Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2024)Volume 15, Issue 1
The case study is regarding a 50-year-old patient who had been undergoing corticosteroid therapy for renal disease. The patient was referred to Erasme Hospital due to a significant and a progressive decline in visual acuity in his left eye and was hospitalized for the management of uveitis, a condition characterized by inflammation of the uvea, which is the middle layer of the eye. Further investigations revealed a rare etiology i.e., Aspergillosis endophthalmitis. Endophthalmitis refers to inflammation within the eyeball, and in this case, it was associated with an infection caused by the fungus Aspergillus. Aspergillosis endophthalmitis is an infrequently reported clinical presentation in patients considered to be at risk of invasive aspergillosis. The association between corticosteroid use and the occurrence of aspergillosis endophthalmitis underscores the importance of considering the potential side effects and complications associated with immunosuppressive treatments. It also highlights the need for vigilance in monitoring patients who are at an increased risk of fungal infections, especially with unusual symptoms such as a drastic decrease in visual acuity.
Uveitis; Endophthalmitis; Invasive aspergillosis; Corticosteroid therapy
Aspergillus fumigatus is a fungus commonly considered a harmless saprophyte and is ubiquitous in the environment. It typically causes self-limiting infections [1]. However, in some cases, the infection can be severe and disseminate hematogenously, leading to invasive aspergillosis [2]. Invasive aspergillosis is usually observed in immunocompromised patients, such as those with hematologic malignancies, Human Immunodeficiency Virus (HIV) infection, solid tumors or those receiving immunosuppressive agents, including corticosteroids [3]. While the infection primarily affects the lungs, it can also manifest in extra pulmonary sites, including the central nervous system, heart, kidneys, skin and eyes. The symptoms of invasive aspergillosis are often non- specific and clinical signs can vary due to the involvement of multiple organs. Ocular pain and/or decreased visual acuity can indicate the presence of endogenous endophthalmitis [4]. Through this clinical case, we aim to emphasize the importance of a multidisciplinary approach and early diagnosis of invasive aspergillosis.
Patient history
Our patient was a 50-year-old man who had been under medical care since January 2021 for stage IIIa-IIIb chronic kidney disease. In May 2021, a renal biopsy revealed focal segmental glomerulonephritis (Immunoglobulin A (IgA) nephropathy), for which oral corticotherapy with methylprednisolone 64 mg per day was initiated for 2 months and gradually reduced to 32 mg approximately 1 month before his admission to our department.
In July 2021, he consulted his primary care physician due to fever, pharyngeal pain and left otalgia. As he had a sub- febrile temperature, the primary care physician recommended symptomatic treatment. However, as the symptoms worsened and the patient experienced a sudden decrease in vision in his left eye accompanied by scintillating scotomas and holocranial headaches, he was hospitalized.
Blood tests showed a moderate inflammatory response (C-Reactive Protein (CRP) at 61.1 mg/L). Thoracic Computed Tomography (CT) scans revealed multiple pulmonary nodules. Ophthalmological examination revealed white retinal lesions and a fibrillar appearance in the vitreous. The patient was transferred to us at this stage for the management of a presumed infectious uveitis.
Upon arrival, the patient reports a significant and progressive decrease in visual acuity, along with an intermittent sensation of tension in the left eye. The best-corrected visual acuity, according to the Monoyer chart, was 10/10 in the right eye and 1.6/10 in the left eye. Slit lamp examination showed an anterior chamber inflammatory reaction with 4+ cellular Tyndall in the left eye. Fundus examination revealed numerous hemorrhages and white retinal lesions accompanied by significant vitritis as shown in Figure 1. The clinical examination of the right eye was unremarkable.
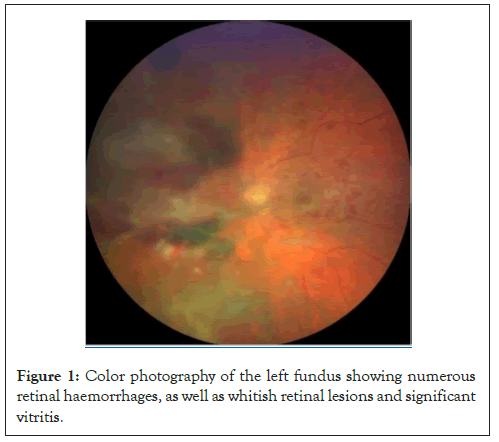
Figure 1: Color photography of the left fundus showing numerous retinal haemorrhages, as well as whitish retinal lesions and significant vitritis.
Fluorescein angiography of the left eye revealed hypofluorescence in the nasal retina corresponding to hemorrhagic areas and macular leakage. Figure 2 shows that the Optical Coherence Tomography (OCT) confirmed macular edema and showed focal hyper reflectivity under the fovea (Figures 1 and 2).
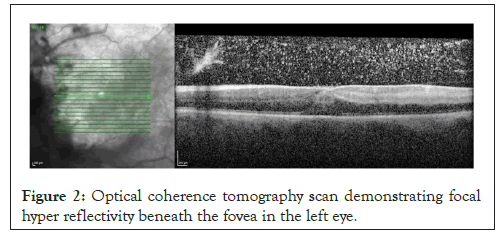
Figure 2: Optical coherence tomography scan demonstrating focal hyper reflectivity beneath the fovea in the left eye.
