operative, MIO: Maximal Interincisal Opening
Table 3: Type of treatment, Success of treatment, and further relevant observations.
In 2017, Gerbino, et al. conducted a retrospective study to analyze total alloplastic reconstruction of the TMJ using stock and custom- made Biomet prosthesis [9]. The study included 38 patients, 29 females and 9 males, average age category 45.1. Causes of primary intervention was bony and fibrous ankyloses in 12 cases, degenerative bone disease in 13 cases, autoimmune systemic disease in 4 cases, 3 pathological resection cases, 5 congenital deformity and previous surgeries, and 1 case of previous prosthesis substitution. In total 55 TMJ prosthesis was analyzed in this study and the following complications were recorded: bleeding in 2 cases, malocclusion in 1 case, and postoperative infection with subsequent prosthesis removal in 1 case, contralateral TMJ overload in 1 unilateral case, and heterotopic bone formation in 1 case. HO with reankylosis and restricted mouth opening was observed unilaterally in 1 patient with bilateral stock prostheses due to degenerative joint disease. Management modality included heterotopic bone resection, temporary prosthesis removal with simultaneous autologous fat graft. This management modality has been suggested by Mercuri and Wolford as a prophylaxis to heterotopic bone formation with excellent results [1,7,10].
In 2016, Selbong, et al. reported 3 cases of HO where atraumatic removal of the prosthesis and resection of heterotopic tissue was performed [2]. Followed by replacement of the prosthesis into previous position with simultaneous autologous fat packing around the articulation. The three patients, 2 males and one female with an average age of 55 years, all with bilateral TMJ prosthesis, were experiencing pain with restricted mouth opening. The longest period of pain-free follow-up was 5 years where the patient presented a mouth opening of 26 mm. This management modality showed good early results; however, long-term follow-up is required.
In 2014, Sanovich, et al. conducted a retrospective study to report the outcomes of TMJ replacement with Biomet Stock prostheses [11]. The study included 36 patients (26 bilateral, 6 left, and 4 right) with 62 prostheses, all females with an average age of 49.4 years. The etiology of first surgical intervention included: 15 cases of degenerative joint disease, 7 cases of fibrous and bony ankylosis, 6 cases of previous failed TMJ prosthesis, 4 cases of rheumatoid arthritis, 3 cases of fractures resulting from trauma and 1 case of TMJ pathology. After an average follow-up time of 30 months, an increase of more than 8 mm in average MIO was noted (pre- operative average MIO 26.1 mm as compared to 34.4 mm in post- operative. Moreover, improvements in criteria such as restrictions with eating, jaw functions, pain score and quality of life were observed. Of the 62 prostheses installed, 2 prostheses had to be removed and/or replaced due to heterotopic bone formation.
In 2014, Guarda-Nardini, et al. presented a case report in which heterotopic ossification occurred after a post-operative period of 10 years around TMJ prosthesis in a 45 years old female [6]. However, the authors deduced that, in this specific case, HO occurred several years after prosthesis installation that implies better evaluation of pre-operative risk factors and further understanding of prevention techniques.
A study conducted by Jensen, et al. in 2010 presented post- operative radiation therapy as a long-term prophylactic measure for prevention of recurrent HO [12]. This study comprised 12 patients (18 prostheses) where heterotopic ossification around TMJ prosthesis occurred and induced bony ankylosis of the joint. With a mean follow-up rate of 16, 4 years, low-dose radiation therapy for post-operative prophylaxis of TMJ HO has shown over 50% success rate in prevention of heterotopic bone formation in with relatively mild and infrequent treatment-related toxicity.
Several methods have been proposed in the literature to guide through diagnosis, prevention and management modalities of heterotopic bone formation. Nevertheless, there is not enough published data regarding this topic in the current literature to serve as a solid base. Further investigation and studies should be reported to form an evidence-based protocol to help clinicians in diagnosis, prevention and management of heterotopic ossification.
Citation: Salman NJ, Trento GS, Carvalho PHA, Gabrielli MAC, Gabrielli MFR, Sant’Ana E, et al. (2022) Heterotopic Ossification Around Temporomandibular Joint Prosthesis: Case Report and a Scoping Review. J Bone Res. S1:003.
Received: 03-Mar-2022, Manuscript No. BMRJ-21-9372; Editor assigned: 07-Mar-2022, Pre QC No. BMRJ-21-9372 (PQ); Reviewed: 21-Mar-2022, QC No. BMRJ-21-9372; Revised: 25-Mar-2022, Manuscript No. BMRJ-21-9372 (R); Published: 01-Apr-2022 , DOI: 10.35248/2572-4916.22.S1.003
Copyright: © 2022 Salman NJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.