Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2024)Volume 15, Issue 1
Purpose: To assess the efficacy and safety of Gonioscopy Assisted Transluminal Trabeculotomy (GATT) in the treatment of glaucomatocyclitic crisis (Posner-Schlossman syndrome).
Materials and methods: We retrospectively reviewed six patients diagnosed with glaucomatocyclitic crisis and uncontrolled Intraocular Pressure (IOP) who underwent Gonioscopy Assisted Transluminal Trabeculotomy (GATT). ALL the patients were followed-up for 12 months after the surgery. Clinical outcome measurements included visual acuity, intraocular pressure, complications and relapses.
Results: Mean IOP before GATT was 31.17 mmHg ± 7.08 mmHg (range 23 mmHg-41 mmHg). The mean number of anti-glaucoma medication prior to surgery was 2.50 ± 0.55. By the last follow-up, IOP in 5 patients was reduced to normal level (15.40 mmHg ± 2.97 mmHg) and their anti-glaucoma medication was decreased prominently to 0.80 ± 0.84. Only 1 of the patients with a 30-year history of Posner-Schlossman Syndrome (PSS) underwent trabeculectomy at 8 months after GATT. The mean percentage of IOP decrease in 5 patients at 12 months was 44.29%. Recurring attack of glaucomatocyclitic crisis occurred in 3 patients during the follow-up period; nonetheless the peak IOP and the duration of the Elevated Intraocular Pressure (EIOP) were reduced after the surgery.
Conclusion: GATT seems to be a reliable and effective method for the management of glaucomatocyclitic crisis with uncontrolled IOP. Although it may not prevent relapses of glaucomatocyclitic crisis, there is a chance that it may lower the peak IOP and the duration of the EIOP in the relapse.
Intraocular presssure; Glaucomatocyclitic crisis; Anti-glaucoma
Posner Schlossman Syndrome (PSS), also known as glaucomatocyclitic crisis, was first published by Posner, et al. [1] it is a unilateral ocular disease characterized by recurrent episodes of acute non-granulomatous anterior uveitis and increased Intraocular Pressure (IOP) [1]. The condition tends to affect young man between 20 and 50 years of age. It usually causes only minor eye discomfort, accompanied by a few fine white Keratic Precipitates (KP) and mild anterior chamber inflammation. The IOP will be elevated to as high as 40 mmHg-60 mmHg during an attack; gonioscopy will show an open angle. PSS is usually selflimited and lasts for days to weeks. Treatment of PSS is aimed at IOP and intraocular inflammation reduction. Recent reports have shown that Cytomegalovirus (CMV) plays a pathogenic role in some PSS patients [2-5].
Although PSS is believed to be benign at first, long-term research shows that repeated attacks might lead to secondary glaucomatous optic nerve changes. An elevation of IOP caused by some episodic changes in the trabecular meshwork and reduced outflow of aqueous humor may occur during the intermission stage, accompanied by permanent glaucomatous damage and loss of corneal endothelial cell [6,7]. In order to prevent further optic nerve damage and visual field defect, surgical interventions should be selected when there is uncontrolled IOP. The purpose of this report is to examine the efficacy and safety of GATT in a series of patients diagnosed with glaucomatocyclitic crisis and uncontrolled IOP.
This study was a retrospective case-series analysis of 6 patients (3 females and 3 males) diagnosed with PSS and uncontrolled IOP at Chengdu First People’s Hospital, who underwent Gonioscopy Assisted Transluminal Trabeculotomy (GATT) between 2018 and 2021. Table 1 describes the gender, mean age, preoperative IOP, number of anti-glaucoma medications, cup/disc ratio, preoperative best-corrected visual acuity and mean history of PSS. 2 of the patients had trabeculectomy before, all the patients were followed by (11.3 ± 1.6) month (Table 1).
