Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Case Report - (2019)Volume 7, Issue 4
Takotsubo syndrome (TS) is a recognized acute cardiac disease entity. The defining feature of TS is the regional circumferential pattern of left ventricular wall motion abnormality (LVWMA) with good contractions in the remainder of the left ventricle resulting in a conspicuous ballooning of the left ventricle during systole. In about 70 of cases, TS is preceded by an emotional or a physical stress factor. Externally administered epinephrine or innate elevation of epinephrine in diseased condition as pheochromocytoma has been reported to trigger TS. Herein, we report the case of a 42-year-old man with epinephrine-induced TS with 3 important features: immediate induction of the disease after epinephrine administration and rapid recovery; the mid-basal pattern (inverted) TS pattern, which may be seen in one thirds of patients with epinephrine-induced TS; and the post-extrasystolic augmentation of the stunned myocardial contractility.
Takotsubo; Epinephrine; Pheochromocytoma; Myocardial stunning; Broken heart syndrome
LVWMA: Left Ventricular Wall Motion Abnormality
Takotsubo syndrome is currently a recognized acute cardiac disease entity, characterized by reversible regional left ventricular wall motion abnormality (LVWMA) extending beyond the coronary artery supply territory [1]. The term takotsubo was introduced in 1990 and 1991 to describe the silhouette of the left ventricle during systole in patients with clinical features of myocardial infarction without obstructive coronary artery disease [2,3]. The defining feature of TS is the circumferential pattern of LVWMA with good contraction in the remainder of left ventricular wall resulting in a conspicuous ballooning of the left ventricle during systole. The ballooning may be localized to the apical, mid-apical, midventricular, mid-basal and basal segments [4]. Focal and global TS have also been reported [1]. One third of patients may have right ventricular involvement. In about 70% of patients with TS, the disease is preceded by either an emotional or a physical stress factor [5]. External catecholamine administration including epinephrine [6,7] and in diseases characterized by hypercatecholaminemia such as pheochromocytoma [8,9] have been reported to induce TS. Herein, we report on a case of epinephrine-triggered inverted TS with post-extra-systolic augmentation in the contractility of the left ventricle including in the stunned segments of the myocardium.
Takotsubo syndrome is currently a recognized acute cardiac disease entity, characterized by reversible regional left ventricular wall motion abnormality (LVWMA) extending beyond the coronary artery supply territory [1]. The term takotsubo was introduced in 1990 and 1991 to describe the silhouette of the left ventricle during systole in patients with clinical features of myocardial infarction without obstructive coronary artery disease [2,3]. The defining feature of TS is the circumferential pattern of LVWMA with good contraction in the remainder of left ventricular wall resulting in a conspicuous ballooning of the left ventricle during systole. The ballooning may be localized to the apical, mid-apical, midventricular, mid-basal and basal segments [4]. Focal and global TS have also been reported [1]. One third of patients may have right ventricular involvement. In about 70% of patients with TS, the disease is preceded by either an emotional or a physical stress factor [5]. External catecholamine administration including epinephrine [6,7] and in diseases characterized by hypercatecholaminemia such as pheochromocytoma [8,9] have been reported to induce TS. Herein, we report on a case of epinephrine-triggered inverted TS with post-extra-systolic augmentation in the contractility of the left ventricle including in the stunned segments of the myocardium.
