
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2021)Volume 11, Issue 6
Objective: This study aimed to explore the effects of periodic telephone follow-ups by a hospital nurse to care managers on the problems faced by patients after discharge.
Methods: Participants included eligible patients who were older than 65 years, had a charge care manager, and were discharged from a hospital to their homes or residential care facilities. A director of nursing conducted the telephone follow-ups for care managers one week, one month, and two months after discharge. The control group received the usual follow-up. As the main outcome, patients were asked to respond to 17 items about the problems faced one week and two months after discharge. Care managers completed a self-administered questionnaire survey on nurses’ cooperation telephonically.
Results: The problems faced by patients two months after discharge were not significantly different from those faced after one week. However, comparing the responses from patients one week and two months after discharge, the proportion of patients’ problems in the intervention group decreased for 11 items. The results of the responses from care managers in the survey on cooperation revealed that “psychological support” and “issues related to information sharing before discharge” were common between the intervention and control groups. “Issues related to the method and practice of cooperation” was an original category of the intervention group, and “no memory of the follow-up” was an original category of the control group.
Conclusion: Periodic telephone follow-ups from hospital nurses to care managers did not statistically annoy patients. Furthermore, it was necessary for the patients to have the same nurse continue with regular telephone follow-ups after discharge. Thus, we recommend the reinforcement of information sharing with the patient before discharge, while also highlighting the need for multiple follow-ups after discharge. Additionally, these follow-ups may be effective for providing psychological support to care managers.
Telephone follow-up; Randomized controlled trial; Psychological support
In Japan, home care has been promoted to effectively use health resources, as the demand for medical and non-medical care increases with the increasing aging rate. Therefore, discharge planning related to patients’ admission has attracted considerable attention. Its general process involves screening assessment, planning, enforcement, and follow-up. The introduction of a screening tool and conferences with bedside nurses has resulted in an improvement of screening and assessment abilities related to discharge planning. However, the effects on patients have not been considered because intervention contents previously did not include continuous follow-ups after discharge [1]. Existing studies on the system of cooperation for continuous nursing within and outside the hospital have investigated cooperation methods through an exchange of documents or conferences held before or at the time of the discharge, mainly in Japan. However, few studies have investigated the effects of the cooperation method for the purpose of follow-ups after discharge, with most studies reporting the effects on patients and their families, based on case studies [2].
However, several studies outside of Japan have conducted telephone follow-ups with patients directly [3,4]. Telephonic counseling on medication, treatment, and the lifestyles of stroke patients showed a positive effect on their blood data and blood pressure in Sweden [5]. Telephone follow-ups for patients with a high risk of rehospitalization were effective in improving their physical function and movement in Australia [6]. Additionally,educational instruction imparted via telephone to patients who needed medical treatment resulted in an increase in their knowledge and understanding in the United States [7]. Another United States study evaluated telephone follow-ups within 72 hours after discharge among patients who had undergone head and neck surgery, showing a statistical decrease of emergency room visits [8].
Care managers form the central part of the interprofessional system of cooperation that offers support to patients; their role involves care management and planning. Problems faced by care managers include insufficient experience and knowledge of techniques. Additionally, restrictions placed by public long-term care insurance and the obstacles caused by socioeconomic circumstances can be challenging for care managers [9].
Against such a background, the role of hospital staff includes follow-ups with community staff to not only ensure a seamless shift to home care, but to also provide the continuous care necessary to patients. Cooperation with care managers is therefore essential.
Purpose
The purpose of this study was to explore the effects of periodic telephone follow-ups by hospital nurses to care managers on the problems faced by patients after their discharge.
We hypothesize that patients whose care managers receive three telephone follow-ups from hospital nurses face fewer problems after discharge than patients whose care managers receive one telephone follow-up.
Study design
This study employed a randomized controlled trial. It was approved by the Ethics Review Board of Sonoda Women’s University (No. 17-04-005) and was registered with the UMIN Clinical Trials Registry (ID: UMIN000032251).