| Patient/eye | Age | Gender | History of PSS (years) | Pre-operative | Pre-operative IOP (mmHg) | Pre-operative | Cup/disc ratio | Follow up duration | Prior procedure |
|---|---|---|---|---|---|---|---|---|---|
| 1/OD | 55 | Female | 30 | 3 | 41 | 0.7 | 0.6 | 12 | - |
| 2/OS | 36 | Female | 4 | 3 | 30 | 1 | 0.5 | 12 | - |
| 3/OS | 28 | Male | 4 | 2 | 38 | 1 | 0.5 | 12 | - |
| 4/OD | 65 | Male | 2 | 3 | 30 | 1 | 0.7 | 8 | - |
| 5/OD | 67 | Female | 3 | 2 | 23 | 0.5 | 0.4 | 12 | Trabeculectomy |
| 6/OS | 46 | Male | 6 | 2 | 25 | 0.9 | 0.7 | 12 | Trabeculectomy |
Note: PSS: Posner-Schlossman Syndrome; IOP: Intraocular Pressure; OD: Oculus Dexter; OS: Oculus Sinister
Table 1: Preoperative characteristics of patients.
All the patients fulfilled the following selection criteria:
• Mild recurrent episodes of acute non-granulomatous anterior uveitis.
• The IOP elevated to 40 mmHg-60 mmHg during an attack.
• Only minor eye discomfort, no nausea, vomiting or headache.
• Accompanied by a few fine white KP.
• Gonioscopy showed an open angle.
• Accompanied by permanent and progressive glaucomatous damage after recurrent attack or with uncontrolled IOP even though there is no glaucomatous damage.
Surgical procedure
Topical proparacaine 0.5% was applied preoperatively and standard sterile preparations were performed. An inferior temporal and a superior nasal limbal paracentesis were created by a 15° microsurgery knife. After making a 1.8 mm incision in the superior temporal cornea, the anterior chamber was anesthetized using 1% lidocaine. An Anterior Chamber (AC) tap was performed for analyzing CMV and Herpes Simplex Virus (HSV) in 3 patients with their permission. After injecting an miotic agent (carbachol 0.005%), the anterior chamber was filled with a viscoelastic agent (sodium hyaluronate). A surgical gonioscope was used to observe the Trabecular Meshwork (TM). Schlemm’s canal was incised by 2 mm on the nasal side using a microsurgical blade. The tip of a micro-catheter or a 5-0 nylon suture was placed into the anterior chamber through the limbal incision. The viscoelastic agent was used to expand the incision at Schlemm’s canal. The rounded tip of a micro-catheter or a 5-0 nylon suture was then inserted into Schlemm’s canal using a 23-gauge forceps, advanced through the canal circumferentially 360°. The tip was pulled out through the same opening. The same forceps were then used to make a 360-degree incision in Schlemm’s canal. The viscoelastic and the blood were removed from the anterior chamber. Postoperatively, oral Callicarpa nudiflora were prescribed for 3 days, topical steroid eye drops (prednisolone acetate) were prescribed 4 times daily for a week and then tapered over to 2 times daily for a week. Topical antibiotic (levofloxacin) was used 4 times daily for 2 weeks; non-steroid anti-inflammatory drug was used 4 times daily for 3 months. To prevent peripheral anterior synechia, pilocarpine 2% was used 3 times daily for 3 months when there is no active bleeding. Topical Ganciclovir gel was applied four times daily for 6 weeks to prevent relapses.
Postoperative follow-up
Clinical information was collected for the postoperative visits such as 1 day, 1 week, 1 month, 3 months, 6 months and 1 year. At each follow-up visit, the data collected was visual acuity, IOP, number of glaucoma medications, gonioscopic findings, complications and relapses. Effect judgements such as complete success i.e., IOP under 21 mmHg without any postoperative use of anti-glaucoma medication, qualified success i.e., IOP under 21 mmHg with anti-glaucoma medications, failure i.e., need for repeated surgery for glaucoma, persistent elevated IOP over 21 mmHg despite medical therapy, or persistent hypotony (IOP<5 mmHg).
Statistical methods
Clinical data was analyzed by SPSS 26.0 software, comparison of pre and post-operative IOP, medication number, visual acuity were performed using a Wilcoxon signed-rank test, a p-value of <0.05 was considered to be statistically significant.
