Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2023)Volume 14, Issue 4
Aim: To unveil the success rate of Conjunctival-Limbal Autograft with Marginal Tenon’s layer Excision (CLAG-MTE) on pterygium recurrence rate.
Materials and methods: This study is an interventional non-randomized, non-equivalent control group design. Data of 40 patients in Conjunctival-Limbal Autograft (CLAG) group and 38 patients in CLAG-MTE group retrospectively reviewed. Patients of the both series were selected from whose surgeries were performed from February 2008 to January 2015. The recurrence rate of CLAG and CLAG-MTE was compared. And also, the limbal-conjunctival series of some studies which reported a high success rate on recurrence rate and Hirst's preliminary series were included in this comparison.
Results: The recurrence rate was 5.1% (4 eyes) in the CLAG group and 0% in the CLAG-MTE group. The mean follow-up period was 21.1 ± 5.6 months in the CLAG group and 22.6 ± 6.8 in the CLAG-MTE group. In Fisher's Exact Test, the difference in recurrence rate between the CLAG and the CLAG-MTE groups was not statistically significant.
When all the series were compared by One-way ANOVA in respect to recurrence rate, significant differences were found between a numbers of them. CLAG series, still, were found successful like CLAG-MTE series. However, when they were compared with Hirst’s and Al Fayez’s series, CLAG-MTE series were found to be more successful than CLAG series. Also, in the means of plot analysis, the CLAG-MTE series were showing the lowest plot while the CLAG and Guler’s series were showing the highest plot. The other series especially the Hirst’s ranked in between.
Conclusion: CLAG-MTE is the most effective in preventing recurrence among the techniques which were compared in this study. Moreover, it is relatively easy and less invasive in comparison to Hirst's technique.
Conjunctival-limbal autograft; Pterygium; Recurrence; Tenon’s layer excision
CLAG-MTE: Conjunctival-Limbal Autograft with Marginal Tenon’s layer Excision; CLAG: Conjunctival-Limbal Autograft; PERFECT: Pterygium Extended Removal Followed by Extended Conjunctival Transplantation
The main complication of pterygium excision is recurrence. Recent clinical studies focus on the role of limbus in the prevention of recurrence [1,2]. Therefore, Conjunctival-Limbal Autograft (CLAG) is the most preferable technique for prevention of pterygium recurrence. The reported recurrence rate ranges from 1 to 39%, and due to the short operative time required and the low recurrence rate [2-6] it is adapted worldwide [3,7].
But, Hirst offered a new approach [8]. He advocates that excision of Tenon’s layer is more important on pterygium recurrence than the role of limbus. It has a very low recurrence rate, but it is totally different from CLAG. In a population of 250 cases, he reported only one suspicious pterygium recurrence. Almost zero recurrence rate implies curability of pterygium. He calls his technique as Pterygium Extended Removal Followed by Extended Conjunctival Transplantation (PERFECT) [8]. In spite of zero recurrence rates, the PERFECT approach is technically challenging as it requires more invasive steps than the initial effect of pterygium on any eye.
Rectus muscle exposure on the pterygium area and excision of Tenon’s layer beyond the insertion of rectus are major challenges. The author proposes a different technique that is less invasive than Hirst’s approach with a similarly low recurrence rate. It is called as Conjunctival-Limbal Autograft with Marginal Tenon’s layer Excision (CLAG-MTE) [9].
The recurrence rate and complications of CLAG series were compared with series of CLAG-MTE. Also, some CLAG series were selected from literature which have the most low recurrence rate alongside the PERFECT series [3,5,8,10,11]. These selected series make a see-saw from CLAG to PERFECT. An argument is tried between recurrence rates of these series, so the aim is to unveil the overall success rate of the CLAG-MTE series on recurrence.
This is a single-center study and was carried out in a tertiary health facility. It is an interventional non-randomized, non-equivalent control group design. Patients of the both series are selected from whose surgeries were performed from February 2008 to January 2015. Patients with intermediate or fleshy (grade 2 or 3) pterygia were included. As most of these patients had previous surgeries in the fellow eye, or had the fellow eye operated by a different surgeon, only one eye from each patient was included in the study.
Institutional Ethics Committee of Diyarbakir Gazi Yaşargil Training and Research Hospital approved this study under approval ID of 218. The tenets of the Declaration of Helsinki were followed. Written informed consent was obtained from each patient.
Exclusion criteria are patients with atrophic pterygium (grade 1) and patients with other ocular pathologies except pterygium and cataract. In all the cases, the pterygium extension was at least 3 mm beyond the limbus. All the operations were done by the same surgeon. A randomised study could not be done due to human resource limitations. The patients in the CLAG group all had their surgeries prior to the innovation of CLAG-MTE. After the innovation of CLAG-MTE, CLAG-MTE was preferred.
