Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Case Report - (2023)Volume 13, Issue 3
Non cardiogenic non renal flash pulmonary edema is a dramatic form of acute heart failure syndrome with rapid progression of symptoms giving the emergency physicians a narrow time window (few minutes to hours) to intervene and improve patient outcome. The spectrum of patients presenting is wide, ranging from mild pulmonary edema to respiratory failure. Due to the central role of increased sympathetic activity in the pathophysiology of this subset of patients, SCAPE (Sympathetic Crashing Acute Pulmonary Edema) is a better terminology. Early identification and prompt management helps decrease morbidity and mortality. Use of early Noninvasive Ventilation (NIV) after rapid screening for contraindications, diuretics and fluid restriction forms the basis of management of these patients. Three of the patients were successfully discharged from the hospital.
SCAPE; Negative pressure pulmonary edema; Diuretics; Non-invasive ventilation; Flash pulmonary edema
Acute severe respiratory distress with or without hemodynamic instability is an often-seen presentation in any emergency department. The most commonly seen cases secondary to a cardiac etiology are often readily diagnosed based on clinical history and presentation. The not so common cause of Flash Pulmonary Edema (FPE), secondary to renal artery stenosis, is also now being increasingly recognized since the initial description [1].
Other rarer cause of flash pulmonary edema, with diverse etiology-neurogenic upper airway obstruction anaphylaxis, amniotic fluid embolism, swimming and scuba diving exertion in cold environmental and sexual intercourse etc. have been described in literature, generally as case reports. We present 4 unusual cases of non-cardiogenic, flash pulmonary edema, presenting to our ED over the last 1 year and review pertinent literature. The need for high index of suspicion and correct diagnosis and prompt treatment in these rare scenarios of FPE, is mandatory for good patient outcome [2].
Case 1
A 2-year-old male baby presented to the ER in a comatose state with rapid, shallow breathing. There was a history of fall of wooden plank over child’s head 1 hour prior to admission and 2 episodes of vomiting. On admission GCS was 5 (E1V2M2), pupils were bilateral equal and reacting. Airway was compromised with pooling of secretions in the oral cavity with bilateral rales on auscultation. He had an SPO2 of 86 at room air, HR-114 bpm, Feeble pulse and BP-70/40 mmHg. His ABG revealed respiratory acidosis and ECG showed ST elevations in leads V4-V6. He was intubated in view of low GCS and threatened airway, that revealed frothy secretions. Bedside USG revealed no evidence of cardiac or abdominal injury. Chest x-ray revealed bilateral congested lung fields suggestive of pulmonary edema and bedside 2D Echocardiography revealed dilated left atria and left ventricle with LV global hypokinesia, ejection fraction of 15%. Troponin I and CKMB were within normal limits. Patient could not be shifted for CT head because of persistent hypotension despite increasing vasopressor treatment with noradrenaline and dopamine. He was revived from 2 episodes of cardiac arrest but succumbed to third episode despite all resuscitative measures, 6 hours post presentation. Autopsy revealed extensive SAH with occipital bone fracture. There was no evidence of any cardiac congenital anomaly or heart disease (Figures 1 and 2) [3].
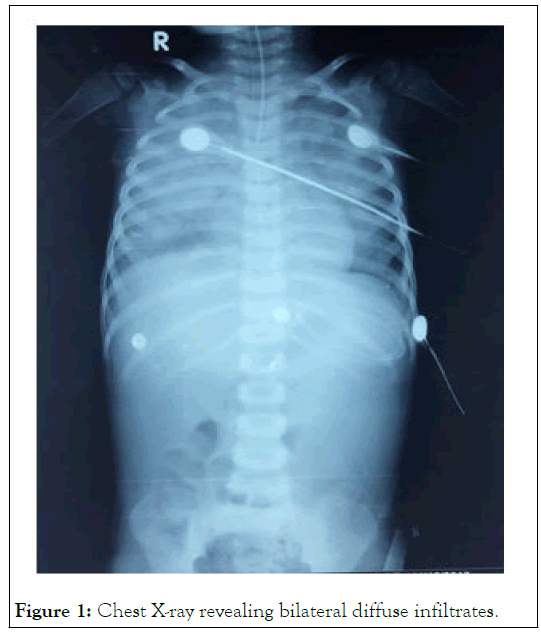
Figure 1: Chest X-ray revealing bilateral diffuse infiltrates.