4 of 6 patients underwent GATT with micro-catheters, 2 of them used 5-0 nylon sutures, and all procedures were performed by a single surgeon.
6 patients showed a mean IOP of (31.17 mmHg ± 7.08 mmHg), the mean IOP decreased to 16.00 mmHg (SD, 3.10 mmHg) on day 1, the average percent lowering of IOP was 44.80% (SD, 22.02%), P<0.05. The mean IOP was reduced to 19.50 mmHg ± 5.00 mmHg (37.17% ± 15.63% reduction) at 1 week, P<0.05, 2 patients showed increased IOP of 23 mmHg and 31 mmHg respectively and the IOP decreased to the normal range in 1 week with use of anti-glaucoma medications. At 1 month, the mean IOP was reduced to 14.67 mmHg ± 2.61 mmHg (50.86% ± 13.32% reduction), P<0.05. The percent reductions in IOP at 3 and 6 months were 40.22% (SD, 24.25%) and 40.62% (SD, 19.54%) respectively. 1 patient had a relapse and the IOP elevated to 32 mmHg with use of 2 anti-glaucoma medications at 8 weeks, accompanied by progressive optic nerve damage and visual field defect, therefore a trabeculectomy was then required to control IOP. Only 5 patients underwent 1 year follow-up, the mean IOP decreased to 15.40 mmHg (SD, 2.97 mmHg) at 1 year, the average percent lowering of IOP was 46.29% (SD, 20.40%), P<0.05. Figure 1 and Table 2 shows that mean IOP significantly decreased during the entire follow-up period (Figure 1 and Table 2).
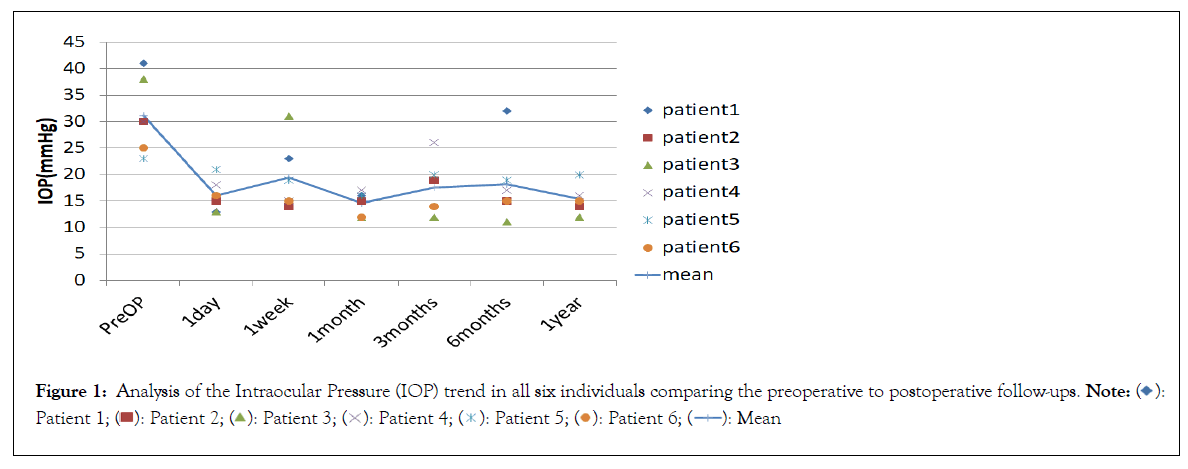
Figure 1: Analysis of the Intraocular Pressure (IOP) trend in all six individuals comparing the preoperative to postoperative follow-ups. 

| Time after surgery | IOP (mmHg) | Reduction from baseline(%) | P-value | Eyes (n) |
|---|---|---|---|---|
| D1 | 16.00 ± 3.10 | 44.80 ± 22.02 | 0.028 | 6 |
| W1 | 19.50 ± 5.00 | 37.17 ± 15.63 | 0.028 | 6 |
| M1 | 14.67 ± 2.61 | 50.86 ± 13.32 | 0.027 | 6 |
| M3 | 17.50 ± 5.21 | 40.22 ± 24.25 | 0.027 | 6 |
| M6 | 18.17 ± 7.28 | 40.62 ± 19.54 | 0.028 | 6 |
| Y1 | 15.40 ± 2.97 | 44.29 ± 20.40 | 0.043 | 5 |
Note: IOP: Intraocular Pressure; P-value is compared with preoperative IOP using the Wilcoxon signed-rank test
Table 2: Course of IOP and reduction of IOP from baseline.
