Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2020)
Purpose: One of the most feared complications of intraocular tumor biopsy with fine needle aspiration biopsy (FNAB) or vitrectomy-assisted biopsy is seeding of the tumor cells directly into the needle tract. We present a case of epibulbar seeding of uveal MALT lymphoma following vitrectomy.
Observations: A 67-year-old male presented with painless loss of vision of the left eye and creamy yellow infiltrates at the level of the choroid. A diagnostic 25-gauge pars plana vitrectomy was performed using a standard 3-port approach. Choroidal biopsy of the lesion demonstrated the presence of Mucosa-Associated Lymphoid Tissue (MALT) lymphoma. Three weeks following vitrectomy, the patient developed a large fleshy subconjunctival mass centered over the prior superonasal sclerotomy site. The lesion was completely excised and histopathology of the lesion demonstrated MALT lymphoma with an identical immunohistochemical staining pattern to that of the choroidal lesion.
Conclusions and Importance: Transvitreal biopsy with fine needle aspiration or vitrectomy is an increasingly common and safe procedure for clinical diagnosis of intraocular tumors. However, there is a risk of tumor seeding of the needle tract and precautions to reduce this risk are warranted.
MALT lymphoma; Uveal lymphoma; Choroidal lymphoma; Vitrectomy-assisted biopsy; Tumor seeding; Epibulbar extension
Uveal lymphoma is a rare intraocular malignancy with approximately 70-80 cases previously reported in the literature. It is important to distinguish uveal lymphoma from primary vitreoretinal lymphoma (PVRL), which represents a distinct disease entity despite sharing a similar clinical appearance. While uveal lymphoma often runs a benign course with excellent prognosis, vitreoretinal lymphoma is characteristically a high-grade large B-cell lymphoma with an aggressive course, high association with CNS involvement in approximately 80% of cases [1], and a uniformly poor prognosis [2]. In contrast, primary uveal lymphoma is predominantly extranodal marginal zone B-cell type (EMZL), between 60-80% of cases [3], otherwise known as mucosa-associated lymphoid tissue (MALT) lymphoma. Clinical presentation of primary uveal lymphoma is characterized by its prolonged and indolent course, diffusely thickened choroid on ultrasound, creamy yellow-white infiltrates at the level of the choroid, and patchy depigmentation of the RPE. Definitive diagnosis requires histopathologic confirmation. The variability of presentation in addition to the scarcity of this disease often leads to misdiagnosis. Common misdiagnoses include amelanotic melanoma, metastatic carcinoma and carcinoid tumors, choroidal hemangioma, inflammatory diseases such as VKH, birdshot choroidopathy, posterior scleritis, uveal effusion syndrome, various uveitic entities including sarcoid and infectious causes such as tuberculous granuloma.
We present a case of choroidal MALT lymphoma confirmed with choroidal biopsy and subsequent development of epibulbar MALT lymphoma after diagnostic vitrectomy.
A 67-year-old Hispanic male presented to our clinic complaining of painless decrease of vision in his left eye. He had a complicated past ophthalmic history including bilateral branch retinal vein occlusions (BRVO) complicated by a tractional retinal detachment in his left eye repaired with a 20-gauge vitrectomy, scleral buckle, silicone oil and peripheral endolaser. The left eye subsequently underwent cataract surgery, YAG capsulotomy and silicone oil removal, leaving him with a visual acuity of 20/100. The patient was lost to follow-up for 8 years before returning to our clinic. His past medical history was significant only for hypertension uncontrolled on two medications and a prior history of H. Pylori.
On presentation the visual acuity in his left eye had decreased from 20/100 to 1’/200 and remained stable at 20/40 in his right eye. Intraocular pressure was 14 mmHg in the right eye and 13 mmHg in the left eye. Examination of the pupils demonstrated a 3+ relative afferent pupillary defect of the left eye. Slit lamp examination (SLE) showed a white and quiet conjunctiva without visible lesions. The anterior chamber of the left eye showed 2+ cell and flare, a well-positioned posterior chamber intraocular lens (PCIOL), and 2+ cell in the post-vitrectomy posterior chamber. Dilated fundus examination (DFE) of the left eye revealed an elevated creamy yellow lesion of the temporal macula (greater than 4 disc diameter) and two smaller lesions of about 1 disc diameter adjacent to the superior arcade. There was also an extensive leopard skin pattern of pigmentation extending inferior from the disc from 5 to 7 o’clock (Figure 1a). Diffuse choroidal folds, sclerotic vasculature and optic nerve pallor with a 0.3 cup-to- disc ratio were also noted. Circumferential endolaser and previously lasered atrophic holes in the superotemporal quadrant were stable. SLE and DFE of the right eye were unremarkable except for mild ERM, ghost vessels with dense prior laser burns in the superotemporal quadrant as evidence of prior BRVO.
