Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Review - (2019)Volume 7, Issue 3
Heart failure creates after some time as the heart's pumping activity becomes weaker. The condition can influence the right side of the heart only, or it can influence the two sides of the heart. Most cases include the two sides of the heart. Right-side heart failure happens if the heart can't pump enough blood to the lungs to get oxygen. Left-side heart failure happens if the heart can't pump enough oxygen-rich blood to whatever remains of the body. Rightside heart failure may make liquid develop in the feet, ankles, legs, liver, stomach area, and the veins in the neck. Right-side and left-side heart failure additionally may cause shortness of breath and weariness (tiredness).The driving reasons for heart failure are sicknesses that harm the heart. Examples incorporate Coronary Heart Disease (CHD), hypertension, and diabetes.
Coronary Heart Disease (CHD); High blood pressure; Diabetes; Abdomen
Congestive Heart Failure (CHF) is a chronic progressive condition that influences the directing energy of heart muscles. While regularly alluded to just as "heart failure," CHF particularly alludes to the phase in which liquid develops around the heart and makes it pump inefficiently [1,2]. The human heart has four heart chambers. The upper portion of the heart has two atria, and the lower half of the heart has two ventricles. The ventricles pump blood to different organs and tissues, and the atria receive blood as it circulates once again from whatever is left of the body [2].
Common types of CHF
Left-sided CHF is the most widely recognized sort of CHF. It happens when left ventricle doesn't legitimately pump blood out to the body [2]. As the condition progresses, fluid can develop in lungs, which makes breathing problems. A right-sided CHF ventricle has difficulty pumping blood to lungs. Blood moves down in veins, which causes fluid retention in bring down furthest points, stomach area, and other indispensable organs. It's conceivable to have left-sided and right-sided CHF in the meantime. For the most part, the disease begins in the left side and after that movement to one side when it's left untreated [3].
Causes of CHF
Risk for heart health problems, including high blood pressure (hypertension), coronary artery disease, and valve conditions etc.
Symptoms of CHF
In the early periods of chronic heart failure, the probably won't see any changes in health. As body condition get worse, Experience continuous changes in the body. Chest pain that radiates through the upper body can also be a sign of a heart attack. In the event that the patient encounters it or any of alternate indications that point to an extreme heart condition, please look for quick therapeutic consideration discussed in Table 1 [4-6].
| Symptom may notice first | Symptoms that indicate condition has worsened | Symptoms that indicate a severe heart condition |
|---|---|---|
| Fatigue | Irregular Heartbeat | Chest pain that radiates through the upper body |
| Swelling in ankles, feet, and legs | A cough that develops from congested lungs | Rapid breathing |
| Weight gain | Wheezing | Skin that appears blue, which is due to lack of oxygen in lungs |
| Increased need to urinate, especially at night | Shortness of breath, which may indicate pulmonary enema | Fainting |
Table 1: Symptoms of CHF (Chronic Heart Failure) are noticed and indicated.
Pathophysiology
Heart failure is a progressive disorder that is initiated after an event either damages the heart muscle, with resultant loss of functioning cardiac myocytes, or disrupts the ability of the myocardium to contract normally. This event may have an abrupt onset, as in the case of a myocardial infarction; a gradual onset, as in the case of hemodynamic pressure or volume overloading; or it may be hereditary [7]. The neurohormonal imbalance associated with chronic heart failure is a contributing factor to the progression of the disease. Overactivation of the Renin-Angiotensin-Aldosterone System (RAAS) and Sympathetic Nervous System (SNS), as well as other systems, contributes to cardiac remodeling and decline in heart function; the normal counter-regulatory beneficial effects of the Natriuretic Peptide System (NPS)—one of the most important counter-regulatory neurohormonal systems [8].
In addition, emerging research suggests that inflammation may play a role in the progression of structural heart failure and cardiac remodelling [8]. Circulating levels of pro-inflammatory cytokines including TNF and IL-6 are increased in patients with heart failure and correlate with adverse patient outcomes (Figure 1).
