Journal of Yoga & Physical Therapy
Open Access
ISSN: 2157-7595
ISSN: 2157-7595
Research - (2019)Volume 9, Issue 3
Objective: To investigate the dynamic postural control and level of functional abilities with and without ankle foot orthosis in ambulatory children with cerebral palsy.
Method: 32 children with spastic cerebral palsy (CP) were selected based on the inclusion criteria in two groups: Children who were using DAFOs and children who had never used DAFOs. Two dynamic activities of sit to stand and forward reach were performed by children of both the groups on force plat form for the assessment of dynamic postural control and their level of functional abilities were scored using Paediatric Evaluation of Disability Index (PEDI) by parental report.
Results: The dynamic postural control using force platform showed lesser COPE in children with CP who were using DAFOs compared to children in other group for sit to stand and forward reach activities respectively (p=0.003; p=0.423). PEDI score was higher in children who were using DAFOs compared to children without DAFOs. The correlation of dynamic postural control with their level of functional abilities was non- significant for both the groups.
Conclusion: Children with spastic CP who are using DAFOs more than a year had better dynamic postural control and functional abilities compared to children without DAFOs.
Postural control mechanism is an integral part of all motor abilities for purposeful movements and functional skills in routine activities of daily life [1,2]. These mechanisms include Postural stability; the ability to maintain Centre of mass (COM) within the limits of the Base of support (BOS) during static or dynamic activities. In postural orientation and postural equilibrium, coordination of movement strategies helps to stabilize the COM during both selfinitiated and externally triggered disturbances of stability [3-6]. The postural control mechanism is also necessary to recover balance and also adapt to changing environmental demands [5,7].
Postural control deficits are common in children with cerebral palsy (CP). The ability to maintain a stable posture demands complex interactions between sensory- motor system, CNS and musculoskeletal system. In children with CP, these mechanisms are affected, that may lead to impairment in postural control [3,8- 11]. Earlier studies on the postural control dysfunction in children with CP had found deficits in postural adjustment strategies (both anticipatory and reactive postural responses), difficulty to control body’s position in space, poor alignment between body segments and maintenance of Centre of Pressure (COP) within the limits of BOS [1,4,11-13].
Postural control deficits also limit the performance of children with CP in daily functional motor skills related to mobility, transfer and self-care [7,13,14]. Previous studies which have assessed their static and dynamic postural control during daily functional activities such as sit to stand and forward reach had showed higher values of postural oscillations measured in centre of pressure excursion (COPE) compared to healthy children [15-20]. Postural control deficits in Children with CP are an important contributing factor affecting their functional abilities. The Paediatric Evaluation of Disability Inventory (PEDI) is a standardized functional assessment measure to evaluate the actual ability of child to perform their daily necessary activities. It is used to measure functionality and caregiver assistance during the activities which they normally perform in their daily routine [21-23]. Studies have shown PEDI is a useful tool with good psychometric properties to describe the level of functional abilities in children with CP [24]. A recent study by Pavao have assessed the association between static postural control and functional abilities using PEDI in children with CP had found poor static balance control make them more dependent on caregiver [17].
AFOs are commonly recommended therapeutic intervention to improve the biomechanical orientation of body and functional capability in children with CP [2,25]. During upright posture, neuro-muscular forces of plantar flexors and dorsi flexors, helps in controlling the displacement of COP over the BOS during sit to stand and forward reach [26]. Studies have shown that dynamic AFOs (DAFOs) improves equal weight distribution in standing, performance time duration during sit to stand and reaching activity, dynamic postural control during gait in children with CP [27,28]. However, there are limited retrievable studies to assess the dynamic postural control during sit to stand and forward reach in standing in children with CP who are using DAFOs and who have not used DAFOs.
Subjects
Children clinically diagnosed with spastic cerebral palsy who were using DAFOs and who had never used DAFOs; within the age group of 5-12 years were included in study.
Total 32 children were included in study. Out of which 16 were using DAFOs for more than a year and 16 children had never used DAFOs. The demographic data of children participated in study are given in the Table 1.