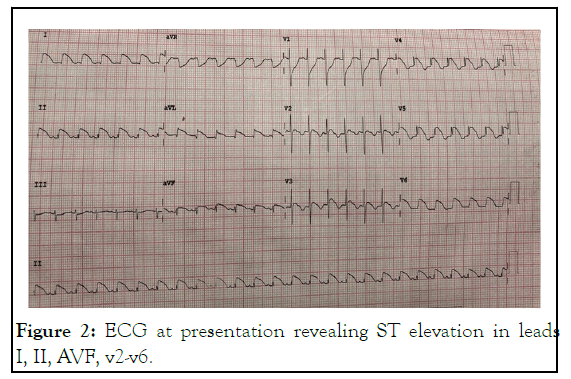
Figure 2: ECG at presentation revealing ST elevation in leads I, II, AVF, v2-v6.
Case 2
A 60 yr old male, known case of obstructive airway disease presented to ER with worsening shortness of breath since 1 day (mMRC-4). No other known co-morbidities. His weight was 65 kg, height 5’10, BP of 130/70 mmHg, HR-100 bpm, RR-40 cpm, maintaining a room air saturation of 64%. His chest x-ray revealed bilateral hyperinflated lung fields and his ECG, 2D Echo and lung USG were unremarkable. ABG revealed (pH-6.935 pCO2 160, pO2 41.1, SaO2 43.3, HCO3 32.2 and lactates-1.9). Patient was placed on NIV-BiPAP mode. Due to worsening of respiratory distress after 15 min of NIV; he was intubated with IV Midazolam 5 mg, Ketamine 50g and succinylcholine 75 mg [4].
Following intubation, white frothy sections were noted in ETT and extensive B/L rales were heard over chest. Repeat chest x-ray was suggestive of frank bilateral pulmonary edema. Patient was put on Mechanical ventilation PSIMV requiring initial PEEP of 15 and PC of 24-26 to generate Tidal volumes of 350 ml which was eventually tapered. He was managed on IV diuretics and positive pressure ventilation. He was eventually weaned off ventilator and discharged (Figure 3) [5].
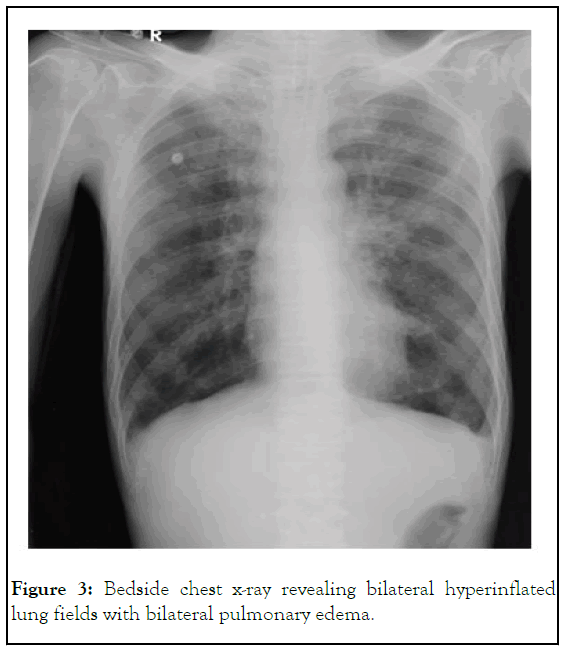
Figure 3: Bedside chest x-ray revealing bilateral hyperinflated lung fields with bilateral pulmonary edema.
Case 3
A 25 yr old male was brought to the ER with alleged history of hanging using a saree (approximately 5-meter-long cotton cloth). He appeared in respiratory distress-RR: 26 cpm and had a SPO2 of 89% at room air, auscultation revealed bilateral rales and had a BP: 100/60 mmHg. He was intubated in view of compromised airway and put on PSIMV mode of mechanical ventilation. Pink frothy sputum was sucked immediately post intubation. His CT brain and cervical spine were normal. He was managed with diuretics and ventilation. His rales cleared; lung fields ventilated equally.8 hours post ventilation ABG was normal. He was gradually weaned off, extubated and discharged [6].
