Family Medicine & Medical Science Research
Open Access
ISSN: 2327-4972
ISSN: 2327-4972
Research Article - (2017) Volume 6, Issue 2
Objectives: A study done in Omdurman Maternity Hospital (OMH) during 2013, to study the effect of corticosteroid administration two days before an elective caesarean section to reduce the respiratory morbidity in infants born.
Methodology: It is a randomized control trial study comparing prophylactic antenatal corticosteroids with no treatment given before elective caesarean section C/S.
Results: A total of 560 patients of 5421 who underwent elective caesarean section C/S in 2013, were randomly selected, 281 (50.2%) were treated by 12 mg dexamethasone, two doses 12 hours apart, and 279 (49.8%) were in the control group. 26 infants were admitted to nursery there were 8 new-borns from the treatment group, and 18 from control group, with regards to indication of admission; those who had Respiratory distress (RDS) in the control group were 6 (2.2%),and in the treatment group were 2(0.7%), Transient tachypnea of the newborn( TTN) in the control group were 12 (4.3%), in the treatment group were 6(2.2%), (P value 0.00), (RR: 0.6 for TTN & 0.25 for RDS). Stay in special babies care unit (SBCU)<24 hours were 6 (2.2%) in control group and 8 (2.8%) in the treatment group, stay>24 hours were 12 (4.3%) in the control group and zero in the treatment, (P value was 0.026). 3 (1.1%) needed assisted ventilation, one death found in the control group (0.4%).
Conclusion: Giving dexamethasone, two before elective C/S had a significant reduction in the respiratory morbidity and decrease hospital study. It has no adverse effect and can be safely used.
<Keywords: Corticosteroid administration; Respiratory morbidity; Sudanese
In recent years, caesarean section rate has been increasing. It represents 30%-40% of births delivering methods [1], approximately half of which are elective caesarean delivery [2]. This may be due to changing practice in the management of previous caesarean and breech presentation as well as increased choice of women. Improved techniques of control of haemorrhage, infection, and thromboembolism have increased safety of the procedure. As a result obstetricians and pregnant women have reduced threshold for choosing it. However although maternal risks have decreased, the effect of surgical delivery on the baby before due date continues to be debated. Caesarean section is a risk factor for the development of neonatal respiratory complications, mostly respiratory distress syndrome (RDS) and transient tachypnoea of the new-born, both in term and preterm infants [3-6]. Infants born at term by caesarean delivery are more likely to develop respiratory morbidity than infants born vaginally, and this risk increases furthermore for the subgroup of children born after elective caesarean section, i.e. before onset of labour [4], with potentially severe implications [7]. The risk is decreasing with advancing gestational age, and infants born between 37+0 and 37+6 weeks are at 1.7 times more risk for respiratory complications than those born between 38+0 and 38+6 weeks, which in turn are at 2.4 times more risk than the infants born between 39+0 and 39+6 weeks [8]. If women were given two intramuscular injections of 12 mg of dexamethasone, two doses for 48 hrs. The rates of admissions were 5.2 at 37 weeks, 2.8% at 38 weeks, and 0.6% at 39 weeks. Although none of the babies in the control group died, admission will increase parental anxiety, the cost to nursery unit and invasive procedures including artificial ventilation giving mothers dexamethasone, two doses before elective section halved neonatal morbidity. So should we give steroids to mothers before delivery? Five studies lasting between three and 20 years with more than 1500 patients have shown no adverse effect of single course of antenatal corticosteroid, neither through infection of the fetus or mother nor in long term neurological or cognitive effect [9,10].
In view of this evidence, it is currently recommended that elective caesarean section should be deferred to 39 weeks [11]. However approximately 10%-15% of woman planed for c/s may deliver before 38 weeks, and there may be concern on waiting in the presence of specific indications or previous history. Respiratory morbidity in cases of term elective caesarean birth appears to have a different pathophysiology than in preterm birth, and retention in the lungs being the most likely cause. Interestingly, recent evidence indicates that apart from the traditional mechanical concept of vaginal squeeze, molecular mechanisms (predominantly lung epithelial sodium channels promote alveolar fluid drainage, and these channels are under active in fetuses unexposed to the process of labor. Glucocorticoid appears to increase the number and the function of thyroid hormones, providing a rational for their exogenous administration in cases of elective caesarean delivery. The objective of this study was to study the effect of corticosteroid administration 48 hrs before caesarean section on respiratory morbidity in infants born at term by elective caesarean.
Study population
The study was conducted at Omdurman Maternity Hospital, which has been and remains to be the largest specialized maternity hospital in Sudan. It conducts over 36,000 deliveries (normal vaginal deliveries and caesarean sections) annually.
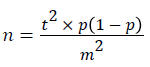
The study included women who underwent elective caesarean section at complete 37+0 to 39 weeks. The samples sizes were calculated using the below formula:
Descriptions:
n = required sample size.
t = confidence level at 95% (standard value of 1.96).
p = estimated prevalence.
m = margin of error at 5% (standard value of 0.05).