A 42-year-old man with a history of Horton´s headache. The patient was referred for bronchoscopy for suspicion of an unidentified 1cm pulmonary change in the left upper lobe. He was pre-medicated with morphine. During introduction of the bronchoscopy tube, he developed vasovagal reaction with severe bradycardia with almost a systole and hypotension. The patient received epinephrine 0.5 mg intravenously and naloxone 0.4 mg. The heart rate increased immediately to 170/min and the blood pressure to 180/135 mmHg. The patient developed headache, and chest pain. The blood pressure and the heart rate stabilized thereafter. The electrocardiogram (ECG) revealed ST-depression in V4-6 and in the inferior leads with T wave inversion in the inferior leads. Some ST-elevation was noted in the leads 1 and aVL (Figure 1A). The patient was referred for emergency invasive coronary angiography, which showed no signs of obstructive coronary artery disease (Figures 1B and C). Contrast left ventriculography showed marked hypokinesia in the middle and basal segments of the left ventricle with normal contractility in the apical segments (Figures 2A and B). There was augmentation of post-extra-systolic left ventricular contractility even in the hypokinetic stunned segments (Figures 2C-E). There was moderate elevation of plasma troponin 742 nanog/L. Echocardiography, one day after admission, showed normalization of the left ventricular function with ejection fraction 55%. Cardiac magnetic resonance imaging 2 days after admission revealed also almost normalization of the left ventricular function and signs of myocardial edema in the mid-basal segments of the left ventricle. Treatment with acetylsalicylic acid and beta blocker were initiated. He was investigated for pheochromocytoma and revealed normal plasma metanephrine (<0.2 nmol/L, normal<0.3 nmol/L) and normetanephrine (0.2 nmol/L, normal <0.6 nmol/L), which were obtained on third day of admission.
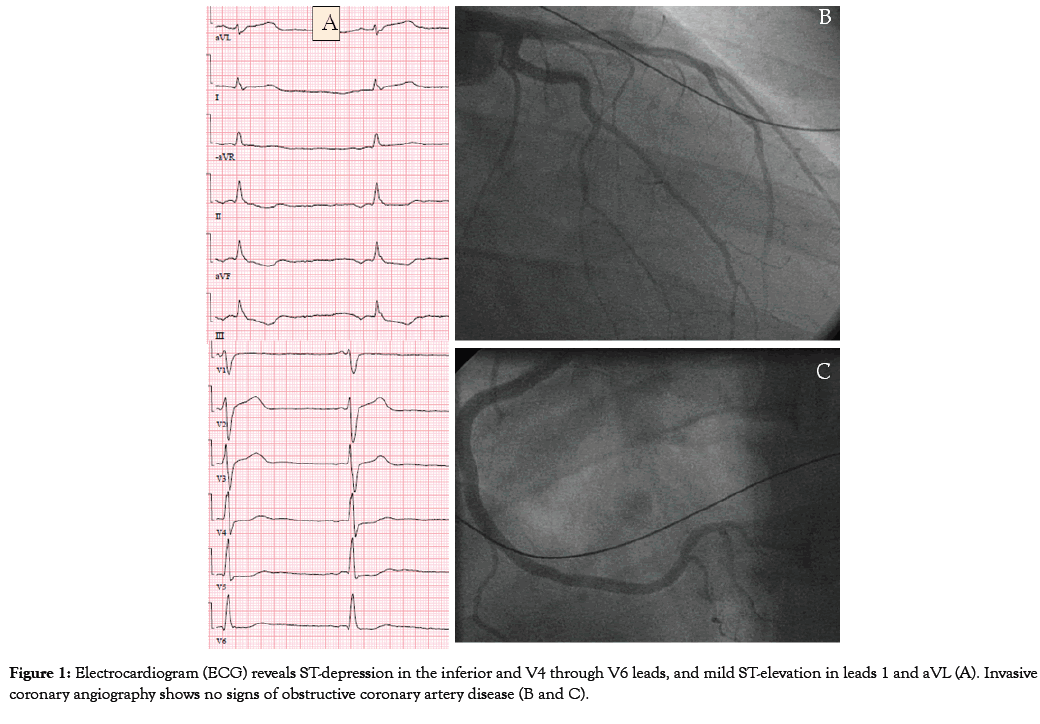
Figure 1: Electrocardiogram (ECG) reveals ST-depression in the inferior and V4 through V6 leads, and mild ST-elevation in leads 1 and aVL (A). Invasive coronary angiography shows no signs of obstructive coronary artery disease (B and C).