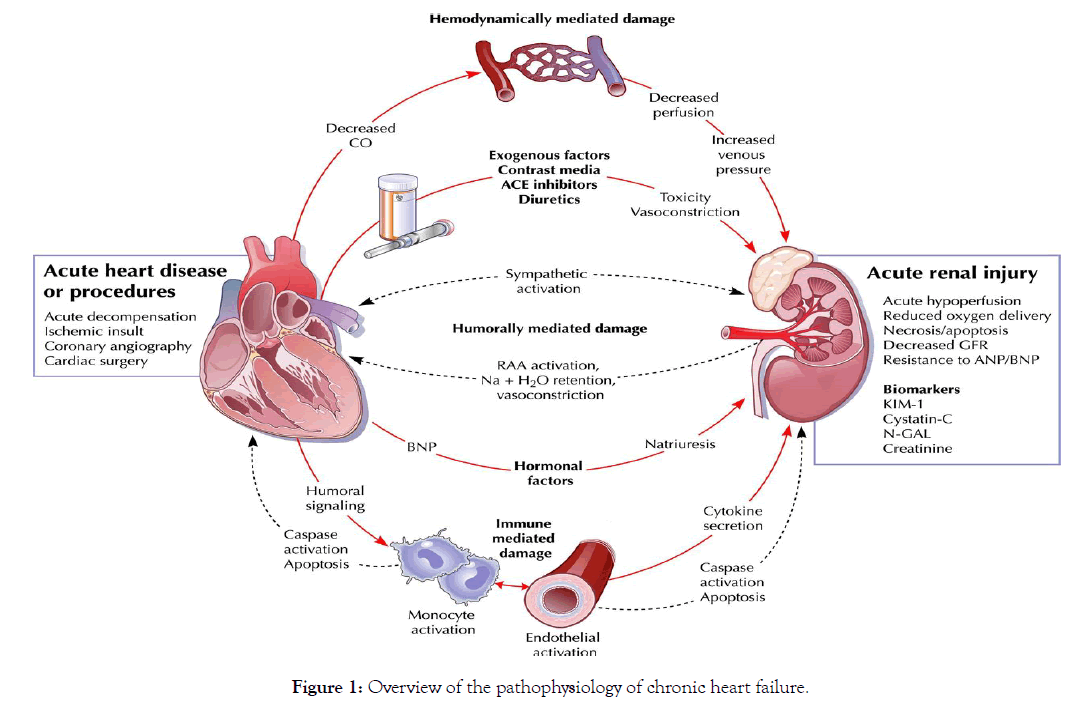
Figure 1: Overview of the pathophysiology of chronic heart failure.
Treatment of heart failure requires a multimodal approach. It involves a tight control over a combination of lifestyle modifications, medications and possibly the use of devices or surgery. As the condition progresses, doctors specializing in the treatment of heart failure can offer more advanced treatment options. The treatments are also changed with the changes in the stages of the disease [9-12].
Diet and lifestyle measures
The treatment of heart failure may include limits on the amount of fluids consumed (including alcohol) and reductions in dietary sodium (less than 2,000 mg per day). In addition, follow the doctor's instructions on getting regular exercise, which can help prevent symptoms from worsening. Patients with CHF are educated to undertake various non-pharmacological measures to improve symptoms and prognosis. Generally water intake should be limited to 1.5 L daily or less in patients with hypernatremia, though fluid restriction may be beneficial regardless in symptomatic reduction.
Medications with pharmacological management
There is a significant evidence–practice gap in the treatment of CHF; particularly the underuse of ACE inhibitors and β-blockers and aldosterone antagonists which have been shown to provide mortality benefit. Treatment of CHF aims to relieve symptoms, to maintain a euvolemic state (normal fluid level in the circulatory system), and to improve prognosis by delaying progression of heart failure and reducing cardiovascular risk. Drugs used include: Inhibition of Renin-angiotensin system, Beta-adrenoreceptor blockers, Diuretic agents, Vasodilator agents, Positive inotropes, and Aldosterone antagonists (e.g., Spironolactone). Some drugs which increase heart function, such as the positive inotrope Milrinone, lead to increased mortality, and are contraindicated [13].
Renin-Angiotensin system blockers: Angiotensin-Converting Enzyme (ACE) and inhibitors and Angiotensin II Receptor Blockers (ARBs).