Participants’ eligibility criteria
This study used data from a hospital located in a central city of Japan, which had 150 beds (52 general beds, 52 integrated community care beds, and 46 long-term care beds). Eligible patients were older than 65 years, had a charge care manager, and were discharged from the hospital to their homes or residential care facilities.
Recruitment
An explanation and request for cooperation were provided both orally and in writing by the chief nurses of each ward to eligible patients as well as their charge care managers. The patients and care managers provided their informed consent to participate in this study. An agreement on study cooperation was established by signed written consent from the participants.
Allocation
A random number list was computer-generated before the start of this study. Identities (IDs) for this study were assigned to each of the patient–care manager pairs, after receiving consent from both the patient and their care manager. ID pairs that corresponded to a generated number were categorized as the intervention group.
Sample size
A total of 64 pairs (32 pairs in each group) were required for this study to detect a statistically significant difference at a power of 80% and a significance level of 0.05 (two sides), when the probability that problems after the discharge do not occur was a 30% difference between groups (intervention group 10%, control group 40%) was considered.
Theoretical basis of the intervention
Some studies could not reveal statistically significant effects of follow-ups within two weeks after discharge among patients with chronic [10] and vascular brain disease [11]. Many investigations included the first follow-up within one week after discharge, and the interval of time before the next follow-up was gradually increased [12-14]. Furthermore, families of home care patients required approximately three months to become familiar with medical measures [15]. In reference to these previous studies, the follow-ups of this study were set at one week, one month, and two months after discharge.
A director of nursing who was well-versed in discharge planning conducted the follow-ups telephonically and asked the care manager about the problems and the general situation of the patient after discharge. The director of nursing then gave care managers advice, if necessary.
Intervention group
Within the intervention period, the director of nursing conducted the three follow-ups over the telephone for care managers (one week, one month, and two months after discharge).
Control group
The control group received the usual follow-up, which involved the hospital nurse informing the care manager at the time of discharge to contact the hospital if necessary. A telephone follow-up from the director of nursing to the care manager was conducted once-two months after discharge or when the intervention was completed.
Outcome and data collection
The responses regarding problems faced by patients after discharge were rated on a four-point Likert scale (“I am not troubled,” “I am not very troubled,” “I am somewhat troubled,” and “I am troubled”) for 17 items (physical condition, treatment policy, emergency correspondence, hospital visit or consultation, content of meals, medicine, medical treatment, arrangement of medical equipment and medicaments, long-term care insurance and welfare system procedure, contents of home services, arrangement of care articles, house and house repair, daily life, household affairs, care burden on family, economy, and future medical treatment location) that were identified by a previous study [16]. These items were investigated using the self-administered questionnaire twice (one week and two months after discharge).
As a process evaluation, the self-administered questionnaire was conducted telephonically with care managers to determine cooperation.
Anonymity of nurses and care managers
As the intervention time periods for care managers differed, it was difficult to guarantee the anonymity of the hospital nurses. Similarly, it was challenging to obscure the identity of the care managers in the control group as they conducted the usual follow-up over the telephone once, after the intervention on patients was completed,and the frequency of receiving the follow-up interventions from hospital nurses was different. Patients’ identities were anonymized.
Baseline analysis
Patients’ demographic characteristics and attributes (age, sex, diagnosis [International Classification of Diseases] and care level of long-time care system, cohabitation characteristics, and length of hospital stay) were gathered from the hospital’s electronic charts. Patients received and filled out the questionnaire regarding the problems they faced within one week after discharge. Similarly, care managers received a questionnaire and provided details regarding their age, sex, qualifications, and years of experience. The data were analyzed using several methods. Mann-Whitney U tests were used to compare patients’ average length of hospital stay and care managers’ average years of experience in the control group and intervention group. Chi-squared tests were used to compare the patients’ diagnosis as well as the care managers’ qualifications in the two groups. Lastly, Fisher’s exact tests were used to compare the other variables in the control group and the intervention group.