Recurrence rate was the primary outcome measure. A new fibrovascular growth in the previous pterygium area was defined as recurrence [12]. A data questioning diplopia, occurrence of dellen, graft dislodgement, and infection were collected. Diplopia was inquired by the eye movements of the cases after the surgery.
Patients who underwent CLAG (n=40) are classified as Group 1, while patients who underwent CLAG-MTE (n=38) are classified as Group 2. Enrollment of patients in Group 1 was from February 2008 to May 2013. Enrollment of patients in Group 2 was from May 2013 to January 2015. The sample size of the both series was calculated based on results of the previous studies (0% vs. 10% recurrence rate). The minimum sample size with a power of 50% and 5% significance level was achieved. To decrease the risk of bias from a non-blinded study, the recurrence and complications post-surgery were assessed by one different observer per group and one same observer for the both.
The main difference in the surgical technique of CLAG-MTE from CLAG is the Tenon’s layer excision under free edges of the conjunctiva in the CLAG-MTE approach. Details of the CLAG-MTE technique was previously published [9]. Performed by the same surgeon, the total duration of operation of CLAG-MTE takes approximately 40 minutes, while CLAG takes approximately 35 minutes. The surgeries were performed under peribulbar anesthesia with 2 ml of 20 mg/ml lidocaine & epinephrine 0.0125 mg/ml mixture. A transverse transection was performed at the limbus to separate the head from the body of pterygium. For the graft preparation, the eye was turned down and a pair of radial incisions was made with a crescent knife in the intended graft area (encompassing approximately 1 mm larger area than the recipient bed) on the superior bulbar conjunctiva (Supplementary video file).
Post-operative treatment included the following: (a) Topical dexamethasone eye drop tapered in 45 days; (b) Antibiotic eye drop for 2 weeks; (c) Topical eye lubrication for 1 month; (d) Topical nonsteroidal antiinflammatory drug on the first day. Follow-up evaluation was done on 1st day, week, and month postoperatively and then monthly. Patients who failed to comply with the follow-up schedule were called for their post-operative reminder.
The recurrence rate of the CLAG and CLAG-MTE groups were compared. And also, the limbal-conjunctival series of a number of studies which reported a high success rate were included in this comparison. Hirst's preliminary series was included in this comparison, as well (Table 1). So by this comparison, a spectrum of those compared series’ success rate will be able to be drawn and the overall success of the CLAG-MTE will be able to be determined within the pterygial surgery.
| Series | Hirst | CLAG-MTE | CLAG | Al Fayez | Guler | Young | Arı |
|---|---|---|---|---|---|---|---|
| Number | 250 | 38 | 40 | 105 | 31 | 52 | 50 |
| Recurrence | 1 | 0 | 4 | 1 | 4 | 1 | 2 |
Table 1: Number of eyes included and number of recurrence in the series.
Statistical Package for Social Sciences (version 16.0; SPSS Inc, Chicago, IL) was used in statistical analysis. AP value<0.05 is considered significant. Parametric or non-parametric data were compared based on normality. Fisher's Exact Test was used for comparison of pre-operative characteristics and recurrence of the both groups. One-Way ANOVA test was used for analysis of statistically significant differences between the recurrence rates of all the groups. Levene's Test was used for equality of variances and Bonferroni was used as a post hoc tests.
Forty patients in the CLAG group and 38 patients in the CLAG-MTE group were included in this study. The patient characteristics for both groups were given in Table 2. The difference in the pre-operative characteristics of the patients in both groups were not statistically significant (p>0.05). There was one recurrent pterygium in each group. The prior operation was GLAG in both patients which were done by a different surgeon. All the other patients had primary pterygium. Follow-up was done for at least 12 months. The mean follow-up period was 21.1 ± 5.6 months in the CLAG group and 22.6 ± 6.8 months in the CLAG-MTE group. All operated pterygia were nasal (100%). The mean size of pterygium in the CLAG group was 3.8 ± 0.6 mm and in the CLAG-MTE group was 3.8 ± 0.7 mm in length.
| Parameter | CLAG (N=40; 51.3%) | CLAG-MTE (N=38; 48.7%) | Exact Sig. (2-sided) |
|---|---|---|---|
| Age | 44.6 ± 15.9 y | 43.7 ± 15.2 y | 0.985 |
| Gender (male/female) | 20/20 (25.6%/25.6%) | 20/18 (25.6%/23.1%) | 0.825 |
| Follow-up time | 21.1 ± 5.6 mo | 22.6 ± 6.8 mo | 0.36 |
| Ptergium size | 3.8 ± 0.6 mm | 3.8 ± 0.7 mm | 0.592 |
| Primary ptergium | 39 (50%) | 37 (47.4%) | 1.0 |
| Recurrent ptergium | 1 (1.3%) | 1 (1.3%) | |
| Laterality (right/left) | 20/20 (25.6%/25.6%) | 18/20 (47.4%/52.6%) | 0.825 |
| With recurrence | 4 (5.1%) | 0 (0%) | 0.116 |
| Without recurrence | 36 (46.2%) | 38 (48.7%) |
Note: CLAG: Conjunctival-Limbal Autograft, CLAG-MTE: Conjunctival-Limbal Autograft with Marginal Tenon’s layer Excision, y: years, mo: months, mm: millimeters, N: number of subjects.