ACE Inhibitors: Captopril, Enarpril, Fosinopril, Lisinopril, Ramipril, Quinapril & others.
Angiotensin-receptor blockers: Candesartan, Losartan, Telmisartan, Valsartan, Losartan.
Positive inotropic drugs: Positive inotropic agents are the chemically similar compounds which enhance cardiac muscle contractility and thus increase cardiac output and therefore, are widely used in treating CHF.
Digitalis: The cardiac glycosides are often called digitalis glycosides showing in (Figure 2).
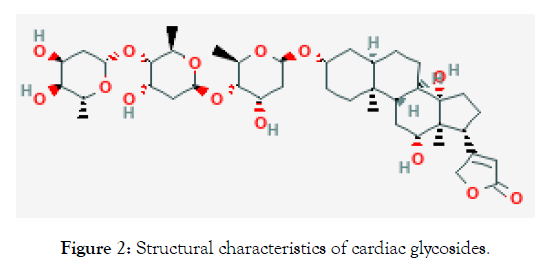
Figure 2: Structural characteristics of cardiac glycosides.
Dobutamine, the inotropic agent, Phosphodiesterase inhibitors such as Milrinone are sometimes utilized in severe cardiomyopathy.
Beta-adrenoreceptor blockers: Carvedilol, Atenolol, Nebivolol and extended-release metoprolol.
Diuretics:
Loop diuretics (e.g. Furosemide, Bumetanide)
Thiazide diuretics (e.g. Hydrochlorothiazide, Chlorthalidone, Chlorthiazide)
Potassium-sparing diuretics (e.g. Amiloride, Spironolactone, Eplerenone)
Vasodialator agents: The combination of Isosorbide dinitrate/ Hydralazine is the only vasodilator with proven survival benefits. Others vasodialators are Sodium nitroprusside, Nitroglycerine. Calcium channel blockers should be avoided in CHF patients.
Aldosterone receptor antagonists: Spironolactone is a direct antagonists of aldosterone, It should use for the most advanced cases of HF. Adverse effect include gastric disturbance, peptic ulcer, CNS effects such as lethargy, confusion, endrocrine abnormalities and menstrual irregularities.
Recombinant neuroendocrine hormones: Nesiritide.
Vasopressin receptor antagonists: Tolvaptan and conivaptan antagonize the effects of antidiuretic hormone (vasopressin).
CRT (Cardiac Resynchronization Therapy)
CRT is a clinically proven treatment option for some individuals with heart failure. A CRT device sends small electrical impulses to both lower chambers of the heart to help them beat together in a more synchronized pattern. This may improve the heart’s ability to pump blood and oxygen to your body [13-15].
CCM (Cardiac Contractility Modulation)
Cardiac contractility modulation is a name of a therapy developed by Impulse Dynamics NV, who implements the therapy within its implantable devices, under the brand name CCM™. This therapy is intended for the treatment of patients with moderate to severe heart failure (NYHA class II–IV) with symptoms despite optimal medical therapy who can benefit from an improvement in cardiac output in Figure 3. The short and long-term use of this therapy enhances the strength of ventricular contraction and therefore the heart’s pumping capacity by modulating (adjusting) the myocardial contractility.
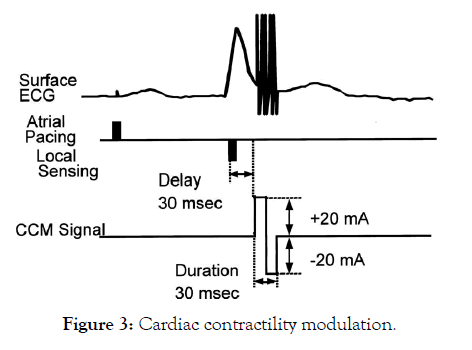
Figure 3: Cardiac contractility modulation.
AICD (Automated Implantable Cardioverter Defibrillator)
An Implantable Cardioverter-Defibrillator (ICD) or Automated Implantable Cardioverter Defibrillator (AICD) is a device implantable inside the body, able to perform cardioversion, defibrillation, and (in modern versions) pacing of the heart showing in Figure 4. "AICD" was trademarked by the Boston Scientific corporation, so the more generic "ICD" is preferred terminology.