Patients’ outcome analysis
Regarding problems faced two months after discharge, answers were analyzed using a Fisher’s exact test for each item after they were classified in two groups; those who faced problems chose “I am somewhat troubled” or “I am troubled,” while those who did not face problems chose “I am not troubled” or “I am not very troubled.”
Process evaluation analysis
The care managers’ responses were analyzed using a Fisher’s exact test for multiple-choice answers and a qualitative analysis for the free descriptive answers; these were compared between the intervention and control groups.
Participation
The target patients of this study were 6,350 people hospitalized from May 2018 to December 2019 who had a charge care manager. There were 142 care managers who agreed to participate in the intervention, while 13 pairs of patients or their family members agreed to participate. Based on random computer-generated numbers, the 13 pairs were assigned to 5 pairs in the intervention group and 8 pairs in the control group (Figure 1).
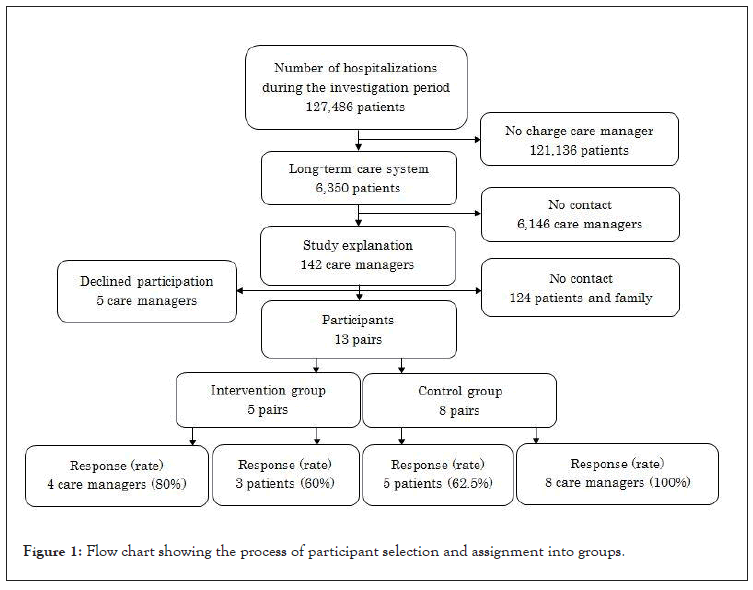
Figure 1: Flow chart showing the process of participant selection and assignment into groups.
Self-administered questionnaire survey for the patients
Three patients from the intervention group (60%) and five from the control group (62.5%) responded to the questionnaire (Figure 1). The demographic characteristics and attributes of the control and intervention groups (Table 1) and the problems faced by patients one week after discharge were not significantly different (Table 2). The problems faced by patients two months after discharge were also not significantly different. However, the result of having compared the responses one week and two months after discharge revealed that the proportion of patients who reported being troubled in the intervention group decreased on 11 items. However, the proportion in the control group reporting the same increased on 13 items. The problem items (emergency correspondence, medicine, content of meals, contents of home services, daily life, house and house repair, future medical treatment location, and hospital visit or consultation) disappeared in the intervention group two months after discharge, while four items (emergency correspondence, medicine, contents of home services, and hospital visit or consultation) still appeared in the control group two months after discharge (Table 3).