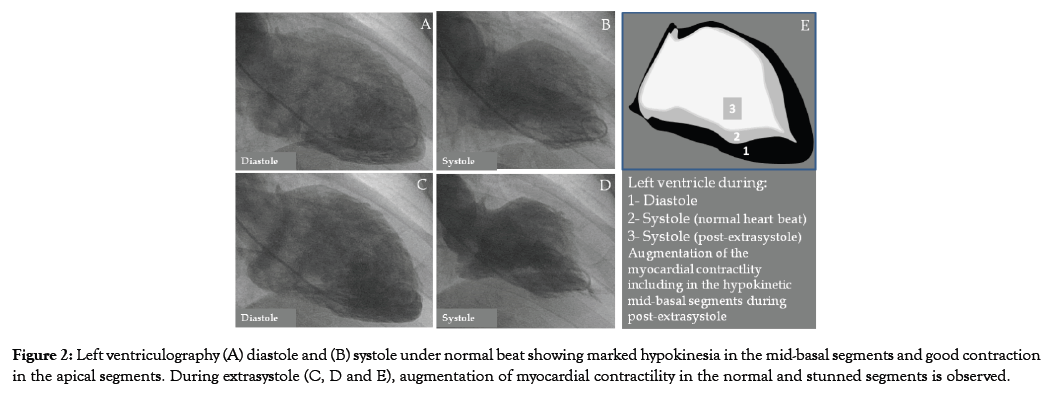
Figure 2: Left ventriculography (A) diastole and (B) systole under normal beat showing marked hypokinesia in the mid-basal segments and good contraction in the apical segments. During extrasystole (C, D and E), augmentation of myocardial contractility in the normal and stunned segments is observed.
Main findings in the present case are:
1) Takotsubo syndrome was triggered most probably by epinephrine injection where the chest pain started immediately after epinephrine injection and there was rapid recovery of the left ventricular wall motion abnormality (LVWMA) where the echocardiography showed normal left ventricular function one day after the disease onset. Epinephrine-induced TS is characterized by a dramatic clinical presentation where the clear majority of patients developed symptoms of hemodynamic disturbances immediately after the injection in a review study [7]. In 17 of 20 cases, the symptoms or the hemodynamic disturbances started immediately, directly or shortly (within minutes) after epinephrine administration [7]. In the same study, 11 of 17 (65%) patients where the recovery time reported, the left ventricular function was normalized within one week; in 3 patients, the normalization period of the left ventricular function was <2 days, where in one of them as short as 30 minutes. In the current case the left ventricular function normalized one day after admission. Moreover, it should be recognized that the stress of bronchoscopy with the associated vasovagal reaction may have contributed to the induction of TS.
2) The pattern of the LVWMA was mid-basal ballooning with normal contractility in the apical segments. The inverted TS pattern (basal or mid-basal) was reported in almost one third of patients with epinephrine- and pheochromocytoma-induced TS [6-9]. The apical sparing pattern (mid-ventricular, mid-basal or basal) is reported in 31.5% to 51.22% of patients with epinephrine- and pheochromocytoma-induced TS [6-9]. This contrasts with other all- TS population, where only 2.2% had basal (inverted) and 16.8% had apical sparing type [5]. The apical sparing pattern in this patient and in almost half of the patients with epinephrine-induced TS challenges strongly the hypothesis of epinephrine induced switch in intracellular signal trafficking from beta 2-adrenoceptor-Gs to beta 2-adrenoceptor-Gi causing apical ballooning in TS [1,10]. 3) Post-extra-systolic potentiation of myocardial contractility even in the hypokinetic segments was noted in the left ventriculography (Figure 2E) in the current patient indicating viable stunned but hypokinetic myocardium. Because of its instantaneous nature, post-extra-systolic potentiation represents a potent inotropic stimulus without risk of provoking ischemia, and may be used for identifying viable myocardium in patient with ischemic heart disease undergoing myocardial revascularization [11].
A case of epinephrine-induced inverted TS, with immediate inception after epinephrine administration and rapid recovery, is presented. Post extra-systolic augmentation of myocardial contractility in the stunned segments was observed indicating viable but stunned myocardium.
Citation: Y-Hassan S, Henareh L (2019) Epinephrine-Induced Inverted Takotsubo Syndrome: Postextrasystolic Potentiation of the Stunned Myocardial Contractility. Angiol Open Access. 7:234. doi: 10.35248/2329-9495.19.7.234
Received: 28-Aug-2019 Accepted: 13-Nov-2019 Published: 20-Nov-2019 , DOI: 10.35248/2329-9495.21.7.234
Copyright: © 2019 Hassan YS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.