Table 2: Demographic parameters and recurrence rate in the CLAG and the CLAG-MTE groups.
The recurrence rate was 5.1% (4 eyes) in the CLAG group and 0% in the CLAG-MTE group. The difference in recurrence rate between the CLAG and the CLAG-MTE groups was not statistically significant in Fisher's Exact Test (p>0.05). However, when one-way ANOVA was used (F(7.618)=4.674, p=0.000), surprisingly, significant differences were found between a number of them. When Hirst’s series were compared against all other series in the Bonferroni post hoc test, the CLAG series and Güler’s series showed a statistically higher recurrence rate. On the other hand, there was not any statistically significant difference between Hirst’s series and the CLAG-MTE series. When the CLAG-MTE group was compared against all the other series, only Güler’s series showed a significant difference in recurrence rate. All other series showed no significant differences. And when the CLAG group was compared against all the other series, Hirst’s and Al Fayez’s series showed a statistically significant lower recurrence rate. But the CLAG-MTE group did not show any statistically significant difference. So, the lowest plot was the CLAG-MTE series in the means. The highest plot was Guler’s series. The CLAG series showed the second highest recurrence level. Even though the CLAG-MTE series and the CLAG series were not statistically significant in Fisher's Exact Test, the CLAG-MTE series seemed the most successful and the CLAG and Güler’s series seemed the least successful in the means plot. All other series -including the Hirst’s- ranked in between (Table 3 and Figure 1).
| (I) groups | (J) groups | Mean Difference (I-J) | Std. Error | Sig. |
|---|---|---|---|---|
| CLAG | Al Fayez | 0.090* | 0.028 | 0.035 |
| Hirst | 0.096* | 0.026 | 0.005 | |
| CLAG-MTE | Guler | -0.129* | 0.036 | 0.011 |
| Al Fayez | CLAG | -0.090* | 0.028 | 0.035 |
| Hirst | CLAG | -0.096* | 0.026 | 0.005 |
| Guler | -0.125* | 0.029 | 0 |
Note: *The mean difference is significant at the 0.05 level.
Table 3: Benferroni post hoc test.
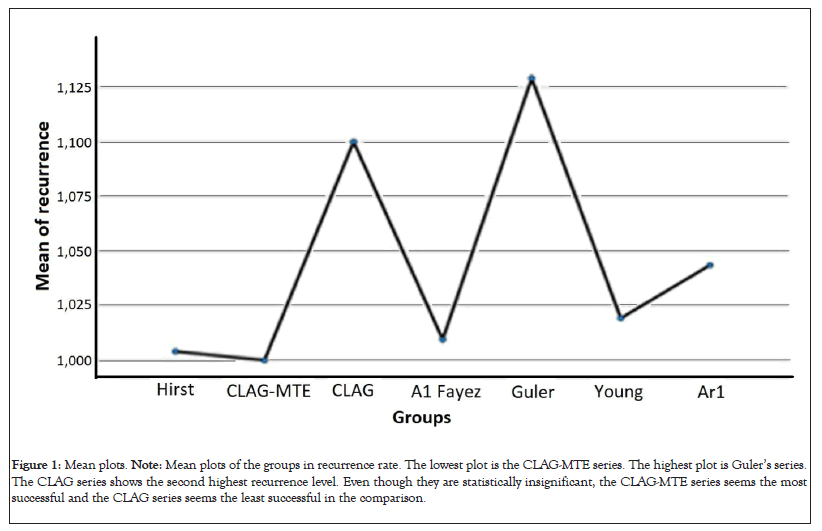
Figure 1: Mean plots. Note: Mean plots of the groups in recurrence rate. The lowest plot is the CLAG-MTE series. The highest plot is Guler’s series. The CLAG series shows the second highest recurrence level. Even though they are statistically insignificant, the CLAG-MTE series seems the most successful and the CLAG series seems the least successful in the comparison.
In terms of postoperative course of the CLAG and the CLAG-MTE group’s significant ocular pain was only reported on the first postoperative day. The patients were usually comfortable and the conjunctiva was quiet by the first postoperative week. None of the patients reported diplopia. Dellen developed in two patients in the CLAG group during their postoperative week 1 visit. In those patients, the edema of the marginal Tenon’s layer may have led to an irregular surface that disturbed tear distribution. There was no graft dislodgement and no granuloma development. One patient in each group developed a postoperative infection by the postoperative week 1 visit. The infections resolved after the patients were instructed to refrain from eye rubbing. The development of dellen and infection in both groups are not statistically significant (p>0.05). All patients were compliant to their post-operative follow-up visits.