| N = 8 | ||||||
|---|---|---|---|---|---|---|
| Intervention (n=3) |
Control (n = 5) |
p-value | ||||
| n | % | n | % | |||
| Age | 60–69 | 0 | 0.0 | 1 | 20.0 | 0.19a) |
| 70–79 | 0 | 0.0 | 1 | 20.0 | ||
| 80–89 | 2 | 66.7 | 0 | 0.0 | ||
| 90–99 | 1 | 33.3 | 3 | 60.0 | ||
| Sex | Male | 2 | 66.7 | 3 | 60.0 | 1a) |
| Female | 1 | 33.3 | 2 | 40.0 | ||
| Diagnosis(International Classification of Diseases) | ||||||
Injury, poisoning, or other consequences of external causes |
0 | 0.0 | 2 | 40.0 | 0.32b) | |
Diseases of the respiratory system |
0 | 0.0 | 1 | 20.0 | ||
Certain infectious or parasitic diseases |
0 | 0.0 | 1 | 20.0 | ||
Diseases of the circulatory system |
1 | 33.3 | 1 | 20.0 | ||
Diseases of the musculoskeletal system or connective tissue |
1 | 33.3 | 0 | 0.0 | ||
Diseases of the digestive system |
1 | 33.3 | 0 | 0.0 | ||
| Care level of long-time care system Needed Support 2 | 1 | 33.3 | 2 | 40.0 | 0.83a) | |
| Needed Long-Term Care 1 | 0 | 0.0 | 1 | 20.0 | ||
| Needed Long-Term Care 4 | 1 | 33.3 | 1 | 20.0 | ||
| Needed Long-Term Care 5 | 1 | 33.3 | 1 | 20.0 | ||
| Cohabitation characteristics Together | 2 | 66.7 | 3 | 60.0 | 1a) | |
Alone |
1 | 33.3 | 2 | 40.0 | ||
| Average length of hospital stay (standard deviation) | 49 (24.2) | 64(55.2) | 0.15c) | |||
The results of a) Fisher’s exact test, b)Chi-squared test, and c) Mann-Whitney U test revealed no significant difference.
Table 1: Patients’ demographic characteristics and attributes.
| N = 8 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 3) | Control (n = 5) | p-value | |||||||||
| Yes | No | Yes | No | ||||||||
| n | % | n | % | n | % | n | % | ||||
| Physical condition | 2 | 66.7 | 1 | 33.3 | 2 | 40.0 | 3 | 60.0 | 1.0 | ||
| Treatment policy | 1 | 33.3 | 2 | 66.7 | 0 | 0.0 | 5 | 100.0 | 0.38 | ||
| Emergency correspondence | 1 | 33.3 | 2 | 66.7 | 0 | 0.0 | 5 | 100.0 | 0.38 | ||
| Hospital visit or consultation | 1 | 33.3 | 2 | 66.7 | 0 | 0.0 | 5 | 100.0 | 0.38 | ||
| Content of meals | 1 | 33.3 | 2 | 66.7 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Medicine | 1 | 33.3 | 2 | 66.7 | 0 | 0.0 | 5 | 100.0 | 0.38 | ||
| Medical treatment | 0 | 0.0 | 3 | 100.0 | 0 | 0.0 | 5 | 100.0 | 1.0 | ||
| Arrangement of medical equipment and medicaments | 0 | 0.0 | 3 | 100.0 | 0 | 0.0 | 5 | 100.0 | 1.0 | ||
| Long-term care insurance and welfare system procedure | 1 | 33.3 | 2 | 66.7 | 0 | 0.0 | 5 | 100.0 | 0.38 | ||
| Contents of home services | 1 | 33.3 | 2 | 66.7 | 0 | 0.0 | 5 | 100.0 | 0.38 | ||
| Arrangement of care articles | 0 | 0.0 | 3 | 100.0 | 0 | 0.0 | 5 | 100.0 | 1.0 | ||
| House and house repair | 1 | 33.3 | 2 | 66.7 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Daily life | 2 | 66.7 | 1 | 33.3 | 3 | 60.0 | 2 | 40.0 | 1.0 | ||
| Household affairs | 2 | 66.7 | 1 | 33.3 | 0 | 0.0 | 5 | 100.0 | 0.11 | ||
| Care burden on family | 2 | 66.7 | 1 | 33.3 | 2 | 40.0 | 3 | 60.0 | 1.0 | ||
| Economy | 0 | 0.0 | 3 | 100.0 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Future medical treatment location | 1 | 33.3 | 2 | 66.7 | 2 | 40.0 | 3 | 60.0 | 1.0 | ||
The results of Fisher’s exact test revealed no significant difference.