Inclusion criteria of the study were as follows: Children with spastic CP
(i) Both
(ii) genders with age range of 5-12 years;
(iii) GMFCS
(iv) level I and II;
(v) Able to perform sit to stand from a chair without support and forward reach in standing without any assistance or lose of balance;
(vi) On observation showed Pes Equinus in walking;
(vii) Mini mental state examination (MMSE) of ≥ 23;
(viii) For DAFOs group those who were using DAFOs for more than one year.
Exclusion criteria were: Children with spastic CP
(i) History of orthopaedic surgical intervention involving Upper or Lower extremity in past 12 months;
(ii) Who had received Botox in last 6 months or on regular antispasmodic medications;
(iii) Severe Visual or Hearing deficits;
(iv) Fixed joint contracture or deformity in the lower extremity. The study protocol was approved by the Scientific Committee and Institutional Ethics Committee, KMC, Mangalore (MAHE) [IEC MLR 1115/264]. Parents of participants were explained about the study procedure in brief and on approval a signed inform consent was obtained.
Instrumentation
Dual Axis Force Platform (Model no. DFP4) manufactured by Biometrics Ltd. UK was used to assess COPE during both the dynamic activities of sit to stand and forward reach. The area of displacement was recorded with the help of computer attached to the force plate system. A Wooden bench (Width×Height×Length=1ft×1ft×3 ft) was used to make the child sit during performance of sit to stand task. For forward reach task an attractive toy was kept in front of child for the completion of forward reach task.
With the help of an inch tape the distance between child’s hand to a toy was been kept equal for all the participants. Paediatric Evaluation of Disability Inventory (PEDI), a scale consisting of three domains of self-care, mobility and social functions was used to measure functionality level of participants based on parental report. The total score of each component was considered for final correlation and comparison.
Permission from institution head was obtained and 48 children with spastic cerebral palsy were screened and 32 spastic cerebral palsy children were included in the study. Parents of participants were explained about the study procedure in brief and on approval a signed inform consent was obtained Baseline demographic data and GMFCS levels were collected by the tester.
For Dynamic Postural Control Assessment
To assess the dynamic postural control in children with spastic CP two dynamic activities; Sit to stand and Forward Reach in standing were selected, as earlier studies have suggested that these two activities are most commonly used activities in daily life. Before the actual testing procedure, proper explanation and demonstration for all the study participants was delivered by the tester. During testing, both the activities were performed in random orders with adequate rest periods of 5 minutes between them. To avoid anxiety and fatigue, the test procedures were carried out with parents/ caregiver guidance and also before the regular physiotherapy sessions. Participants in the DAFOs group were using outer shoe during test procedures while the children without DAFOs performed activities without shoe [29,30].
Force Plate Arrangements
Force plates were arranged on force platform as per the standard procedure given in the manual (Biometrics Ltd. UK). Children with spastic cerebral palsy were made to stand on force plates so that forefoot and hind foot of each foot was in contact with two parallel force plates for each leg.
Activity Performance
Children with spastic CP were facing towards the physiotherapist on Dual Axis Biometrics platform (Biometrics Ltd. UK). To alleviate anxiety a parent / a guardian was sitting behind the force plates during the test. Starting positions of each foot of child on force plate was noted. Each time starting position was the same. Each subject performed two practice trials to assure the cognitive idea of test procedure. During the procedure participants are encouraged to use their dominant hand to reach at self-selected velocity for an attractive toy placed in therapist’s hand at 10% more than the arm length. Standardised verbal instructions to reach for the toy were given for all the participants. During the performance of activity from standing to forward reach position the measure of COPE was measured. Following two trials of familiarization of test procedure three valid test measurements were measured and further considered for data analysis. It is indicated in Figures 1 and 2.