Every patient had used 2 or 3 anti-glaucoma medications preoperatively, the average number was 2.50 ± 0.55. At 1 year, it decreased prominently to 0.80 ± 0.84, although the difference fell short of statistical significance. 2 of the patients achieved complete success, 2 of the patients who had uncontrolled IOP after trabeculectomy, both achieved qualified success after GATT. There was no significant difference in visual acuity or cup/disc ratio compared with those before surgery, P>0.05 as shown in Table 3. A patient with a 30-year history of PSS had uncontrolled IOP of 32 mmHg with maximal medical therapy at 8 months, accompanied by progressive optic nerve damage and visual field defect, gonioscopy revealed focal Peripheral Anterior Synechiae (PAS) and pigmentation at the cleaved trabecular. Therefore, a trabeculectomy was performed to control IOP. The complete and the qualified success rate were 33.3% and 83.33% respectively at last follow up (Table 3).
| Characteristics | Pre-operation | The last follow-up | P-value | Eyes (n) |
|---|---|---|---|---|
| Anti-glaucoma medications (n) | 2.50 ± 0.55 | 0.80 ± 0.84 | 0.066 | 5 |
| Mean best-corrected visual acuity (logMAR) | 0.08 ± 0.12 | 0.04 ± 0.11 | 0.581 | 5 |
| Mean cup/disc ratio | 0.57 ± 0.1 | 0.62 ± 0.19 | 0.18 | 5 |
Note: P-value compared with preoperative number of anti-glaucoma medications using Wilcoxon signed-rank test
Table 3: Number of anti-glaucoma medications, mean best-corrected visual acuity and mean cup/disc ratio after surgery.
Table 4 represents the intraoperative and postoperative complications. The most common complication was intraoperative anterior chamber blood reflux, which occurred in 5 eyes (83%). Transient hyphema occurred in 2 eyes (33.3%) postoperatively, all hemorrhages were resolved within 1 week. IOP spikes were seen in 2 eyes (33.3%) but administration of antiglaucoma medications reduced IOP to normal within 1 week. No incidences of hypotony, shallow anterior chamber, choroidal detachment, infection were noted (Table 4).
| Complications | Patients, n (%) |
|---|---|
| Intraoperative | |
| Anterior chamber blood reflux | 5(83.0%) |
| Anterior chamber flattening | 0 |
| Descemet’s membrane detachment | 0 |
| Cyclodialysis | 0 |
| Postoperative | |
| Transient hyphema | 2(33.3%) |
| Intraocular pressure spike (>20 mmHg) | 2(33.3%) |
| Hypotony (<5 mmHg) | 0 |
| Shallow anterior chamber | 0 |
| Choroidal detachment | 0 |
| Infection | 0 |
| Procedure failure | 1(16.67%) |
Table 4: Intraoperative and postoperative complications with the 360° suture trabeculotomy ab interno procedure.
At last follow-up, relapses were noted in 3 eyes. The preoperative and postoperative frequency showed no significant differences. Nonetheless all the peak IOP were reduced after the surgery and the peak IOP decreased by 20% from the pre-operation in 2 eyes. 3 patients who had relapse showed reduction of duration of Elevated Intraocular Pressure (EIOP) after the surgery. Among the 3 patients who had Polymerase Chain Reaction (PCR) examination of aqueous humor samples, 1 patient was positive for HSV and had relapse after surgery. The peak IOP and duration of EIOP slightly decreased while the frequency showed no obvious difference (Table 5).