Table 2: Troubles faced one week after discharge.
| N = 8 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 3) | Control (n = 5) | p-value | |||||||||
| Yes | No | Yes | No | ||||||||
| n | % | n | % | n | % | n | % | ||||
| Physical condition | 1 | 33.3 | 2 | 66.7 | 2 | 40.0 | 3 | 60.0 | 1.0 | ||
| Treatment policy | 1 | 33.3 | 2 | 66.7 | 2 | 40.0 | 3 | 60.0 | 1.0 | ||
| Emergency correspondence | 0 | 0.0 | 3 | 100.0 | 2 | 40.0 | 3 | 60.0 | 0.46 | ||
| Hospital visit or consultation | 0 | 0.0 | 3 | 100.0 | 3 | 60.0 | 2 | 40.0 | 0.20 | ||
| Content of meals | 0 | 0.0 | 3 | 100.0 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Medicine | 0 | 0.0 | 3 | 100.0 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Medical treatment | 0 | 0.0 | 3 | 100.0 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Arrangement of medical equipment and medicaments | 0 | 0.0 | 3 | 100.0 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Long-term care insurance and welfare system procedure | 1 | 33.3 | 2 | 66.7 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Contents of home services | 0 | 0.0 | 3 | 100.0 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Arrangement of care articles | 0 | 0.0 | 3 | 100.0 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| House and house repair | 0 | 0.0 | 3 | 100.0 | 3 | 60.0 | 2 | 40.0 | 0.20 | ||
| Daily life | 0 | 0.0 | 3 | 100.0 | 3 | 60.0 | 2 | 40.0 | 0.20 | ||
| Household affairs | 1 | 33.3 | 2 | 66.7 | 1 | 20.0 | 4 | 80.0 | 1.0 | ||
| Care burden on family | 1 | 33.3 | 2 | 66.7 | 2 | 40.0 | 3 | 60.0 | 1.0 | ||
| Economy | 0 | 0.0 | 3 | 100.0 | 3 | 60.0 | 2 | 40.0 | 0.20 | ||
| Future medical treatment location | 0 | 0.0 | 3 | 100.0 | 3 | 60.0 | 2 | 40.0 | 0.20 | ||
The results of Fisher’s exact test revealed no significant difference.
Table 3: Troubles at two months after discharge.
Self-administered questionnaire survey for the care managers
Four care managers of the intervention group (80%) and eight care managers of the control group (100%) returned the questionnaire (Figure 1). The demographic characteristics and attributes between the intervention and control groups were not significantly different (Table 4). There was no significant difference in the two questions about cooperation over the telephone. However, a higher proportion of care managers in the intervention group agreed that the telephone follow-up was useful, in response to the two questions (Table 5).
| N = 8 | ||||||
|---|---|---|---|---|---|---|
| Intervention | Control | p-value | ||||
| (n=4) | (n=8) | |||||
| n | % | n | % | |||
Age |
40–49 |
2 | 50.0 | 4 | 50.0 | 1.0a) |
50–59 |
2 | 50.0 | 4 | 50.0 | ||
Sex |
Male |
0 | 0.0 | 2 | 25.0 | 0.52a) |
Female |
4 | 100.0 | 6 | 75.0 | ||
Qualification Care worker |
4 | 100.0 | 4 | 50.0 | 0.38b) | |
Social worker |
0 | 0.0 | 3 | 37.5 | ||
Home helper level 2 |
0 | 0.0 | 1 | 12.5 | ||
Dental hygienist |
0 | 0.0 | 1 | 12.5 | ||
Nursery teacher |
0 | 0.0 | 1 | 12.5 | ||
| Average years of experience (standard deviation) | 5 (5.62) | 10 (1.12) | 0.15c) | |||
The results of a) Fisher’s exact test, b) Chi-squared test, and c) Mann-Whitney U test revealed no significant difference.
Table 4: Troubles at two months after discharge.
| N = 8 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 4) | Control (n = 8) | p-value | |||||||||
| Yes | No | Yes | No | ||||||||
| n | % | n | % | n | % | n | % | ||||
| Was the advice given by the nurse over the telephone helpful? | 3 | 75.0 | 1 | 25.0 | 5 | 62.5 | 3 | 37.5 | 1 | ||
| Do you think that this type of cooperation over the telephone is useful in general? | 4 | 100.0 | 0 | 0.0 | 5 | 62.5 | 3 | 37.5 | 0.49 | ||
The result of Fisher’s exact test revealed no significant difference.