Figure 4: A Guidant Corporation ICD device.
LVAD (Left Ventricular Assist Devices)
Another current treatment involves the use of Left Ventricular Assist Devices (LVADs). LVADs are battery-operated mechanical pump-type devices that are surgically implanted in the upper part of the abdomen. They take blood from the left ventricle and pump it through the aorta. LVADs are becoming more common and are often used in patients waiting for heart transplants.
Surgery is aimed at stopping further damage to the heart and improving the heart's function.
1. Bypass Graft
2. Coronary Artery Bypass Graft (CABG) Surgery
3. Valve Surgery
Newer procedures under examination are based on the observation that the spherical configuration of the dilated heart reduces ejection fraction compared to the elliptical form. Mesh-like constraint devices such as the Acorn CorCap aim to improve contraction efficacy and prevent further remodelling in Figure 5. Clinical trials are underway. Another technique which aims to divide the spherical ventricle into two elliptical halves is used with the Myosplint device.
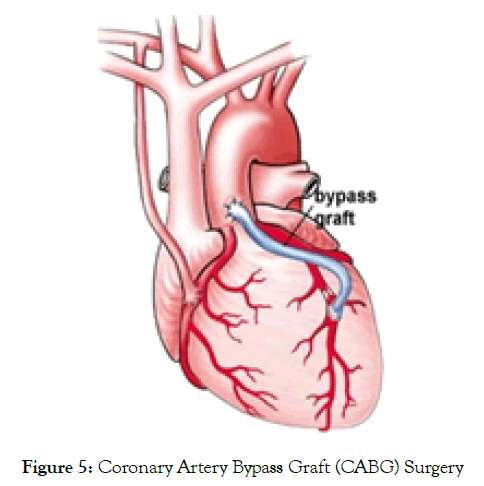
Figure 6: Coronary Artery Bypass Graft (CABG) Surgery
Each type of heart medications has different side effects.
Side effects of Angiotensin Converting Enzyme (ACE) inhibitors include cough, elevated blood potassium levels (hyperkalemia), low blood pressure, dizziness, headache, drowsiness, weakness, abnormal taste, and rash.
Taking vasodilators may cause lightheadedness or dizziness, increased or irregular heart rate, or headache. Side effects of calcium channel blockers include constipation, nausea, headache, rash, edema, low blood pressure, drowsiness, and dizziness.
Common side effects of beta blockers: Dizziness, Feeling tired, Worsening of usual symptoms, Stopping beta blockers suddenly can cause the symptoms to get worse. Don't stop taking medicine without talking to the doctor or nurse. Call doctor if, feel faint, pass out, have increased shortness of breath or wheezing, or have other symptoms that bother.
Aldosterone antagonist (Spironolactone, Eplerenone): These medicines prevent body from producing hormones that can damage heart. Common side effects of aldosterone antagonists: Changes in kidney function, increased potassium levels, swelling or tenderness in the breasts (in both men and women). The patient will have regular blood tests to check kidney function and potassium levels while taking this medicine.
Digoxin slows heart rate and improves the pumping ability of the heart. The patient will get a blood test to make sure the dose they are taking is right for them. Common side effects of digoxin: Nausea, Poor appetite, Digestive problems it also can cause notice a yellow tinge or "halos" in vision.
Get medical help immediately if patient has swelling of mouth, lips, or tongue. This could be an allergic reaction that can be lifethreatening [16].