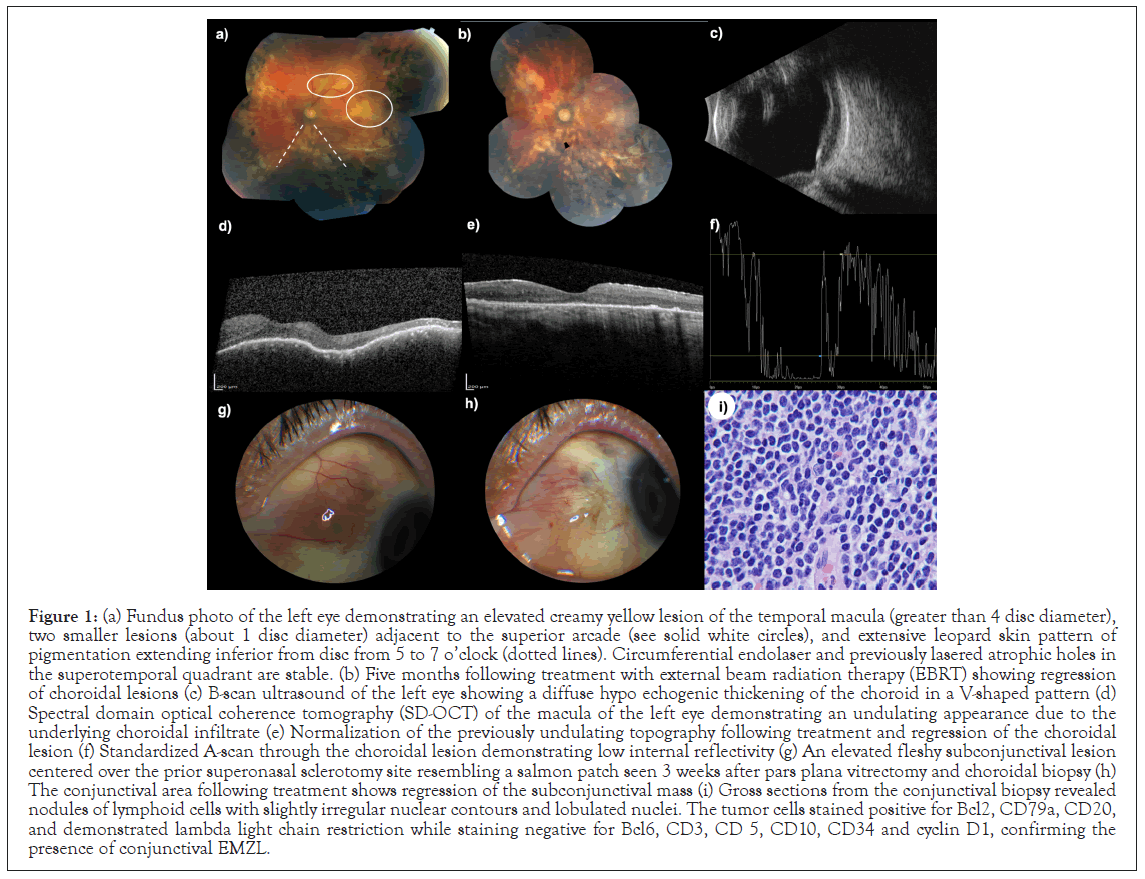
Figure 1: (a) Fundus photo of the left eye demonstrating an elevated creamy yellow lesion of the temporal macula (greater than 4 disc diameter), two smaller lesions (about 1 disc diameter) adjacent to the superior arcade (see solid white circles), and extensive leopard skin pattern of pigmentation extending inferior from disc from 5 to 7 o’clock (dotted lines). Circumferential endolaser and previously lasered atrophic holes in the superotemporal quadrant are stable. (b) Five months following treatment with external beam radiation therapy (EBRT) showing regression of choroidal lesions (c) B-scan ultrasound of the left eye showing a diffuse hypo echogenic thickening of the choroid in a V-shaped pattern (d) Spectral domain optical coherence tomography (SD-OCT) of the macula of the left eye demonstrating an undulating appearance due to the underlying choroidal infiltrate (e) Normalization of the previously undulating topography following treatment and regression of the choroidal lesion (f) Standardized A-scan through the choroidal lesion demonstrating low internal reflectivity (g) An elevated fleshy subconjunctival lesion centered over the prior superonasal sclerotomy site resembling a salmon patch seen 3 weeks after pars plana vitrectomy and choroidal biopsy (h) The conjunctival area following treatment shows regression of the subconjunctival mass (i) Gross sections from the conjunctival biopsy revealed nodules of lymphoid cells with slightly irregular nuclear contours and lobulated nuclei. The tumor cells stained positive for Bcl2, CD79a, CD20, and demonstrated lambda light chain restriction while staining negative for Bcl6, CD3, CD 5, CD10, CD34 and cyclin D1, confirming the presence of conjunctival EMZL.