Case 4
A 37-year-old female presented in altered mentation in near respiratory arrest to the ER. She was immediately intubated and placed on PSIMV mode of mechanical ventilation with PEEP of 5. Her BP and pulse stabilized. Her chest X-ray revealed bilateral haziness and bedside USG showed B-lines. Her ECG and Echo did not show any abnormality. A USG abdomen and pelvis were done with ruled out renal artery stenosis. Her urine for metanephrines was negative and cardiac enzymes were within normal limits. Later a detailed history from husband revealed recurrent episodes of transient syncope and tachycardia during coitus on multiple events. On this occasion it was more severe with a syncopal attack followed by sudden respiratory distress. Choking/Strangulation, history of inhaled toxins or drug intake, were ruled out. She was managed with diuretic infusion and positive pressure ventilation and extubated next morning [7].
Flash Pulmonary Edema (FPE) describes a state of sudden, dramatic and precipitous form of acute decompensated heart failure. Irrespective of the etiology or the precipitating cause, sudden increase in left ventricular end diastolic pressure is the final denominator for development of pulmonary edema. Cardiogenic pulmonary edema is also a result of acute decompensated heart failure. Hypertension, coronary ischemia and valvular heart disease are well known to cause acute decompensation and pulmonary edema [8].
Acute non-cardiogenic pulmonary edema developing in patients without any underlying cardiac abnormality has been reported in variety of dissimilar conditions including- upper airway obstruction, anaphylaxis, fluid maldistribution, severe CNS trauma or SAH and other acute CNS conditions, drugs, extreme emotional stress, swimming, scuba diving and sexual intercourse. Also described is a fulminant, hyperacute flash pulmonary edema in hypertensive heart failure presenting always with high systolic blood pressure and has aptly been called sympathetic crashing acute pulmonary. Neurogenic Pulmonary Edema (NPE), as seen in case 1 of our series is a poorly understood and relatively rare condition following a critically ill neurological ailment. NPE has been described in a host of conditions including severe traumatic brain injury SAH, meningitis, status epilepticus stroke, acute hydrocephalus etc [9].
The clinical presentation may range from subclinical to fulminant flash pulmonary edema. Classical and severe NPE is associated with severe brain damage and presents with clinical and radiological pulmonary congestion prink frothy sputum and often death despite all treatment. Patients may have tachycardia, dyspnea, reduced O2 saturation, severe hypertension or sometimes hypotension. NPE may be associated with stunned myocardial syndrome characterized by hypotension, myocardial failure with ECG and enzyme changes that may resemble acute coronary disease, as probably present in our case too [10].
Any neurological condition leading to acute profound increase in Intracranial Pressure (ICP), appear to be at the greatest risk of developing NPE This may be directly due to increased sympathetic activity or due to release of other neurohumoral factors such as neuropeptide Y, inflammatory mediators, cytokines, fibrin and fibrin degradation products etc. However, the final mechanism that causes changes at the pulmonary vascular endothelium remains unresolved. The postulated mechanism included changes that increase the hydrostatic pulmonary pressure (The blast theory), increased pulmonary capillary permeability (Permeable defect theory) and neurocardiac or neurodynamic mechanism. Although hydrostatic pressure plays an important role in the pathogenesis the presence of RBCS and protein in the alveolar fluid in patients with NPE is inexplicable with this theory.
Theodore and Robin postulated the ‘blast theory’ of NPE, in 1976. The Blast theory postulates that the abrupt increase in the systemic and pulmonary pressures due to a marked sudden catecholamine surge results in shift of blood from systemic to pulmonary circulation, leading to development of transudative pulmonary edema. This theory also further postulated that this acute rise in capillary pressure induces a degree of barotrauma that could damage the capillary alveolar membrane. This damage would lead to vascular leak and protein rich pulmonary fluid edema. The other mechanism of NPE proposed that, an acute CNS injury directly affect the pulmonary vascular bed with edema developing regardless of any systemic circulatory changes. This may be due to directly increased sympathetic activity or secondary to release of other neurohormonal mediators such as neuropeptide, cytokines, fibrin and fibrin degradation products etc [11].
