Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2021)
Purpose: To evaluate how corneal epithelium thickness changes after myopic Photorefractive Keratectomy (PRK) relate to the magnitude of myopic correction, the diameter of the Optical Zone (OZ) and the incidence of regression in the early postoperative period.
Setting: Tertiary referral center
Design: Prospective longitudinal cohort study
Methods: Twenty-two eyes of 11 patients with mean manifest spherical equivalent of -4.75 ± 1.69 D underwent PRK between November 2016 and March 2017. Epithelial thickness profiles were evaluated preoperatively and at 1, 3 and 6 month’s postoperatively using ultra-high resolution anterior segment OCT. The relationship between post-operative epithelial thickness changes and the magnitude of myopic correction, the OZ diameter and the refractive outcomes was investigated prospectively.
Results: Central epithelial thickening progressed during the first three postoperative months (p=0.045, between first and third postoperative month) and stabilized thereafter (p=0.980, between third and sixth postoperative month). A corresponding myopic shift of 0.13 D and an increase in mean K by 0.65 D were observed at three months postoperatively, which remained stable thereafter and did not affect the final refractive outcomes (mean postoperative spherical equivalent 0.14 ± 0.40 D). Central epithelial thickness increased proportionally with the amount of myopia treated (r=0.41, p=0.04) and reversely with the ablation zone diameter (r=-0.39, p=0.04).
Conclusion: Corneal epithelial hyperplasia after myopic PRK is dependent on the preoperative myopic error and ablation zone diameter. Epithelial hyperplasia-induced regression did not have a negative effect on the overall refractive outcome.
Synopsis: The degree of epithelial thickening and hyperopic shift post-PRK depends on the preoperative refraction and the optical zone diameter. The subsequent regression does not negatively affect the refractive outcome.
Laser refractive surgery; PRK; LASIK; Epithelial thickness profile; Epithelial hyperplasia; Regression; Optical zone diameter
The corneal epithelium is a highly adaptive structure that aims not only to protect the cornea from external insults but also to maintain homogeneity of the optical system. Through changes in its thickness profile, the corneal epithelium reacts to underlying stromal asymmetries in order to reduce surface irregularities and, thus, maintain a smooth corneal surface. Such compensatory thickness changes have been reported in keratoconus, [1-6] dry eye [7,8] and post refractive surgery [9-13].
Initial evaluations of corneal epithelial thickness were performed using confocal microscopy 14 and very-high frequency (50 MHz) digital ultrasound biomicroscopy[14,15]. These techniques are rather invasive requiring direct contact with the ocular surface or immersion of the cornea in a liquid medium, respectively. The advent of high resolution anterior segment optical coherence tomography (HR AS-OCT) has made in vivo measurements of corneal epithelial thickness more accurate (axial resolution, 5 μm), reproducible and non-invasive [16,17].
HR AS-OCT has been used for the evaluation of the epithelial thickness profile deviations in ectatic corneas, where it reproducibly reveals epithelial thinning over the apex of the cone and thickening in areas around the cone [1-6]. In refractive surgery, HR AS-OCT imaging of the corneal epithelial thickness after myopic Laser Assisted in situ Keratosmileusis (LASIK) has shown progressive epithelial and flap thickening between the first and the third postoperative months [10,11] and in one report thickening continued to progress up to 1 year postoperatively [9]. Both in alcohol-assisted [12] and in trans-epithelial [13] myopic PRK, HR AS-OCT imaging of the corneal epithelium revealed comparable central (2 mm) and paracentral (2-5 mm) gradual corneal epithelial thickening over the course of 3 and 6 months respectively.
Herein we aim to assess changes in the epithelial thickness profile after alcohol-assisted myopic PRK using Ultra High Resolution Anterior Segment Optical Coherence Tomography (UHR AS-OCT) with an axial digital resolution of 3 μm. Our goal is to correlate such changes with the magnitude of the myopic correction, the optical zone diameter and the postoperative refractive outcomes. In the present study, excimer laser ablation was conducted using an aspheric aberration-neutral module.
Patients
Twenty-two eyes of eleven patients who underwent bilateral alcohol-assisted PRK between November 17, 2016 and March 15, 2017 were enrolled in the study. Exclusion criteria were age <18 years, ocular or systemic diseases, central corneal thickness <470 μm, irregular topography and history of prior ocular surgery. All patients had discontinued contact lens use 1 to 3 weeks prior to the preoperative evaluation depending on the contact lens type. The study protocol was approved by the Institutional Review Board of the University of West Attica and adhered to the tenets of the Declaration of Helsinki.