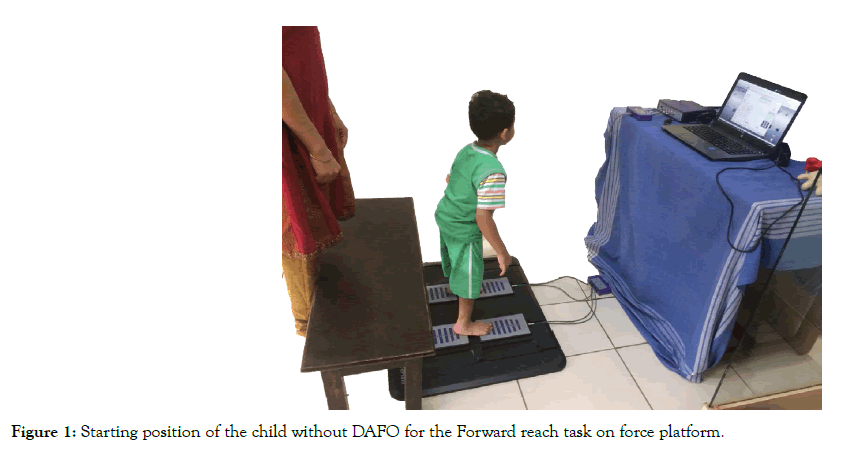
Figure 1: Starting position of the child without DAFO for the Forward reach task on force platform.
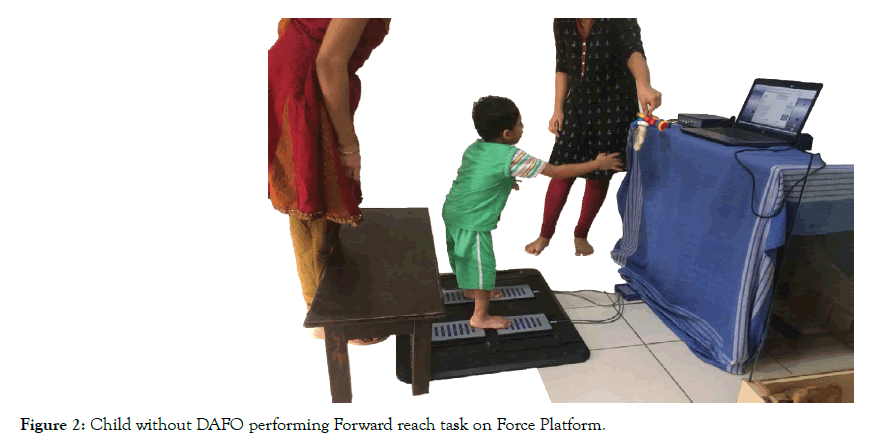
Figure 2: Child without DAFO performing Forward reach task on Force Platform.
Force Plate Arrangements
Dual Axis Force plates were arranged as per the standard procedure given in the manual. Children with spastic CP were made to sit in such a way that fore foot and hind foot of each foot was in contact with force plates on either side for each leg.
Activity Performance
At the beginning of activity children with spastic CP were seated on a wooden bench with hips, knees, and ankles at 90°; and the arms were rested on the thighs. Once seated, they were given standardised verbal instructions to assume an upright posture at a self-selected speed. Following two trials of familiarization of test procedure three valid test measurements were measured and further considered for data analysis. All the test outcome measures were collected by primary investigator. We also observed no adverse events during the test procedure. It is showed in Figures 3 and 4.
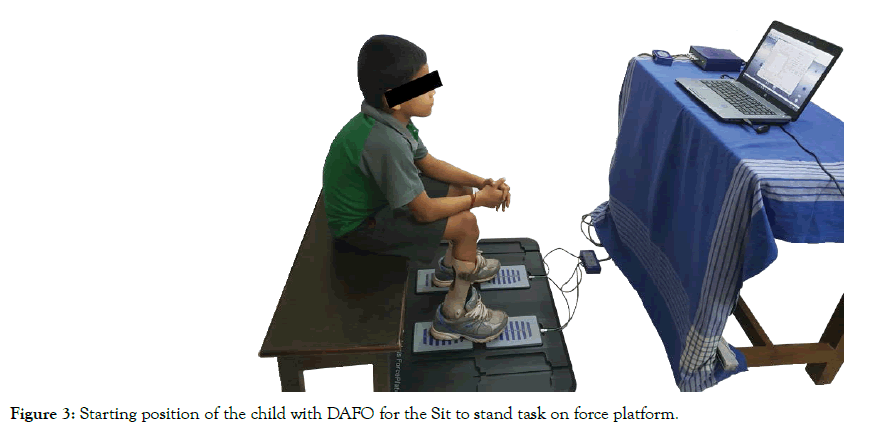
Figure 3: Starting position of the child with DAFO for the Sit to stand task on force platform.