The patient was hospitalized with a presumptive diagnosis of Cytomegalovirus (CMV) retinitis and intravenous ganciclovir therapy was initiated. An anterior chamber paracentesis is performed and the patient is hospitalized with a presumptive diagnosis of CMV retinitis with the aim of initiating intravenous ganciclovir treatment. Laboratory tests revealed a CRP of 110 mg/L (normal range <5), mild leukocytosis (12,550/mm³, normal range is 3-11,000) and anemia (hemoglobin at 8 g/dL, normal range is 13-18). FAN and Anti-Neutrophil Cytoplasmic Antibodies (ANCA) tests were negative. Viral Polymerase Chain Reaction (PCR) tests on aqueous humor were also negative. Immunoglobulin G (IgG) antibodies were found for toxoplasmosis, Epstein-Barr Virus (EBV), Herpes Simplex Virus (HSV) and Varicella Zoster Virus (VZV), but not CMV. Serologies were negative for syphilis, HIV, Rickettsia, Bartonella, Brucella and Aspergillus.
PWithin 72 hours of hospitalization, the patient experienced a rapid deterioration in his general condition, particularly in the neurological and respiratory aspects, leading to admission to the intensive care unit. Unfortunately, the subsequent clinical course was marked by a stroke with multiple ischemic lesions demonstrated by Magnetic Resonance Imaging (MRI), as well as a suspected pyogenic abscess in the left temporal region, as revealed by transesophageal echocardiography, showing a pedunculated intracardiac mass on the left ventricular inferolateral wall, suggestive of thrombosis or endocarditis.
This dramatic clinical progression led the medical team, in agreement with the family, to discontinue invasive treatments and provide palliative care. A post-mortem biopsy of a hardened nodule on the anterior aspect of the right thigh revealed Aspergillus filaments within a necrotic infiltrate. Aspergillus fumigatus filaments were also found in Broncho-alveolar lavage performed three days after the patient's admission.
Aspergillosis, caused by fungi belonging to the Aspergillus family, with Aspergillus fumigatus being the most common, is usually harmless to the general population. Spores are carried by the air and are typically inhaled without consequence. However, in cases like that of our patient, compromised immunity can create conditions for devastating infection. Invasive aspergillosis, characterized by symptoms such as cough, chest pain, hemoptysis and respiratory distress, is often encountered in immunocompromised patients. Immediate consideration is given to bronchial or blood cultures for microbiological analysis and lung lesion evaluation using chest CT scans.
Endophthalmitis due to Aspergillus is a rarely reported clinical presentation in patients considered at risk of invasive aspergillosis, but there is a known association between this condition and the use of corticosteroids. Ocular involvement typically presents as fulminant endophthalmitis, marked by chorioretinal masses, retinal exudative lesions, vitritis and anterior segment inflammation. Orbital involvement or canalicular system compromise may also occur.
The diagnosis of Aspergillus endophthalmitis is challenging because blood cultures and other serological or cutaneous tests are generally uninformative. In most cases, the final diagnosis is made through vitreous biopsy or post-mortem examination, which was the case with our patient. Treatment typically involves the use of intravitreal and/or systemic amphotericin B along with therapeutic vitrectomy, which may be repeated as necessary [5,6].
Our patient, who was otherwise healthy before the nephrological diagnosis, developed rapidly progressive intraocular inflammation, multiple excavated lung nodules and several cerebral ischemic lesions after only three months of systemic corticosteroid therapy. As in most cases, blood cultures were negative and the diagnosis of invasive aspergillosis was unfortunately only confirmed post-mortem. Due to the likely viral etiology, we had initially considered anterior chamber tap for viral PCR. The fact that the patient had been on systemic corticosteroid monotherapy for only three months did not immediately suggest a fungal infection.
The rapidity of his admission to the intensive care unit (60 hours after our initial examination) did not allow us to arrange a diagnostic vitrectomy. The analysis of the vitreous might have potentially allowed us to identify Aspergillus filaments. Given its often unfavorable prognosis and rapid, potentially fatal progression, a diagnostic vitrectomy should be promptly performed in search of a fungal infection in any patient on immunosuppressive therapy, including corticosteroids, with rapidly progressive retinitis unresponsive to first-line antivirals.
Fungal endogenous endophthalmitis should be considered and ruled out by diagnostic vitrectomy in any patient with a history of corticosteroid use when viral ocular involvement is suspected and the patient does not respond favorably to appropriate antiviral treatment. A vitrectomy is a surgical procedure involving the removal of the vitreous humor, the gel-like substance inside the eye. A diagnostic vitrectomy, also known as retinal biopsy is suggested to obtain a sample of the vitreous humor for laboratory analysis, also to identify conditions such as intraocular lymphoma. This allows for a direct examination of the ocular tissues to identify the presence of fungal pathogens.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Hassani MC, Hakami S, Afsari PE, Roux PL, Lipski D, Motulsky E, et al (2024) Aspergillus Endophthalmitis in a Patient on Corticosteroid Therapy: A Case Report. J Clin Exp Ophthalmol. 15:968.
Received: 29-Dec-2023, Manuscript No. JCEO-23-28419; Editor assigned: 01-Jan-2024, Pre QC No. JCEO-23-28419 (PQ); Reviewed: 15-Jan-2024, QC No. JCEO-23-28419; Revised: 22-Jan-2024, Manuscript No. JCEO-23-28419 (R); Published: 29-Jan-2024 , DOI: 10.35248/2155-9570.24.15.968
Copyright: © 2024 Hassani MC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.