560 patients out of 5421, who underwent elective caesarean section C/S in the period from July 2013 to January 2014, were randomly selected. Inclusion criteria for the case and control groups were the same which included: Women with singleton pregnancies at term (complete 37+0-39 weeks); under regional anaesthesia, and only women with confirmed dates (early ultrasound scan 1st and 2nd trimester, or sure about LMP). It was a randomized controlled trial comparing prophylactic antenatal corticosteroid administration with no treatment given before elective caesarean section at term (at or after 37+0 weeks of gestation). It was a randomized controlled trial comparing prophylactic antenatal corticosteroid administration with no treatment given before elective caesarean section at term (at or after 37+0 weeks of gestation). It was a randomized controlled trial comparing prophylactic antenatal corticosteroid administration with no treatment given before elective caesarean section at term (at or after 37+0 weeks of gestation). Prophylactic maternal corticosteroid administration was in the form of dexamethasone two doses of 12 mg intramuscular, 12 hours apart 48 hours before elective caesarean section compared to no treatment.
Study period
This study was conducted during the period from July 2013 to January 2014.
Exclusion criteria
Were also the same in both groups, and included: Women with DM, women with congenital malformed babies, IUGR, women less than 37 weeks, multiple pregnancies, Women who received dexamethasone, two doses during pregnancy due to other causes, and women who refused this intervention.
Sampling technique
Two doses of dexamethasone, two doses 12 mg were given intramuscular, 12 hours apart, 48 hours before elective caesarean section. The mothers, who fulfilled the criteria, were given numbers e.g. 1, 2, 3...etc... To the mothers, the odd numbers were taken as cases, and even numbers as controls.
Data collection: Data was collected by structured questionnaire; during the preparation for the elective caesarean section, assessing the babies after delivery and following babies during their admission in the neonatal unit. Dexamethasone, two doses 12 mg two doses intra muscular, and Questionnaire, which included maternal antenatal care, maternal data, use of dexamethasone, timing of El C/S and infants data sex, and age. After delivery the infant was assessed using Apgar score, admission to neonatal unit, development of TTN or RDS, duration of stay in neonatal unit.
Ethical clearance
Approval of the study was obtained from the ethical committee and permission to conduct study was obtained from the administration of Omdurman Maternity Hospital, which consist of seven consultants in the field of obstetrics’, written consent was obtained from each respondent.
The demographic characteristics of patients in the study group and control are nearly comparable as shown in (Table 1).
| Information | Dexamethzone Frequency | Percentage (%) | ||||
|---|---|---|---|---|---|---|
| Control | Treatment | Total | Control | Treatment | ||
| Age | <19 | 6 | 3 | 9 | 2.20% | 1.10% |
| 20-30 | 137 | 125 | 262 | 49.10% | 44.50% | |
| 31-40 | 130 | 147 | 277 | 46.50% | 52.30% | |
| >40 | 6 | 6 | 12 | 2.20% | 2.10% | |
| Total | 279 | 281 | 560 | 100% | 100% | |
| Occupation | Employer | 29 | 22 | 51 | 10.40% | 7.80% |
| House wife | 250 | 259 | 509 | 89.60% | 92.20% | |
| Total | 279 | 281 | 560 | 100% | 100% | |
| Education | illiterate | 9 | 5 | 14 | 3.20% | 1.80% |
| Primary | 33 | 38 | 71 | 11.80% | 13.50% | |
| Secondary | 143 | 154 | 297 | 51.30% | 54.80% | |
| University | 94 | 84 | 178 | 33.70% | 29.90% | |
| Total | 279 | 281 | 560 | 100% | 100% | |
| Parity | Primigravida | 27 | 26 | 53 | 9.70% | 9.30% |
| MultiPara | 219 | 242 | 461 | 78.50% | 86.10% | |
| Grand MultiPara | 33 | 13 | 46 | 11.80% | 4.60% | |
| Total | 279 | 281 | 560 | 100% | 100% | |
Table 1: Distribution of women who underwent elective cesarean delivery at term according to sociodemographic data, at OMH, 2013.
Dexamethasone was given to 281 cases, which represents the treatment group, while 279 cases didn’t have it, representing the control group. Gestational age at delivery was similar in the two groups, also the fetal weight at delivery was nearly equal and no significant difference was found between fetal weight in patients treated with dexamethasone and those not treated.
Gender distribution showed 133 (52.4%) males in the control group against 121 (47.6%) in the treatment group, females represented 146 (47.7%) in the control group against 160 (52.3%) in the treatment group. About 96% of treated babies had Apgar score of 10 at 5 minutes while 93.9% in the control group. Sign of respiratory morbidity indicated by grunting was found in 12 (4.3%) cases of the control group, and in 5 (1.8%) of in the treatment group. There was recession in 5 (1.7%) of the control group, and no case in the study group, tachypnea in 4 (1.4%) of the control group and none in the study group.
At GA of (37+0-37+6) weeks, the admission was 10 cases in the control group and 3 cases in the treatment group. At GA of (38+0-38+6) weeks, the admission was 11 cases in the control group and 2 in the treatment group, while there was no admission at GA of (39+0-39+6) weeks.