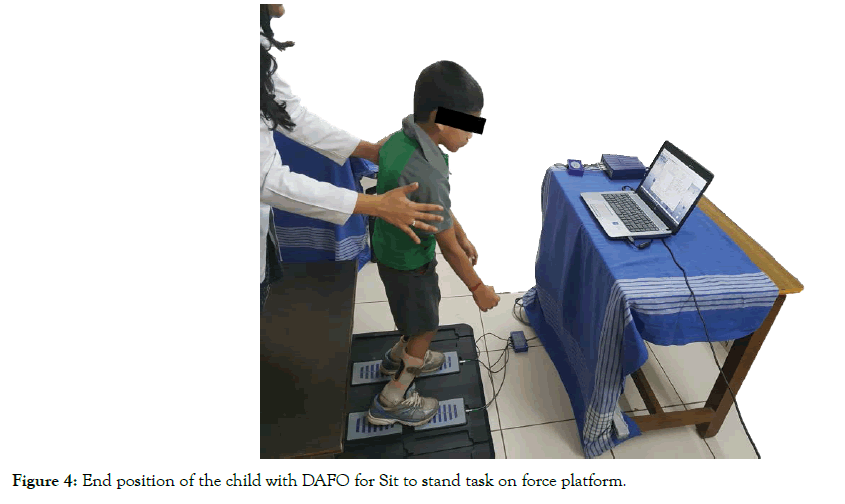
Figure 4: End position of the child with DAFO for Sit to stand task on force platform.
Children with DAFOs and without DAFOs were marked on PEDI scale based on parental report. Domains of scale were explained to parents by tester in their own language. Total scores for each child were noted for all three domains of PEDI.
Data collected were entered and analysed by the SPSS (statistical package for social science) version 16.0 for Windows (IBM). Descriptive statistics was used to analyse baseline characteristics for both the groups. Results of the test outcome measures were expressed as a summary measures (Median and Inter- quartile range) and presented with appropriate tables. Mann- Whitney’s U test was used to compare the summary scores between the groups. Pearson’s correlation test was used for analysing association between dynamic postural control and level of functional abilities among the groups.
p value of <0.05 was considered as statistically significant.
The study included 32 children with spastic CP, n=16 in each group of Children with DAFOs [Mean age 8.44 ± 2.33 years: 6 boys (37.5%); 10 girls (62.5%)] and without DAFOs [Mean age 9.25 ± 2.08 years: 11 boys (68.8%); 5 girls (31.3%)]. The children with CP who were using DAFOs included children with GMFCS level I [n=12; (75.0%)] and GMFCS level II [n=4; (25.0%)] with 5 (31.3%) children diagnosed with spastic hemiplegia and 11 (68.8%) were diagnosed with spastic Diplegia whereas the children with CP who had never used DAFOs were of GMFCS level I [n=3, (18.8%)] and GMFCS level II [n=13 (81.3%)] with 6 (37.5%) children diagnosed with spastic hemiplegia and 10 (62.5%) with spastic Diplegia. Table 1 summarizes the above findings.
| Characteristics | Children with DAFOs Mean ± SD / N (%) | Children without DAFOs Mean ± SD / N (%) |
|---|---|---|
| Age (Years) | 8.44 ± 2.33 | 9.25 ± 2.08 |
| Height (Cm) | 123.63 ± 8.52 | 126.13 ± 8.07 |
| Weight (Kg) | 21.13 ± 4.12 | 21.81 ± 4.62 |
| BMI (Kg/m2) | 13.76 ± 1.95 | 13.62 ± 2.00 |
| Boys | 6 (37.5) | 11(68.8) |
| Girls | 10 (62.5) | 5 (31.3) |
| GMFCS Level I | 12 (75.0) | 3 (18.8) |
| GMFCS Level II | 4 (25.0) | 13 (81.3) |
| Spastic Hemiplegic | 5 (31.3) | 6 (37.5) |
| Spastic Diplegic | 11 (68.8) | 10 (62.5) |
Table 1: Demographic characteristics of study participants (N= 16 in each group).