Table 5: Care managers responses on the usefulness of telephone follow-ups.
As a result of the analysis of free descriptive answers regarding cooperation over the telephone, three categories (psychological support, issues related to information sharing before discharge, and issues related to the method and practice of cooperation) were extracted from the intervention group (Table 6) and three categories (psychological support, issues related to information sharing before discharge, and no memory of the follow-up) were extracted from the control group (Table 7). A comparison of the categories between groups revealed that psychological support and issues related to information sharing before discharge were common. “Issues related to the method and practice of cooperation” and “no memory of the follow-up” were original categories of the intervention and control groups, respectively.
| Category | Subcategory | Data |
|---|---|---|
| Psychological support | Thanks | I am very thankful for being able to cooperate and consult after the discharge. |
| Relief | If there is periodical cooperation, it leads to relief. | |
| Issues related to information sharing before discharge | Information sharing regarding the precaution | I don’t know whether the patient understands the precautions stated by the physician. |
| Information sharing of the patient | There is no information sharing about the current situation of the patient. | |
| Issues related to the method and practice of cooperation | Practice of cooperation | I want you to be careful and cooperate with the outpatient department at the time of the patient’s next consultation. |
| If I describe the state of the patients after their discharge, I doubt they will cooperate. | ||
| Cooperation method | If the nurse in charge contacts me, we can compare the situation of the patient before and after discharge. |
Table 6: Free descriptive answers of the intervention group care managers.
| Category | Subcategory | Data |
|---|---|---|
| Psychological support | Thanks | I am very thankful for the cooperation after the discharge. |
| Relief | It was useful for the relief of the care manager. | |
| Safety | The cooperation after the discharge was reassuring. | |
| Issues related to information sharing before the discharge | Hope for information sharing | I want you to inform me about the retirement or change of the chief physician. |
| No memory of the follow-up | No memory | My memory of contacting you is vague. |
| My memory of follow-up is faint. |
Table 7: Free descriptive answers of the control group care managers.
Patients’ effects
Compared to patients in the control group, a larger proportion of patients in the intervention group reported that they did not have problems (based on their responses on majority of the items). As different proportions of care managers in the intervention group felt that telephone follow-ups were useful, we believe that they effectively used the information received from a nurse, and were therefore able to provide a precise response, so that the patients could carry on with their lives without facing any problems. A good relationship with medical staff is necessary to continue home care after discharge. However, the obstacles to interprofessional cooperation for care managers include relationships with physicians; professional competency; relationships among other professionals; environmental constraints; relationships with nonprofessionals; other professionals’ unfamiliarity with the care manager’s role; and the lack of mutual understanding, boundaries, and information sharing among medical professionals [17]. In other words, telephone follow-ups may be an effective method to ensure information sharing.
Telephone follow-ups make correspondence with the hospital possible, especially for emergency correspondence, hospital visits or consultations, and medicine. Because care managers’ basic qualifications differ, they face difficulty not only in the care management of the patients needing medical care, but also in cooperating with physicians and visiting nurses [18]. If the community staff has difficult cases, knowing that the hospital staff can provide backup may offer relief to both patients and care managers.
Regarding “contents of home services,” advice from the viewpoint of nursing may be useful for examining and introducing service contents that the patients use. When care managers introduce home nursing, they refer to advice from nurses [19].
However, there was no significant statistical difference because the intervention contents of this study had a narrow focus: cooperation between a nurse and the care manager. In addition to care managers, various professionals directly support patients who have been discharged from the hospital.
Therefore, care managers who receive follow-ups from hospital nurses must cooperate with the community staff. Interprofessional cooperation in home care is effective against subjectivity about the health of older adults [20]. However, difficulty in cooperation is caused by the lack of understanding the role of other professionals [21]. Because the intervention contents of this study did not enable cooperation between the community staff, it could not lead to significant effects among the patients. A system for care managers to follow with contents they can share among the community staff members who provide home care, is therefore necessary.
