Mycobacterial Diseases
Open Access
ISSN: 2161-1068
ISSN: 2161-1068
Case Report - (2023)Volume 13, Issue 3
Hansen’s disease presents with a spectrum of clinical manifestations ranging from lepromatous leprosy to tuberculoid leprosy. The course of the disease may be superseded by the leprosy reactions which are of two types, Type 1 and Type 2 reactions. A 61-year-old male initially diagnosed with scrofuloderma after Fine Needle Aspiration Cytology (FNAC) of the discharge from the swelling over the axilla and inguinal region which tested positive for Ziehl- Neelsen (ZN) stain. He was started on Anti-Tubercular Treatment (ATT). Five days after starting the ATT, the patient developed fever, edema of the bilateral lower limb, and generalized arthralgia. It was followed by the development of multiple tiny pustules over bilateral legs. A provisional diagnosis of acute generalized exanthematous pustulosis was considered and a skin biopsy was taken from the lesion. Histopathological examination revealed epidermis with pustule filled with neutrophils, superficial and deep dermis showed granulomatous inflammation. On further clinical examination, patient had thickening of bilateral ulnar nerve, right common peroneal nerve with no neuritis. On sensory examination, hypoesthesia noted over bilateral soles. On reviewing, the biopsy specimen showed edematous superficial and deep dermis with interstitial, perivascular and periappendageal inflammatory infiltrate comprising foamy macrophages, lymphocytes and polymorphs. The fite stain for Acid fast bacilli was positive and Bacterial Index (BI) was 5+. Acute Generalized Exanthematous Pustulosis (AGEP) is a severe cutaneous eruption with nonfollicular, sterile, pustules on an erythematous background associated with fever and leukocytosis. In the vast majority of cases medications are implicated, few theories of infectious etiologies are also suspected. Previous case reports of infectious etiology such as coccidioidomycosis, chlamydia, cytomegalovirus, and parvovirus have been described. This may implicate AGEP-like eruptions is also a rare presentation of Hansen’s reaction. The pustular lesion in Erythema Nodosum Leprosum (ENL) is an uncommon form of ENL and is a criterion for severe ENL. This case highlights the need for thorough clinical examination and histopathological correlation for diagnosing the new facets of Hansen’s disease.
Acute generalized exanthematous pustulosis (AGEP); Pustular ENL; Atypical hansen; Type 2 reaction; Erythema Nodosum Leprosum (ENL)
Hansen’s disease presents with a spectrum of clinical manifestations ranging from lepromatous leprosy to tuberculoid leprosy. The course of the disease may be superseded by the leprosy reactions which are of two types, type 1 and type 2 reactions. Here we report a rare presentation of Hansen’s disease with type 2 reaction morphologically presenting as acute generalized exanthematous pustulosis.
A 61-year-old male patient was referred to Dermatology OPD with complaints of multiple pustules over the bilateral lower limbs. The patient was initially diagnosed as a case of scrofuloderma after FNAC of the discharge from the swelling over the axilla and inguinal region which tested positive for ZN stain. He was started on Anti-Tubercular Treatment (ATT). Five days after starting the ATT, the patient developed fever, edema of the bilateral lower limb, and generalized arthralgia. It was followed by the development of multiple tiny pustules over bilateral legs. Cutaneous examination revealed multiple non follicular pustules of varying size ranging from 0.3 × 0.3 cm to 0.5 × 0.5 cm over an erythematous background present over lower part of bilateral legs, more on the anterior aspect (Figure 1). Bilateral inguinal and axillary region showed enlarged tender lymph nodes, 2-3 cm in size and firm in consistency (Figure 2). A provisional diagnosis of acute generalized exanthematous pustulosis was considered and a skin biopsy was taken from the lesion. Histopathological examination revealed epidermis with pustule filled with neutrophils, superficial and deep dermis showed granulomatous inflammation (Figure 3).
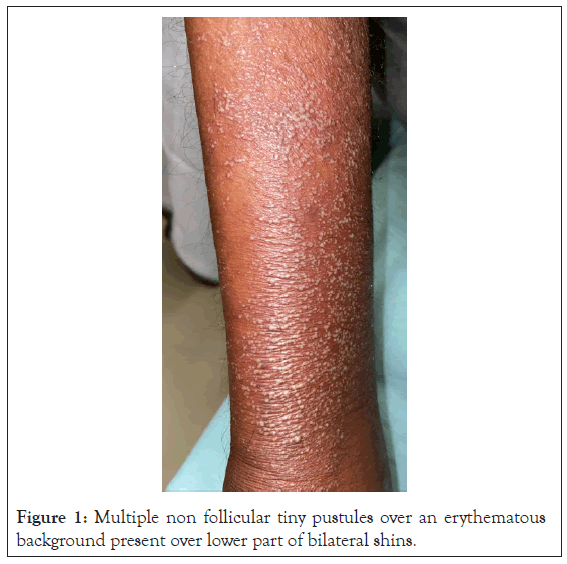
Figure 1: Multiple non follicular tiny pustules over an erythematous background present over lower part of bilateral shins.