In children with spastic CP who were using DAFOs, COPE on force platform for the Sit to stand activity median value was 415.50 (328.50-540.75) mm2, while for Forward Reach median value was 276.50 (238.50-377.00) mm2; whereas in children with spastic CP who have not used DAFOs, COPE for the Sit to Stand activity median value was 598.50 (500.50- 692.25) mm2 and for Forward Reach median value was 300 (270.50378.00) mm2. Between the groups, the COPE is higher in children without DAFOs for both the activities and the difference is also found to be statistically significant for sit to stand activity as depicted in Table 2.
| Dynamic activities performed by children with Spastic CP | COPE (mm2) [Median (IQR)] | p- value | |
|---|---|---|---|
| Children with DAFOs (n=16) | Children without DAFOs (n=16) | ||
| Sit to Stand | 415.50 (328.50- 540.75) | 598.50 (500.50- 692.25) | 0.003* |
| Forward Reach | 276.50 (238.50- 377.00) | 300.00 (270.50- 378.00) | 0.423 |
| *Highly Significant | |||
Table 2: Summary of COPE values for both the groups.
On PEDI, domains of self- care, mobility and social function children with spastic CP who were using DAFOs scored 67.00 (57.25-68.75); 48.00 (44.50-50.00) and 60.50 (59.25-62.00) respectively; while children with spastic CP who were not using DAFOs had 44.50 (40.25- 60.50), 36.00(31.25- 40.00), 58.00 (46.75- 60.75) on same domains.
Children with DAFOs group had higher scores in all the PEDI domains and the differences between the groups had also found to be statistically significant as depicted in Table 3.
| PEDI domains | [Median (IQR)] | p- value | |
|---|---|---|---|
| Children with DAFOs (n=16) | Children without DAFOs (n=16) |
||
| Self-care | 67.00 (57.25-68.75) | 44.50 (40.25-60.50) | 0.001* |
| Mobility | 48.00 (44.50-50.00) | 36.00 (31.25-40.00) | 0.001* |
| Social function | 60.50 (59.25-62.00) | 58.00 (46.75-60.75) | 0.012* |
| *Highly Significant | |||
Table 3: Summary of Self-care, Mobility and Social function scores in PEDI for both the groups
Based on the correlation coefficients shown in Table 4, the results suggest that the correlation values for COPE in Sit to stand dynamic activity performed by children with CP who were using DAFOs on domains of PEDI were; Self-care 0.127 (p=0.638), Mobility 0.168 (p=0.533) and Social function -0.031 (p=0.909). Whereas for Forward Reach dynamic activity values with PEDI these were; 0.060 (p=0.826), -0.174 (p=0.519) and 0.107 (p=0.694) respectively.
| Variables | Children with DAFOs | Children without DAFOs | |||||
|---|---|---|---|---|---|---|---|
| Self-care | Mobility | Social function | Self-care | Mobility | Social function | ||
| COPE in Sit to stand activity | ƍ | 0.127 | 0.168 | -0.031 | 0.051 | -0.15 | -0.079 |
| p | 0.638 | 0.533 | 0.909 | 0.851 | 0.58 | 0.772 | |
| COPE in Forward reach activity | ƍ | 0.06 | -0.174 | 0.107 | -0.067 | -0.006 | -0.181 |
| p | 0.826 | 0.519 | 0.694 | 0.805 | 0.983 | 0.502 | |
| ƍ =Pearson’s correlation coefficient; p=Level of significance | |||||||
Table 4: Correlation of COPE with Self-care, Mobility and Social function domains of PEDI in both the groups.
The correlation values for COPE in Sit to stand dynamic activities performed by children who were not using DAFOs with PEDI for self-care 0.051 (p=0.851); mobility -0.051 (p=0.580); and for social function it was –0.079 (p=0.772). Whereas for forward reach dynamic activity these values were-0.067 (p=0.805); -0.006 (p=0.983) and -0.181 (p=0.502). For both groups results of all correlations are shown in Table 4.