Optical coherence tomography (OCT) of the macula of the left eye demonstrated a choroidal mass of mild hyper reflectivity with an undulating appearance (Figure 1d). These findings were new compared with the previous OCT study 8 years prior. B-scan ultrasound of the left eye revealed a diffuse hypo echoic thickening of the choroid in a V-shaped pattern with standardized A-scan demonstrating low internal reflectivity (Figure 1c,f). Fluorescein angiography (FA) demonstrated delayed filling with a granular pattern of hyper fluorescence and linear hypo fluorescent folds centrally with development of intense subretinal leakage in the area of the temporal macula. Given the presence of vitritis in conjunction with creamy white chorioretinal infiltrates, the concern for intraocular malignancy, including PVRL, was high and the patient was referred to hematology/oncology for systemic work-up. CBC, CMP, and LDH were unremarkable and whole body PET/CT showed no evidence of orbital or systemic disease. The decision was made to take the patient to the operating room for vitrectomy with biopsy of both the vitreous and choroidal lesions. A 25-gauge pars plana vitrectomy with a standard 3-port approach was performed using valved trocar cannulas. Vitreous aspiration was performed and a sample of undiluted vitreous was obtained. The vitrector was then gently passed into the choroidal lesion and activated, obtaining a sample of choroidal tissue. During this maneuver the infusion pressure was briefly elevated to 80 mmHg to obtain hemostasis. All biopsy maneuvers were performed through the superonasal cannula which required multiple entries to obtain the vitreous and choroidal samples. Endolaser was placed around the retinotomy and endodiathermy was performed. Once hemostasis was obtained, the cannulas were removed and the temporal sclerotomies were sutured. The superonasal sclerotomy was free of leaks and was left sutureless. Cryotherapy was not applied. While awaiting definitive tissue diagnosis, the decision was made to start the patient on a course of intravitreal methotrexate starting with a loading dose of 400 mcg weekly for 4 weeks followed by monthly injections.
Immunohistochemistry of the choroidal lesion demonstrated a monoclonal population of large cells with positive staining of CD19, CD20, CD43 and Bcl2 with restriction of lambda light chain (4% of total cellularity) and negative staining for CD5, CD10, CD38 which was consistent with a diagnosis of extra nodal marginal zone B-cell lymphoma (EMZL). Molecular testing (FISH) of the choroidal sample was negative for t (11;14)(q13:q32) (CCND1/IGH) gene fusion. Vitreous sampling was mostly a -cellular but demonstrated a few CD68-positive cells consistent with macrophages. PCR evaluation of the vitreous sample was negative for CMV, EBV, HSV, VZV, and toxoplasma. The patient underwent extensive staging with MRI of brain, orbits and spine which demonstrated choroidal thickening with subtle enhancement in the left eye but was otherwise normal without orbital or retrobulbar masses. Lumbar puncture, bone marrow biopsy, HIV and hepatitis panel were likewise unremarkable.