Figure 2: Enlarged tender lymph nodes, 2-3 cm in size, firm in consistency over bilateral axilla.
Figure 3: Biopsy from pustule shows epidermis with pustule formation.
On further clinical examination, patient had thickening of bilateral ulnar nerve, right common peroneal nerve with no neuritis. On sensory examination, there was hypoesthesia over bilateral soles more on the lateral aspect. On reviewing, the biopsy specimen showed edematous superficial and deep dermis with interstitial, perivascular and periappendageal inflammatory infiltrate comprising foamy macrophages, lymphocytes and polymorphs (Figures 4 and 5). Fite stain for acid fast bacilli was positive and bacterial index was 5+ (Figure 6). Slit skin smear examination was also positive with Bacterial Index (BI) of 3+. FNAC from inguinal and axillary lymphnodes showed suppurative inflammation comprising of viable and degenerative neutrophils (Figure 7). Fite stain was also positive (Figure 8). Hence scrofuloderma was ruled out. Patient was diagnosed as a case of Hansen’s disease in type 2 reaction. He was started on Multi Bacillary Multi Drug Therapy (MBMDT) and systemic steroids. After three days of Intravenous (IV) Dexamethasone edema and erythema over the leg subsided with crusting of the pustules.
Figure 4: Dermis shows macrophage granulomas comprising of foamy macrophages, lymphocytes, polymorphs HE 40x.
Figure 5: Dermis shows macrophage granulomas comprising of foamy macrophages, lymphocytes, polymorphs HE 100x.
Figure 6: Many acid fast bacilli seen, BI 5 (fite oil immersion).
Figure 7: FNAC of lymph nodes showing necrosis with degenerated and viable inflammatory cells (wright giemsa stain 40x).
Figure 8: FNAC of lymph nodes showing multiple fragmented AFB [fite oil immersion].
The relatively uneventful typical chronic course of Hansen is interrupted by episodes of acute or subacute inflammation known as leprosy reactions which can happen prior to, during, or after the treatment course [1]. The two types of leprosy reactions are reversal reaction and erythema nodosum leprosum. Patients with Lepromatous Leprosy (LL) or Borderline Lepromatous (BL) frequently experience ENL [1]. ENL presents as evanescent erythematous tender nodules frequently [2]. Less commonly presents as pustules, vesicles, bullae, ulcerations, erythema multiforme-like lesions [2-4]. Apart from the pustular ENL described, which is often seen in the case of chronic EBL, or after administration of bactericidal drugs such as ofloxacin. In our case, the patient is de novo pustular eruption without evanescent erythematous nodule or introduction of the bactericidal drug. The possible pathogenesis of high bacillary load is implicated in the manifestation of pustular lesions. The presence of a high bacillary load in endothelial cells induces antiendothelial antibodies which play a major role in the formation and dissemination of ENL [5]. Our case presents with multiple crops of tiny nonfollicular pustular eruptions over the bilateral shin and axillary flexure after the introduction of ATT, associated with fever and elevated White Blood Count (WBCs) led to differentials of acute generalized exanthematous pustulosis, pustular ENL. AGEP is a severe cutaneous eruption with nonfollicular, sterile, pustules on an erythematous background associated with fever and leukocytosis [6-9].
In the vast majority of cases medications are implicated, few theories of infectious etiologies are also suspected. Previous case reports of infectious etiology such as coccidioidomycosis, chlamydia, cytomegalovirus, and parvovirus have been described. This may implicate AGEP-like eruptions is also a rare presentation of Hansen’s reaction. Pustular lesion in ENL is an uncommon form of ENL and is criteria for severe ENL. This case highlights the need for thorough clinical examination and histopathological correlation for diagnosing the new facets of Hansen’s disease.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Shreya K, Lakshman AM, Asati DP, Goel G (2023) Hansen’s Reaction Presenting as Acute Generalized Exanthematous Pustulosis-A New Facet to an Old Disease. Mycobact Dis. 13:332.
Received: 01-Mar-2023, Manuscript No. MDTL-23-22088; Editor assigned: 03-Mar-2023, Pre QC No. MDTL-23-22088 (PQ); Reviewed: 17-Mar-2023, QC No. MDTL-23-22088; Revised: 24-Mar-2023, Manuscript No. MDTL-23-22088 (R); Published: 31-Mar-2023 , DOI: 10.35248/2161-1068.23.13.332
Copyright: © 2023 Shreya K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.