The primary aim of this study was to assess the postural control during the dynamic activities in children with spastic CP who were using DAFOs and who had never used DAFOs and its related effect on functional abilities on PEDI. The results of the present study indicates that children with spastic CP using DAFOs had more effective dynamic postural control mechanisms measured in COPE and also better performance in PEDI compared to children without DAFOs. Between them, we also observed a statistically significant difference for COPE in sit to stand activity and all sub domains of PEDI score. However, these variables had found very weak correlation in our study participants (p>0.05).
Sit to stand and forward reach in standing are fundamental upright mobility activities which are widely performed in daily life [31- 37]. These activities demand higher levels of neuromuscular coordination and muscle strength which are necessary for postural stability and postural adjustments during the performance [38-40]. In children with spastic CP, studies have shown poor ankle motor control mechanisms which includes biomechanical mal-alignment in lower extremities leading to pes equines, altered muscle tone and length in plantar flexors as well as excessive sub-talar pronation had shown to influence the dynamic postural control mechanisms [18,41,42].
In our study children with DAFOs were using Double walled Dynamic Ankle Foot Orthosis made up of poly propylene with support strapping at sub-talar joint and foot arch modification. These support mechanism provides stabilizing control for sub talar mobility that aids them in their ability to actively control the alignment in foot and ankle complex as well as more even weight distribution to facilitate for better postural adjustments [43,44]. These findings could have contributed for lesser COPE in children with spastic CP who was using DAFOs. This is supported by Park et.al which showed during Sit to stand transfer activity, the children with spastic CP who were using AFOs where found to have better performance compared to children with CP without AFOs [45]. However, in their study they have taken the total time duration of the sit to stand performance compared to the present study.
According to the International Classification of Functioning, Disability and Health (ICF), the health status of individuals has multi-directional relationships between different domains of health. Based on the changes in body structure and function (such as deficits in postural control mechanisms as observed in CP) will affect their level of activity and participation restriction [46].
In our study children with DAFOs had better performance in selfcare, mobility and social function of PEDI domains. Some of the activities addressed in PEDI are challenged with postural control mechanisms which involves sit to stand and reach in standing activity. The participants in DAFOs group had lesser COPE which indicates they could have maintained successful postural stability to perform the daily routine task involving sit to stand and reach in standing. These further, could have an impact on their level of independence and also to explore the environment around them for active social participation. These findings are supported from a recent study by Pavao noted that children with CP having higher COPE during static standing found to have lower scores on Self-care and Mobility domains of PEDI [17]. As our participants were using AFOs more than one year, a recent study by Buckon et al. had reported that children with spastic CP shows functional benefit when they use AFOs for minimum period of 3 months regularly [47].
In our study, area of COPE had a very weak correlation with level of functionality for both the groups with p value > 0.05. Earlier studies on topographic distribution of CP with functional level had shown that gross motor abilities affect their self-care and daily mobility task. In our study 66% of participants were spastic diplegics and 34% were spastic hemiplegics could have resulted further present findings [14]. Other domains which may influence the functional abilities are level of intelligence, family support, community and socio-economic status which could have influenced our study results [48,49].
We also observed in DAFOs group 65% are girls and 75% of them were GMFCS level I. The group without DAFOs had 69% boys and 81% of them were level II. Hence, the results of the present study should be interpreted cautiously. Study findings are limited to GMFCS level I and II children with spastic CP. Muscle tone, Muscle length and Range Of Motions with respect to lower extremity were not considered. Physiotherapy interventions delivered in DAFOs group were not considered.
A cohort study design to find out the benefits of DAFOs in postural control mechanisms and its association with functional abilities in children with spastic CP. Age and Gender matched participants with identical GMFCS level may be considered for similar study design.
Children with spastic CP who are using DAFOs more than a year had better dynamic postural control and functional abilities compared to children without DAFOs.
Citation: Patel V, Kumar VK, Narayan A (2019) Postural Control and Level of Functional Abilities with and without Ankle Foot Orthosis in Ambulatory Children with Cerebral Palsy: A Cross Sectional Study. J Yoga Phys Ther 9: 300. doi: 10.35248/2157-7595.19.09.300.
Received: 12-Jul-2019 Accepted: 27-Nov-2019 Published: 03-Dec-2019
Copyright: Patel V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.