| Patient | Pre-operative frequency (relapses per year) | Pre-operative peak IOP(mmHg) | Pre-operative duration of EIOP(days) | Post-operative frequency (relapses per year) | Post-operative peak IOP(mmHg) | Post-operative duration of EIOP(days) | PCR |
|---|---|---|---|---|---|---|---|
| 1 | 3 | 42 | 7 | - | - | - | - |
| 2 | 3.4 | 48 | 7-8 | 3 | 38 | 3 | - |
| 3 | 4 | 38 | 7-8 | 4 | 29 | 3 | - |
| 4 | 2 | 43 | 5 | - | - | - | - |
| 5 | 4 | 58 | 15 | 4.8 | 45 | 7 | HSV(+) |
| 6 | 2 | 39 | 7-8 | - | - | - | - |
Note: IOP: Intraocular Pressure; EIOP: Elevated Intraocular Pressure; PCR: Polymerase Chain Reaction; HSV: Herpes Simplex Virus
Table 5: The frequency, the duration and the peak IOP of PSS attack and PCR results.
The mechanisms of increased intraocular pressure of PSS is still not clear, it was referred that increased production of aqueous humor and reduced coefficient of outflow facility might play an important role. Animal experiment has shown that prostaglandins can induce elevated intraocular pressure. The content of prostaglandin in aqueous humor increases during PSS attack. Meanwhile the vasodilatation of Prostaglandin (PG) may lead to an increase in permeability of blood-aqueous barrier, thereby increasing the aqueous humor resulting from ultrafiltration and diffusion [8]. On the other hand, increased PG inhibits the release of Noradrenaline (NE) from sympathetic nerve, therefore antagonize the biological effects of NE directly. NE is an important medium for regulating the outflow of aqueous humor. The loss of regulation of trabecular meshwork leads to decreased coefficient of outflow facility and increased IOP. In addition, previous study showed that the inflammatory cell, protein and inflammation mediator like cytokines in the aqueous humor could lead to obstruction of aqueous outflow, trabecular meshwork edema may also play a role in IOP elevation in PSS [9,10].
Maruyama, et al. [11] reported a retrospective case-series analysis of 17 patients diagnosed with PSS, who underwent trabeculectomy to control IOP. This study found that PSS patients with a higher IOP and progressive visual field defects required glaucoma surgery more often, these characteristics might indicate a need for surgery. Trabeculectomy is considered to be an effective treatment for uveitic glaucoma [12].
Not only does it decrease IOP, but it also reduces inflammation of uveitis, because it can drain the anterior chamber inflammatory mediator to the filtering bleb, thereby reducing the severity of uveitis attack [13,14]. Jap, et al. [6] performed trabeculectomy surgery in 9 PSS patients with uncontrolled IOP and progressive visual field defect; they used antimetabolite in the surgery to improve the success rate, the IOP decreased significantly after surgery at 37 months (6 mmHg ~ 15 mmHg). 9 patients reported at least 3-4 recurrence per year before surgery, 6 of them had no recurrence at first year, 2 patients had 1 recurrence, a patient developed failure filtering bleb and progressive visual field defects after 15 recurrences. Therefore, although trabeculectomy is effective, postoperative complications associated with filtering procedures such as hypotony, wound leak, flat anterior chamber, choroidal effusion may occur [15]. In addition, the sub-conjunctival fibroblasts, lymphocytes and macrophages in patients with PSS may increase the risk of scarring of the filtering channel and lead to surgical failure [16]. Trabeculectomy with Mitomycin C (MMC) was less effective in maintaining intraocular pressure reduction in Uveitic Glaucoma (UG) eyes including PSS than in Primary Open Angle Glaucoma (POAG) eyes.