On 3-week follow-up after choroidal biopsy the patient was noted to have developed a large elevated fleshy subconjunctival lesion centered over the prior superonasal sclerotomy site resembling a salmon patch (Figure 1g). The conjunctival lesion was fully excised with clear margins and sent to pathology. While awaiting definitive diagnosis the patient was continued on intraocular methotrexate for a total of seven doses. Sections from the conjunctival biopsy subsequently revealed benign squamous epithelium with underlying connective tissue showing a nodule of lymphoid cells with slightly irregular nuclear contours and lobulated nuclei (Figure 1i). The tumor cells stained positive for Bcl2, CD79a, CD20, and demonstrated lambda light chain restriction while staining negative for Bcl6, CD3, CD 5, CD10, CD34 and cyclin D1. The proliferation index was low (Ki67 <10%). This pattern confirmed the presence of conjunctival EMZL. The immunohistochemical staining pattern was identical to that of the choroidal tumor.
The patient was referred to radiation-oncology and based on their recommendation; the patient was treated with external beam radiation therapy (EBRT) to bilateral orbits for a total dose of 30 Gy in 15 divided doses. Five months following EBRT treatment, regression of choroidal lesions with normalization of the choroidal corrugations was noted, though the leopard skin appearance remained as diffuse areas of RPE atrophy (Figure 1b). The conjunctival area remained white without recurrent infiltrates (Figure 1h) and the final visual acuity was 20/400.
We present a patient with primary MALT lymphoma of the choroid with delayed epibulbar involvement following vitrectomy. The patient demonstrated the classic findings of diffusely thickened choroid on ultrasound and multiple creamy yellow-white infiltrates at the level of the choroid, but the development of an accompanying subconjunctival/epibulbar mass was unusual. The location of the lesion directly over the prior superonasal sclerotomy site and its speed of proliferation was concerning for epibulbar seeding of the choroidal tumor during vitrectomy-assisted biopsy. Multiple studies have demonstrated experimentally the potential seeding of tumor cells into the needle tract following Fine Needle Aspiration Biopsy (FNAB) in enucleated eyes [4,5]. However, the prevalence of clinical cases with documented extra-ocular seeding of tumors in the ophthalmic literature is exceedingly rare. There are only seven case reports in the literature documenting extra-ocular extension of uveal melanoma following FNAB, vitrectomy, or open biopsy [6-11]. There is only a single reported case of extra-ocular extension of intraocular lymphoma after vitrectomy [12]. We report a case of primary uveal MALT lymphoma with presumed extra ocular extension through seeding of the vitrectomy tract during transvitreal biopsy. Factors theorized to reduce the risk of tumor seeding during tumor biopsy include the use of small-gauge needles, limiting use of an infusion line, cryotherapy applied at the scleral entry site, suturing of sclerotomy wounds, and immediate treatment of the tumor after biopsy, typically with a radioactive plaque [9,13]. It is generally accepted that transvitreal biopsy is safe if these precautions are followed. It is likely that our patient was at higher risk of tumor seeding due to several factors. Multiple passes were made through the superonasal cannula with use of an infusion line, and the intraocular pressure was elevated briefly during the choroidal biopsy to achieve hemostasis. Critically, the decision was made to leave the superonasal sclerotomy unsutured and without cryotherapy. Additional evidence that the epibulbar mass was the result of tumor seeding is that the immunohistochemical staining patterns of both choroidal and epibulbar masses were identical.
We present a case of presumed epibulbar seeding of intraocular uveal MALT lymphoma following vitrectomy. Transvitreal biopsy with fine needle or vitrectomy is an increasingly common and safe procedure for clinical diagnosis of intraocular tumors. However, there is a risk of seeding of the surgical wound and several considerations aimed at reducing this risk are warranted. These include use of the smallest possible gauge of needle or vitrectomy system, limiting use of an infusion line when possible, cryotherapy applied at the scleral entry site, and suturing of all sclerotomy wounds. Though rare, it is important to recognize the distinct clinical features of MALT lymphoma of the uvea for safe and timely diagnosis of this disease.
Written consent was obtained from the patient to publish the case report. This report does not contain any personal information that could lead to identification of the patient.
We thank Dr. Ruc Tran for providing excellent pathology photos and Dr. Ellen McPhail for providing cytogenetic and immunohistochemical analysis.
Citation: Clark P, McCartney D, Mitchell K, Shami M (2020) Epibulbar Seeding of Uveal MALT Lymphoma Following Vitrectomy. J Clin Exp Ophthalmol. 11:865.
Received: 06-Nov-2020 Accepted: 20-Nov-2020 Published: 27-Nov-2020
Copyright: © 2020 Clark P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.