July 7, 2015- The US Food and Drug Administration today approved Entresto (Sacubitril/Valsartan) tablets for the treatment of heart failure. The drug has been shown to reduce the rate of cardiovascular death and hospitalization related to heart failure. Heart failure is a common condition affecting about 5.1 million people in the United States. It is a condition in which the heart can't pump enough blood to meet the body's needs. Heart failure generally worsens over time as the heart's pumping action grows weaker. The leading causes of heart failure are diseases that damage the heart, such as heart attacks and high blood pressure. “Heart failure is a leading cause of death and disability in adults,” said Norman Stockbridge, M.D., Ph.D., director of the Division of Cardiovascular and Renal Products in the FDA’s Centre for Drug Evaluation and Research. “Treatment can help people with heart failure live longer and enjoy more active lives.” Entresto was reviewed under the FDA’s priority review program, which provides for expedited review of drugs that are intended to treat a serious disease or condition and may provide a significant improvement over available therapy. It was also granted fast track designation, which supports FDA’s efforts to facilitate the development and expedite the review of drugs to treat serious or life-threatening conditions and fill an unmet medical need. Entresto was studied in a clinical trial of more than 8,000 adults and was shown to reduce the rate of cardiovascular death and hospitalizations related to heart failure compared to another drug, enalapril. Most patients were also receiving currently approved heart failure treatments, including beta-blockers, diuretics, and mineralocorticoid antagonists. The most common side effects in clinical trial participants being treated with Entresto were low blood pressure (hypotension), high blood potassium levels (hyperkalemia), and poor function of the kidneys (renal impairment) [17].
Angioedema (an allergic reaction usually appearing as swelling of the lips or face) was also reported with Entresto; black patients and patients with a prior history of angioedema have a higher risk. Patients should be advised to get emergency medical help right away if they have symptoms of angioedema or trouble breathing while on Entresto. Health care professionals should advise patients not to use Entresto with any drug from the Angiotensin Converting Enzyme (ACE) inhibitor class because the risk of angioedema is increased. When switching between Entresto and an ACE inhibitor, use of the two drugs should be separated by 36 hours. Health care professionals should counsel patients about the risk of harm to an unborn baby. If pregnancy is detected, use of Entresto should be discontinued as soon as possible.
Entresto is manufactured by Novartis, based in East Hanover, New Jersey. The FDA, an agency within the US Department of Health and Human Services, protects the public health by assuring the safety, effectiveness and security of human and veterinary drugs, vaccines and other biological products for human use and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products [18].
Bristow says CRT is just the first wave of new devices designed for different aspects of heart-failure treatment. "They're working on anything we can imagine," he says. He mentions devices that will physically restrain the heart from enlarging -- a process that leads to worsening heart failure -- and others that will correct leaking heart valves. Devices like LVADs may offer a glimpse into heart-failure treatment for end-stage disease in the future. While stories about fully artificial hearts tend to grab headlines, such devices have limited use at this point. "The problem with the total artificial heart is that, as elegant as they have become, they still have to be absolutely flawless," says Rose. LVADs, which use technology to supplement the heart's natural function, may be a more realistic approach in the near future. "It's the best way to improve the quality of life for these people," Watson tells WebMD. "Although we talk about it a lot, our chances of making a bionic person are still pretty remote". Although devices are sometimes compared unfavourably with drugs because of their costs, many experts consider it a misleading comparison. Instead, devices and drugs will be developed to work together for heart-failure treatment. For instance, Bristow became involved in CRT not because of an inherent interest in mechanical devices, but because he thought that CRT had the potential to improve heart-failure treatment with medications called betablockers. Watson agrees and believes that heart-failure treatment with both drugs and devices will be important. "So far though, I don't think that there's been enough of a concerted effort to study the combination of drugs with devices," he says. "Most trials tend to look at one or the other."
Devices may turn out to be valuable apparatuses for executing promising new heart-failure medications, for example, cell implantation or gene therapy. What we do now is called latent scaffold to recuperation, where we put in the LVAD and expectation that whatever isn't right with the heart normally works itself out, I think what we'll find later on is dynamic scaffold to recuperation where, notwithstanding putting the device in, we'll oversee cells, or genes, or new or even old medications to help repair the heart. Once the treatment works, the device could be expelled. In the utilization of device treatment, two things are sure: The following decade will bring a large number of new devices for heart-failure treatment and they will be extensively littler and more refined than the ones now accessible. I think we've truly entered the time of Devices in heart failure.
Citation: Singh SK, Aswal N, Raza RR, Kumari R, Mondal D (2019) Conventional & Newer therapies of Chronic Heart Failure: A Literature Review. Angiol Open Access 7:232. doi: 10.35248/2329-9495.19.7.232
Received: 05-Apr-2019 Accepted: 19-Jul-2019 Published: 26-Jul-2019 , DOI: 10.35248/2329-9495.21.7:232
Copyright: © 2019 Singh SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.