Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2023)Volume 14, Issue 6
Purpose: To verify the risk factors that influences the Intraocular Lens (IOL) dislocation.
Materials and methods: The time to of in-the-bag IOL (242 eyes) dislocation after the initial surgery was examined using patient characteristics and risk factors. The examined risk factors included 11 factors associated with underlying diseases (trauma, Pseudoexfoliation Syndrome (PE), atopic dermatitis, retinitis pigmentosa, glaucoma attack, glaucoma, short axial length, long axial length, uveitis, scleral buckling, post-pars plana vitrectomy) and two factors associated with the initial surgical findings (Zonular Weakness (ZW), posterior capsule rupture). In addition, the 242 eyes were classified into four groups (group A, PE+ ZW+; group B, PE- ZW+; group C, PE+ ZW-; group D, PE- ZW-) and the dislocation period was examined.
Results: The median patient age was 67 years and the median time to dislocation after the first cataract surgery was 120 months. Among the risk factors, PE and ZW were significantly associated with the time to dislocation (both p<0.05). In addition, the time to dislocation was significantly shorter in groups A (12.3 months) and B (83.6 months) than in group D (135.6 months; p<0.001 and p=0.007, respectively).
Conclusion: The presence of PE and/or ZW increases the risk of IOL dislocation. However, positivity for PE alone may be associated with a lower risk of IOL dislocation, indicating the need to assess ZW in the initial surgery.
Intraocular lens dislocation; Zonular weakness; Risk factors; Aspiration
With the progress of Phacoemulsification and Aspiration (PEA)+Intraocular Lens (IOL) insertion technology, IOL insertion has been actively performed in difficult and comorbid cases of cataract in recent years. However, IOL dislocation occurs over time in some patients, necessitating scleral-sutured ciliary sulcus fixation or intrascleral fixation. Therefore, clarifying the factors related to IOL dislocation is important for patient follow- up and the selection of the IOL fixation method at the time of the initial surgery.
Pseudoexfoliation Syndrome (PE), trauma, post Pars Plana Vitrectomy (PPV) and atopic dermatitis have been reported as risk factors for IOL dislocation [1-7]. However, few reports have examined the influence of various risk factors on the time to dislocation. Therefore, we examined the risk factors related to the time to IOL dislocation in numerous cases.
Case selection and exclusion criteria
We retrospectively examined the medical records of patients with IOL dislocation treated at Showa University East Hospital, Showa University Fujigaoka Hospital, Showa University Fujigaoka Rehabilitation Hospital, and Showa University Toyosu Hospital between February 2001 and September 2016. We limited the patients to those in whom the content of the first cataract surgery was clear.
The initial cataract surgery included all surgical procedures in which the IOL was inserted in a bag, such as PEA, Extracapsular Cataract Extraction (ECCE) and vitrectomy. Conversely, cases in which scleral-sutured ciliary sulcus fixation or intrascleral fixation of the IOL had been previously performed cases in which a capsular tension ring was inserted and cases in which the IOL was externally fixed in the capsular bag were excluded from the analysis. After applying the inclusion and exclusion criteria, 242 cases of IOL dislocation were extracted.
Patient background and risk factors
Information on the patients’ sex, age, risk factors, surgical findings and time to IOL dislocation after the initial surgery was collected retrospectively from the medical records. The following 11 items were collected as potential underlying diseases such as trauma, Pseudoexfoliation Syndrome (PE), atopic dermatitis, retinitis pigmentosa, glaucoma attack, glaucoma, short axial length (<22 mm), long axial length (>26 mm), uveitis, postoperative retinal detachment by scleral buckling surgery and PPV. In addition, rupture or vulnerability of the Zonule of Zinn during the initial surgery (Zonular Weakness (ZW)) and Posterior Capsule Rupture (PCR) were assessed as surgical findings.
Statistical analysis
Continuous variables were presented as the median (interquartile range) and categorical values were presented as n (%). Wilcoxon’s rank sum test or the Kruskal-Wallis test was performed to compare the time to dislocation according to risk factors.
To clarify the effects of PE and ZW on the duration of IOL dislocation, we divided into four groups such as group A, PE+ZW+ (n=6); group B, PE- ZW+ (n=28); group C, PE+ZW- (n=8); and group D, PE- ZW- (n=200). The Kruskal-Wallis test and Steel-Dwass multiple comparison test were performed to compare the time to dislocation in these four groups.