Although NPE is classified as a non-cardiogenic form of pulmonary edema, but in a subset of patients, severe neurological insult causes direct myocardial injury with resultant pulmonary edema.34 takotsubo or stress cardiomyopathy is characterized by depressed cardiac contractility following neurologically stressful event. This causes diastolic dysfunction and global hypokinesia of heart leading to pulmonary edema. Here also, massive sympathetic discharge is thought to induce direct myocyte injury [12].
In addition to the direct toxic effects on the myocardium, indirect cardiac effects have been postulated secondary to increase in systemic and pulmonary pressures. Sarnoff and Sarnoff called this as ‘neuro-hemodynamic pulmonary edema’. In their study, following the injection of fibrin in cisterna magna of dogs and rabbits, substantial increase in aortic and pulmonary pressures were recorded. They postulated that following the sympathetic surge, left ventricle reaches its work failure threshold and is unable to effectively pump against increased systemic pressure. Thus, a transfer of blood from high systemic resistance to low resistance pulmonary circulation ensues, leading to pulmonary edema [13].
In the absence of any definitive diagnostic criteria or proven treatment modalities, the management of NPE remains challenging. The treatment primarily involves hemodynamic and respiratory support, in addition to control of raised intracranial pressure. Loop diuretics, like furosemide, reduce sodium reabsorption and promote arterial venous dilatation, which may improve pulmonary congestion and relieve pulmonary circulation. Alpha-adrenergic blocking agents, which could potentially relieve hemodynamic instability and subsequent respiratory failure has shown promise in animal models, but only sporadic reports document its use in humans [14].
Negative Pressure Pulmonary Edema (NPPE), the possible cause in case 2 and 3 of our series, is an uncommon complication of anesthesia, usually resulting from laryngospasm, with a prevalence rate of around 0.1%. Because of obstruction, a large negative intrathoracic pressure is generated by the patients’ increased breathing effort. This negative pressure causes an increase in left ventricular preload and afterload, in addition to causing increased extramural hydrostatic pressure. This increased left heart load increases pulmonary capillary pressure causing fluids to move from capillary to lung interstitial. In addition, increased sympathetic stimulation leads to peripheral vasoconstriction, increasing left ventricular afterload. Apart from the pressure changes leading to edema formation, the other proposed mechanism involves the disruption of the alveolar membranes from severe mechanical stress [15].
The management of NPPE depends upon the severity of symptoms. Milder cases may recover with conservative treatment. However, severe cases may require temporary intubation and mechanical ventilation with PEEP, ensuring an SPO2 of >90%. Diuretics have been traditionally used but their use remains unproven and may even be deleterious. Whenever possible, non-invasive ventilation could be an alternative for ventilatory support. Nitrates have shown a beneficial effect by causing a decrease in afterload and leading to resolution of pulmonary edema. Studies reveal decreased rates of endotracheal intubation and ICU admissions in patients receiving high-dose NTG (nitroglycerine). Sexual intercourse inducing pulmonary edema, as in case 4 of our series, in otherwise normal individuals is yet another rare cause of FPE. The proposed mechanism again is probably increased sympathetic outburst, with hemodynamic and/or direct capillary permeability defect [16].
In addition to affecting apparently normal individuals, the clinician should be aware that sexual activity induced pulmonary edema could be the first symptoms of a silent/ asymptomatic mitral valve disease and coronary ischemia.
Anticipation and prompt diagnosis of SCAPE helps decrease morbidity and mortality. The mainstay of management is NIV and high-dose nitrate infusions within minutes of the patient's arrival to the ED. Neurogenic pulmonary edema is an underdiagnosed condition with patients often having multiple other comorbidities which may obscure or mimic its diagnosis. Use of high dose Nitrates over Furosemide has shown decreased rates of endotracheal intubation and ICU admissions.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Singh A (2023) Flash Pulmonary Odema-4 Rare Cases of Non-Cardiogenic, Non-Renal Etiology. Emergency Med. 13:285.
Received: 22-Mar-2020, Manuscript No. EGM-23-3702; Editor assigned: 27-Mar-2020, Pre QC No. EGM-23-3702(PQ); Reviewed: 10-Apr-2020, QC No. EGM-23-3702; Revised: 28-Apr-2023, Manuscript No. EGM-23-3702(R); Published: 26-May-2023 , DOI: 10.4172/2165-7548.23.13.285
Copyright: © 2023 Singh A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.