Care managers’ effects
Psychological support was improved in both the intervention and control groups. The telephone follow-ups and supplemental specialized knowledge provided by hospital nurses served as emotional support to care managers. Care managers of both the intervention and control groups expressed feelings of gratitude, relief, and safety related to the follow-ups from nurses in their free descriptive answers to the questionnaire.
The association between exercise function level at discharge and the impairment of activities of daily living six months after discharge among older adults needing care is apparent [22]. Therefore, older adults may develop new problems due to the impairment of physical functions after discharge.
Care managers often have regular contact with patients and help to coordinate care between patients and other members of the care team [23]. Therefore, frequent communication can provide timely advice to care managers, leading to relief and better care quality.
Issues of cooperation
The questionnaire responses of the care managers revealed that the precautions to be followed and the situation of the patients before discharge were not shared in a timely manner. Continuous communication between the staff after hospitalization leads to information sharing about the patients and helps build relationships between the staff. Consequently, communication between the staff after discharge becomes a smooth process.
Discharge planning involving interprofessional cooperation influences the satisfaction of health care professionals [24].
Nurses who were not concerned with the patients during hospitalization may have supported care managers in this study; however, continuous communication with the same nurse may provide more concrete advice to the care manager, before and after discharge. Additionally, if the information obtained from the care managers at the time of follow-up is utilized as feedback for discharge planning and for the next outpatient, improvements to discharge planning competency and interprofessional cooperation awareness of bedside nurses can be expected. An existing study of group interviews by integrated community care ward nurses describes the need to strengthen information sharing between the staff to improve the individual ability of discharge planning and the connection between the communities, outpatient department, and ward [25].
Limitations
A limitation of this study is that the findings cannot be generalized because the number of the participants was not as high as planned. The reason the number of participants was not high was because the time available to explain the study contents and obtain consent was limited, as agreements of care managers, patients, and patients’ families were necessary, particularly in the case of the patients with dementia. Unfortunately, constraints concerning entering the hospital due to the COVID-19 pandemic made it hard to achieve study cooperation. However, interprofessional cooperation is required in such situations. The latest case study reports that effective cooperation and communication contribute to the management of patients during the COVID-19 pandemic [26].
In the future, we will have to continue investigating this topic because interprofessional cooperation using information and communication technology, such as telephones, is needed. Moreover, future research needs to focus on introducing patients to a daily routine via a cooperation system after examining the study design and recruitment method to highlight these effects.
This study aimed to explore the effects of periodic follow-ups by telephone between a hospital nurse and care managers on the problems faced by patients after being discharged from the hospital. The results revealed that the patients’ problems two months after the discharge were not significantly different. However, the proportion of patients’ problems in the intervention group decreased on 11 items. Care managers’ responses regarding cooperation over the telephone revealed that “psychological support” and “issues related to information sharing before discharge” were common categories in both the intervention and control groups. “Issues related to the method and practice of cooperation” was an original category of the intervention group, while “no memory of the follow-up” was an original category of the control group. Therefore, periodic follow-ups may be effective for care managers to address some patients’ problems and offer psychological support. In the future, cooperation with the same nurse must continue regularly via telephone follow-ups after patients’ discharge from the hospital.
This study is funded by the Ministry of Health, Labour and Welfare of Japan through the Health and Labour Sciences Research Grant (No. 15K20690), 2014.
The authors declare that they have no competing interests.
Citation: Domoto T, Matsumura Y, Fukada M (2021) Effects of Telephone Follow-Ups After Hospital Discharge on Patients’ Home Care: A Randomized Controlled Trial. J Clin Trials. 11:482.
Received: 09-Sep-2021 Accepted: 23-Sep-2021 Published: 30-Sep-2021 , DOI: 10.35248/2167-0870.21.11.482
Copyright: © 2021 Domoto T, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.