The level of significance was 5%, and JMP® 15 (SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses.
Patient characteristics
Table 1 presents the characteristics of the study cohort. The median patient age was 67 years and 179 of the examined eyes (74%) were in men. Meanwhile, the surgical site was the right eye in 138 cases (57%) and the left eye in 104 cases (43%). The initial cataract surgery was PEA+IOL insertion in 221 eyes (91%), ECCE+IOL insertion in 5 eyes (2%), PEA+IOL insertion+vitrectomy in 15 eyes (7%) and PEA+IOL+anterior vitrectomy in 1 eye (0.4%). Long axial length was the most common risk factor (97 eyes (40%)), followed by atopic dermatitis (40 eyes (17%)), ZW (34 eyes (14%)), glaucoma (31 eyes (13%)) and PPV (26 eyes (11%)). Conversely, 59 cases (24%) lacked risk factors (Table 1).
| Characteristics | Median(interquartile range) or n(%) |
|---|---|
| Age(years) | 67(55,77) |
| Gender | |
| Male | 179 (74%) |
| Female | 63(26%) |
| Operative eye | |
| Right | 138(57%) |
| Left | 104(43%) |
| Operative method | |
| PEA+IOL insertion | 221(91%) |
| ECCE+IOL insertion | 5(2%) |
| PEA+IOL insertion+vitrectomy | 15(7%) |
| PEA+IOL insertion+anterior vitrectomy | 1(0.4%) |
| Time to dislocation(months) | 120(69,180) |
| Risk factors | |
| Trauma | 20(8%) |
| PE | 14(6%) |
| Atopic dermatitis | 40(17%) |
| Retinitis pigmentosa | 5(2%) |
| Glaucoma attack | 3(1%) |
| Glaucoma | 31(13%) |
| Scleral buckling | 19(8%) |
| PPV | 26(11%) |
| Uveitis | 5(2%) |
| Long axial length | 97(40%) |
| Short axial length | 11(5%) |
| PCR | 11(5%) |
| ZW | 34(14%) |
Note: PEA: Phacoemulsification and Aspiration; IOL: Intraocular Lens; ECCE: Extracapsular Cataract Extraction; PE: Pseudoexfoliation Syndrome; PPV: Pars Plana Vitrectomy; PCR: Posterior Capsule Rupture; ZW: Zonular Weakness
Table 1: Patient characteristics (n=242).
Time to dislocation
The median time to dislocation after the initial surgery was 120 months and Figure 1 presents the median time to dislocation (months) by risk factor. The shortest time to dislocation were observed for glaucoma attack (65.3 months), uveitis (68 months), ZW (72.7 months), PE (84.3 months) and PCR (89.3 months) (Figure 1).
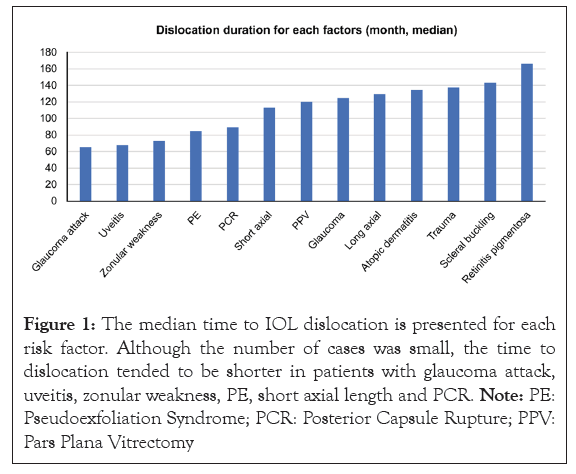
Figure 1: The median time to IOL dislocation is presented for each risk factor. Although the number of cases was small, the time to dislocation tended to be shorter in patients with glaucoma attack, uveitis, zonular weakness, PE, short axial length and PCR. Note: PE: Pseudoexfoliation Syndrome; PCR: Posterior Capsule Rupture; PPV: Pars Plana Vitrectomy
As presented in Table 2, the time to did not differ between men and women (115.2 months vs. 123.7 months, p=0.408), nor was a difference noted between left and right eyes (120 months vs. 122.6 months, p=0.77). In addition, the time to dislocation did not differ according to the surgical procedure (PEA+IOL insertion, 121.7 months; ECCE+IOL insertion, 162.4 months; PEA+IOL insertion+vitrectomy, 103 months; PEA+IOL insertion+anterior vitrectomy, 140 months; p=0.421). Only two risk factors, PE (p=0.041) and ZW (P<0.001), significantly altered the time to IOL dislocation (Table 2).