The loss of regulation of trabecular meshwork in PSS patient may lead to decreased coefficient of outflow facility and increased intraocular pressure, theoretically, reducing the outflow resistance of aqueous humor at the trabecular meshwork can achieve the purpose of decreasing intraocular pressure. Murata, et al. [17] performed surgery in a PSS cohort (10 trabeculectomy, 4 trabeculotomy) with uncontrolled IOP, the IOP after surgery showed no significant difference between the 2 groups. However, the success rate of trabeculectomy was 90% (9/10), the success rate of trabeculotomy was 75% (3/4). There were 4 patients who underwent trabeculectomy had relapse, while 1 patient had relapse in trabeculotomy group during the following period. Pahlitzsch, et al. [18] retrospective analysed 7 patients who underwent 120° trabectome. After 1 year of follow-up, IOP in all patients was reduced to normal level; the mean number of medication was reduced to 0.8 ± 1.1 from 3.1 ± 0.4 prior to the surgery. No recurring attack of glaucomatocyclitic crisis occurred. Hence, trabeculotomy and trabectome can also reduce IOP effectively, with a low rate of bleb-related complications such as hypotony, wound leak, flat anterior chamber, scar formation, while maintaining more ocular surface structure and function.
Gonioscopy Assisted Transluminal Trabeculotomy (GATT) is a kind of Micro-Invasive Glaucoma Surgery (MIGS). So far as we know, there were few reports about GATT in the management of PSS with uncontrolled IOP previously. In our study, we performed circumferential trabeculotomy to reduce the outflow resistance of aqueous humor at the Schlemm’s canal and trabecular meshwork on a greater scale, to increase outflow facility along the natural pathway. Not only it retains the advantages of trabeculotomy compared with trabeculectomy, but also it can reduce IOP more effectively. Our results showed that the percent lowering of IOP of 5 patients was 20%-60%, the number of anti-glaucoma medications decreased prominently after surgery. There were 2 patients who had underwent trabeculectomy before, developed elevated IOP due to scar formation of the flitering bleb, the IOP was reduced to normal level after circumferential trabeculotomy. The qualified success rate was 83.33% at last follow up. Although intraoperative anterior chamber blood reflux was a common occurrence, all hemorrhages were resolved within 1 week. The postoperative complications typically associated with filtering procedures were not reported. GATT seems to be a safe and effective for the management of glaucomatocyclitic crisis with uncontrolled IOP. 1 patient with a 30-year history of PSS had an elevated IOP and focal PAS in gonioscopy, needed a surgical intervention at 8 months. Therefore, the course of the disease and postoperative inflammatory reaction may be the key factors of the surgical effect.
It was referred that the use of antivirals in patients with PSS has been shown to be effective in reducing relapse and the risk of glaucomatous damage and Corneal Endothelial Cell (CEC) loss [19,20]. In our study, topical ganciclovir gel was applied four times daily for 6 weeks, 3 patients had relapse at 1 year after surgery. A reduction of peak IOP and duration of EIOP was noted. Ye, et al. [21] reported that the mean peak IOP during attacks and episodes in patients with PSS were decreased after penetrating canaloplasty. It can be assumed that the effect of lowering peak IOP during the attack can be achieved by increasing the outflow of aqueous humor after circumferential trabeculotomy. Besides, the outflow of inflammatory mediator including prostaglandin increased after GATT, the effect of prostaglandin and other inflammatory mediators on aqueous humor production and coefficient of outflow facility were reduced, making IOP easier to be controlled. Because of our small sample size, only 1 patient was positive for HSV and post-operative frequency showed no obvious difference. The cases are still being followed up and more research is needed to confirm the theory.
In conclusion, our study shows that GATT should be a safe and effective method for the management of glaucomatocyclitic crisis with uncontrolled IOP. However, our study had some inevitable limitations due to the small sample size and the retrospective design. On the other hand, there were few reports about GATT in the management of PSS with uncontrolled IOP previously. More observation of clinical effect and summary require further investigation.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Jing L, He Y, Fan H, Wang S, Xin M, Zheng LZ (2024) Gonioscopy Assisted Transluminal Trabeculotomy in the Management of Posner-Schlossman Syndrome. J Clin Exp Ophthalmol. 15:969.
Received: 29-Dec-2023, Manuscript No. JCEO-23-26533; Editor assigned: 01-Jan-2024, Pre QC No. JCEO-23-26533 (PQ); Reviewed: 15-Jan-2024, QC No. JCEO-23-26533; Revised: 22-Jan-2024, Manuscript No. JCEO-23-26533 (R); Published: 29-Jan-2024 , DOI: 10.35248/2155-9570.24.15.969
Copyright: © 2024 Jing L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.