Length of stay in the SCBU shows that, patients who stayed for less than 24 hours were 9 in the control group and 5 in the treatment group. Those who stayed more than 24 hours in hospital were 12 in the control, group and 0 (0.0%) in the treatment group (Table 2).
| Information | Dexamethzone Frequency | Percentage (%) | ||||
|---|---|---|---|---|---|---|
| Control | Treatment | total | Control | Treatment | ||
| 5 minute | 5 minute | 5 minute | 5 minute | 5 minute | ||
| APGAR Score | 5 | 1 | 1 | 2 | 0.40% | 0.40% |
| 6 | 2 | 1 | 3 | 0.70% | 0.40% | |
| 7 | 5 | 1 | 6 | 1.80% | 0.40% | |
| 8 | 7 | 8 | 15 | 2.50% | 2.80% | |
| 9 | 2 | 0 | 2 | 0.70% | 0.00% | |
| 10 | 262 | 270 | 538 | 93.90% | 96.00% | |
| Total | 279 | 281 | 560 | 100% | 100% | |
Table 2: Distribution of neonates from women who underwent elective cesarean delivery according to Apgar score, at OMH, 2013.
Incidence of respiratory distress morbidity post elective CS at term newborns is increasing. This is because of increased incidence of elective CS. The current study is an attempt to assess how far corticosteroids could affect the incidence of TTN, RDS, post elective caesarean section, and its impact on consequences e.g. hospital stay and severity of RDS and TTN.
This comprehensive study was done on 279 controls and 281 cases (treatment), which was done through random selection considering nearly equal sizes. The two compared groups however, did not differ significantly with regards to age, occupation, education, parity, and the attendance of antenatal care (ANC) unit.
The study findings showed the incidence of TTN to be 4.3% out of 279 cases in the control group, versus 2.1% out of 281 cases in the treatment group (RR=0.6). RDS was found to be 2.2% in the control group and 0.7% in the treatment group (RR:0.25). This obviously reflects a decrease of both TTN and RDS the group treatment by dexamethasone. Admission association with dexamethasone showed significant association (P value=0.033). This is comparable with the findings of a study conducted in UK in 2005 which revealed that: 19 control babies had transient tachypnea and five had respiratory distress syndrome (RDS), in comparison to ten treated babies with transient tachypnea and one with RDS [12].
Admission to the SCBU was also found less among the treatment group when compared to the control group, many studies confirmed such variation. Cochrane Pregnant and Childbirth group trial in 2009 revealed significant decrease in admission to SCBU with respiratory morbidity (RR-15, CI 0.3-64) [13]. A local study in Sudan conducted by Nogod F in 2011 also found significant results; 9 (7.3%) cases admitted in control versus no admission in case group (P value 0.04) [14].
There was no admission at the 39th week. This permits increasing the gestational age up to 39 week which is more effective than giving dexamethasone injection. A Chinese study in Hong Kong among 31420 cases found that, the risk for transient tachypnea of the newborn was significantly increased in those delivered by elective Caesarean section between week 37 and week 38+0/38+6 in the total population, while the increase in the Chinese was statistically significant only for deliveries before 38 weeks of gestation [15].
With regards to clinical diagnosis with symptoms and signs of respiratory distress morbidity, a decrease in cases with signs of grunting, recession and tachypnea was noticed among the treatment group. The correlation showed a significant association between respiratory signs and gestational age (GA) at the time of elective C/S (P value=0.000).
The length of admission was evaluated in the control group showing that 12 cases (4.3%) stayed for more than 24 hours and no case (0.0%) stayed in the treatment group for this period. The length of admission was correlated to the control and treatment groups, and it showed a significant association (P value=0.026).
This is supported by findings of Peter Stutchfield and colleagues in 2005, which showed that, only two intervention babies received intensive care-one at level 1 for one day and level 2 (high dependency) for three days, the other at level 2 for one day. In contrast, 14 control babies received intensive care; three with respiratory distress syndrome required ventilation for two to five days and stayed 12 to 18 days. Antenatal dexamethasone thus substantially reduced resource use in special baby units [16].
Severity of cases admitted to the SCBU between the two groups might be indicated by more frequent need for assisted ventilation (Cpap) in the control group 3 cases (1.1%), in face by no case in the treatment group (0.0%). Other studies advices delaying delivery until 39 weeks, unless necessary, would seem a more prudent option than giving steroids whose long term safety, even as a single course, remains questionable and to decrease the steroids side effects [17] . Beside others minor side effect, increase cost, long hospital stay, and increase babies admission to hospital in their first year of age[18].
According to the findings of the current study, we conclude that, the use of antenatal corticosteroid 48 hours before elective C/S was found to reduce incidence of RDS, TTN post elective C/S. It also has an effect on decreasing the severity of RDS, and it reduces the rate of admission to SCBU and referral to intensive care unit. Delaying the elective C/S as late as possible up to 39 weeks appear to be more effective than giving dexamethasone. Dexamethasone is a safe, and drug can be used safely in two recommended doses 12 hours apart.