| Characteristics | Time to dislocation(months) | p |
|---|---|---|
| Gender(male vs. female) | 115.2 vs. 123.74 | 0.408 |
| Operative eye | ||
| Right | 120 | 0.77 |
| Left | 122.6 | |
| Operative method | - | 0.421 |
| PEA+IOL insertion | 121.7 | |
| ECCE+IOL insertion | 162.4 | |
| PEA+IOL insertion+vitrectomy | 103 | |
| PEA+IOL insertion+anterior vitrectomy | 140 | |
| Risk factors | ||
| Trauma (with vs. without) | 137.5 vs. 120.1 | 0.287 |
| PE | 84.3 vs. 123.8 | 0.041 |
| Atopic dermatitis | 134.6 vs. 118.9 | 0.194 |
| Retinitis pigmentosa | 166.1 vs. 120.6 | 0.151 |
| Glaucoma attack | 65.3 vs. 122.2 | 0.163 |
| Glaucoma | 124.4 vs. 121.1 | 0.807 |
| Scleral buckling | 143.4 vs. 119.6 | 0.155 |
| PPV | 120.5 vs. 121.6 | 0.937 |
| Uveitis | 68 vs. 122.6 | 0.085 |
| Long axial length | 129.5 vs. 116.2 | 0.147 |
| Short axial length | 113 vs. 121.9 | 0.682 |
| PCR | 89.3 vs. 123 | 0.118 |
| ZW | 72.7 vs. 129.5 | <0.0001 |
Note: PEA: Phacoemulsification and Aspiration; IOL: Intraocular Lens; ECCE: Extracapsular Cataract Extraction; PE: Pseudoexfoliation Syndrome; PPV: Pars Plana Vitrectomy; PCR: Posterior Capsule Rupture; ZW: Zonular Weakness
Table 2: Time to dislocation by patient characteristics and risk factors (n=242).
Regarding the influence of PE and ZW on the time to dislocation, the results illustrated that the time to dislocation was significantly shorter in groups A (12.3 months) and B (83.6 months) than in group D (135.6 months, p<0.001 and p=0.007, respectively) (Figure 2).
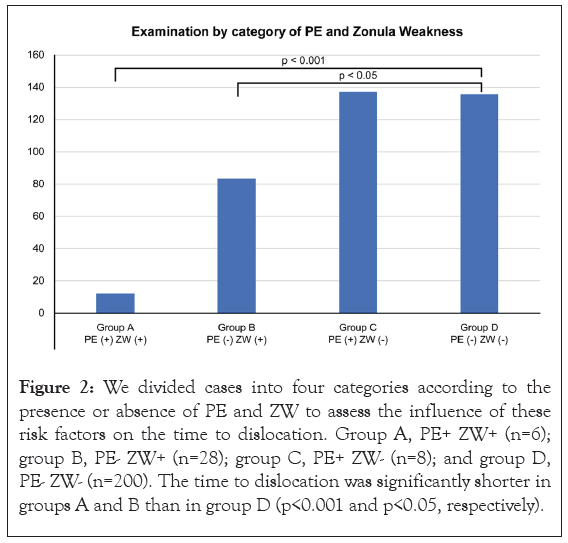
Figure 2: We divided cases into four categories according to the presence or absence of PE and ZW to assess the influence of these risk factors on the time to dislocation. Group A, PE+ ZW+ (n=6); group B, PE- ZW+ (n=28); group C, PE+ ZW- (n=8); and group D, PE- ZW- (n=200). The time to dislocation was significantly shorter in groups A and B than in group D (p<0.001 and p<0.05, respectively).
The frequency of IOL dislocation after cataract surgery ranges 0.098%-3% and the risk of dislocation increases over time after the initial surgery [8-11]. Various factors, such as age, comorbidities and other regional differences in patient background and the degree of burden on the Zonule of Zinn during surgery are related to the risk of IOL dislocation after cataract surgery. Previously reported risk factors for IOL dislocation included uveitis, ZW, PE, vitreous surgery, glaucoma, trauma and complications during the initial surgery. In total, 13 variables have been generally established as risk factors for IOL dislocation and clinical experience has further verified that ZW is likely to increase the risk of dislocation.