Recently, Hirst reported an almost zero recurrence rate of pterygium with a completely new approach of excision [13]. However, this technique may be too risky for a pterygium excision due to the interference of the underlying rectus muscle and removing the Tenon’s layer above the rectus muscle. The Tenon’s tissue around and above the recti muscle constitutes the Tenon’s capsule pulley [14]. These pulleys are believed to be the functional origin of the recti muscles [14,15]. As a result of the interference of the Tenon’s layer, and subsequently the Tenon’s pulley, transient diplopia making driving impossible was reported by Hirst himself in almost all patients [8]. Diplopia, even if transient, is an unacceptable risk. Hirst’s PERFECT technique is also associated with a longer recovery time for patient and is more time-consuming for surgeon [8]. These are the challenges associated with using the PERFECT technique for a routine pterygium surgery. Hirst avoided using limbal tissue. He did report that using limbal tissue may cause limbal stem cell insufficiency in the graft site. But this opinion is also arguable. There had been no report of limbal stem cell insufficiency in the published literature on CLAG [3-7,12]. Since Tenon’s layer removal and limbal graft have separate effects on the prevention of pterygium recurrence, combining the two has an additive effect. However, the minimal amount of Tenon’s layer to be removed has not been determined, yet. Although there is agreement with Hirst about Tenon’s layer removal, ruining Tenon’s capsule pulley is so invasive. So the goal is to achieve the maximum benefit and the lowest recurrence rate without interfering with the Tenon’s capsule pulley.
The CLAG-MTE group has a recurrence rate of 0%. Besides its success, the CLAG-MTE technique offers advantages that are similar to the CLAG technique. First, the CLAG-MTE technique respects the anatomical tissues. Only a 2 to 3mm margin of Tenon’s layer is removed circumferentially around the border of the body of the pterygium. In the medial border of the pterygium, the excision extends only up to the insertion of the medial rectus. Tenon’s capsule pulleys are not touched as in CLAG. While Hirst obliges to reconstruct the semilunar fold, the CLAG-MTE is done far from semilunar fold. So it does not involve semilunar fold. The surgery involves only the ocular surface, which is easily visible. Second, the operative time to perform the CLAG-MTE is reasonable. Compared to Hirst’s PERFECT technique, the CLAG-MTE only takes 40 minutes to perform. This is only a few minutes longer than the 35 minutes which it takes to perform the CLAG. The post-operative recovery for the patient is faster. These advantages give more satisfaction to surgeons and to patients (Figure 2) [16].

Figure 2: Clinical image of 22nd case in CLAG-MTE series. Note: The right image shows intraoperative pterygium. The middle image belongs to the last follow-up which is 21 months in this patient. The left image is taken after 7.5 years during the examination of the patient for complaint blurred vision on his right eye.
The limitations of this study are its non-randomized design and retrospective nature, and the relatively small sample size. However, the sample size in this study is larger than a number of the reported series on CLAG. The strength of this study is the longer postoperative follow-up time. If the technique tends to fail in preventing recurrence, the follow-up time in this study is enough that virtually all recurrences can be identified. Conjunctival-Limbal Autograft with Marginal Tenon’s layer Excision (CLAG-MTE) is a relatively easy and less invasive procedure in comparison to Hirst's technique with a low recurrence rate for pterygium excision. It is also very easy to get accustomed to CLAG-MTE for surgeons who choose to use conjunctival-limbal autograft in their pterygium treatment practice.
Funding/support; None
Financial disclosures; None
The English language was edited by Dr Honeylon Teo who was a clinical fellow in ocular oncology in Kellogg Eye Institute. We appreciate her work.
The recurrence and complications post-surgery were assessed by Dr Leyla Ciftci, Dr Eyyup Dogan, and Dr Umut Dag. I appreciate their effort.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ciftci S (2023) Effect of Marginal Tenon’s Layer Excision for Pterygium Treatment: A Non Randomized Comparative Study. J Clin Exp Ophthalmol. 14:952.
Received: 26-Jun-2023, Manuscript No. JCEO-23-24317; Editor assigned: 28-Jun-2023, Pre QC No. JCEO-23-24317 (PQ); Reviewed: 12-Jul-2023, QC No. JCEO-23-24317; Revised: 19-Jul-2023, Manuscript No. JCEO-23-24317 (R); Published: 27-Jul-2023 , DOI: 10.35248/2155-9570.23.14.952
Copyright: © 2023 Ciftci S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.