Although long axial length was the most common risk factor in our cohort, it was not associated with a longer duration of IOL dislocation than the other factors. Cataract surgery tends to occur at a younger age in patients with a long axial length and the postoperative course after the initial surgery is long, which could increase the risk of dislocation [12]. Additionally, atopic dermatitis, PPV, glaucoma and ZW were also frequently detected in our cohort, in line with previous observations.
Conversely, approximately one-fourth of the eyes in this study lacked risk factors. Similarly, Iwamoto reported that approximately 11% of cases of IOL dislocation do not involve a risk factor that causes ZW and it appears that some patients do not have a risk factor for IOL dislocation. Although the study cohort exhibited male predominance, the duration of dislocation and age did not differ by sex. It has been reported that men were more likely to experience IOL dislocation than women. However, women more frequently undergo cataract surgery than men and the prevalence of PE, which was identified as a strong risk factor in this study, is also higher in women [13,14]. Several reports have described PE as the most important risk factor for IOL dislocation [15]. This accords with clinical experience even though the risk of dislocation was apparently higher in patients with ZW in this study. Thus, further investigation is needed to clarify the reason for the higher prevalence of IOL dislocation in men.
In previous reports, the average time to dislocation after the first cataract surgery ranged 6 years, 67.8 months, 11.5 years and 8.5 years. The time to dislocation after the initial surgery was therefore in line with previous results.
Concerning risk factors, the time to IOL dislocation was shorter than the average in patients with glaucoma attack (65.3 months), uveitis (68 months), ZW (72.7 months), PE (84.3 months), PCR (89.3 months) and short axial length (113 months). Because risk factors can present simultaneously, the presence of these risk factors is believed to facilitate early dislocation. Although only PE and ZW were associated with significant differences in the duration of dislocation, only a few cases involved uveitis (n=5) and glaucoma attack (n=3) and thus, the results could change with the accrual of additional cases. The inability to compare the findings with a control group after normal cataract surgery without dislocation may have also affected the results of statistical analysis.
The present analysis further demonstrated that the presence of ZW, either alone or concomitantly with PE, shortened the time to IOL dislocation, whereas positivity for PE alone did not change the time to dislocation. Thus, it appears that ZW more strongly influences the risk of dislocation than PE. Meanwhile, although the time to dislocation was numerically shorter in group A than in group C (12.3 months vs. 137.1 months), statistical significance was not achieved, likely because of the small number of patients.
Several limitations of this study must be addressed. First, the degree of ZW during surgery was not uniform because it depends on the subjective evaluation of the operator and glaucoma is classified as an open angle or closed angle. It is not done, it is not classified according to the presence or absence of gas replacement during vitreous surgery, the presence or absence of peripheral vitreous compression treatment and the degree of ZW is not uniform even in PE. Ideally, intraoperative findings should be evaluated under a unified view using the ZW classification and the aforementioned disease classification should be clarified and then re-evaluated again. However, data accumulation was impossible in this study.
In conclusion, as mentioned previously, the time to IOL dislocation after cataract surgery was examined according to different risk factors. Based on the average time to dislocation for each risk factor, consider the patient background and risk factors, such as whether to insert the IOL into the bag as usual to complete the surgery or to convert to scleral-sutured ciliary sulcus fixation or intrascleral fixation. After that, it appears necessary to consider the IOL fixation method. Particular attention should be paid to cases involving both PE and ZW.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Tokunaga Y, Nishimura E, Soda M (2023) Examination of Risk Factors Influencing the Time to in-the-bag-Intraocular Lens Dislocation. J Clin Exp Ophthalmol. 14:961
Received: 27-Oct-2023, Manuscript No. JCEO-23-27051; Editor assigned: 30-Oct-2023, Pre QC No. JCEO-23-27051 (PQ); Reviewed: 13-Nov-2023, QC No. JCEO-23-27051; Revised: 20-Nov-2023, Manuscript No. JCEO-23-27051 (R); Published: 28-Nov-2023 , DOI: 10.35248/2155-9570.23.14.961
Copyright: © 2023 Tokunaga Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.