For statistical purposes all eyes were evaluated separately. At the preoperative evaluation the uncorrected and bestcorrected distance visual acuities were measured, manifest and cycloplegic refraction were performed and all patients underwent pupillography, double Scheimpflug tomography (Schwind Sirius; CSO, Florence, Italy), noncontact intraocular pressure measurement (Ocular Response Analyzer; Reichert, NY, USA), analysis of corneal hysteresis (Ocular Response Analyzer; Reichert, NY, USA), corneal pachymetry (Optovue Avanti RTVue XR; Optovue Inc., Fremont, CA) and epithelial thickness mapping (Optovue Avanti RTVue XR; Optovue Inc., Fremont, CA). Post-operative evaluations at 1, 3 and 6 months included uncorrected distance visual acuity, best-corrected distance visual acuity, manifest refraction, double Scheimpflug tomography, corneal pachymetry and epithelial thickness mapping.
Surgical technique
Alcohol-assisted myopic PRK was implemented with the Schwind Amaris excimer laser (Schwind Eye-Tech Solutions GmbH, Kleinostheim, Germany) using the aspheric aberrationfree module, formulated by the Schwind Amaris ORK-CAM. Aspheric ablation profiles balance the peripheral energy loss of the laser due to the increased angle of incidence on the cornea, thus minimizing the induction of spherical aberration that may affect the postoperative results.18 Both eyes of each patient were treated during the same surgical session, aiming at an emmetropic refractive outcome. The chosen optical zone diameter ranged from 6.5 mm to 7 mm as per surgeon preference and pupil diameter. The optimal transition zone (up to 1.5 mm) was estimated by the system’s software depending on the optical zone diameter and the pre-operative refraction.
All surgical procedures were performed by two surgeons (A.C. and G.C.) who followed the same protocol. The corneal epithelium was debrided after a 30-second exposure to 20% ethanol using a crescent blade. A 1050 Hz infrared eye-tracker, incorporated into the system and centered on the corneal vertex ensured proper alignment of the patient’s eye. Mitomycin-C 0.02% was applied for 30 s after the ablation, followed by irrigation of the stromal bed with balanced salt solution. A prophylactic, silicon-hydrogel bandage contact lens was fitted on the treated eye for 5 to 7 days. The postoperative regimen consisted of topical ciprofloxacin 0.3% drops until removal of the bandage contact lens a few and dexamethasone 0.1% drops tapered over 6 weeks.
UHR AS-OCT epithelial thickness mapping
Corneal pachymetry and epithelial thickness maps were generated using the UHR AS-OCT Avanti RTVue with an anterior segment corneal adaptor CAM-L (6.0-2.0 mm mode). This UHR AS-OCT device uses a 840 nm wavelength at a scan rate of 70,000 axial scans per second, a digital axial resolution of 3 μm and transverse resolution of 15 μm. Ultra high-resolution cross-sectional scans were used to cover the 6 mm diameter corneal surface in 8 vertex-centered meridians. Identification of the air-tear film and epithelium-Bowman layer interfaces was automatically performed by the integrated algorithm of the software. Cross-sectional scans were repeated 5 times and averaged to produce the pachymetry and epithelial thickness maps in color scale (Figure 1). The values from the epithelial thickness map used in the analysis included the central 2 mm diameter zone and the mid-peripheral 2-5 mm superior and inferior zones.
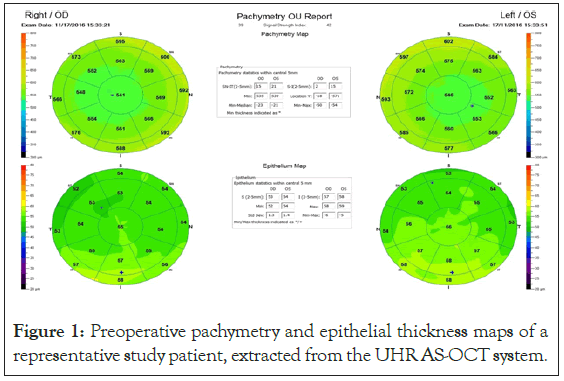
Figure 1: Preoperative pachymetry and epithelial thickness maps of a representative study patient, extracted from the UHR AS-OCT system.
Data analysis
Statistical analysis was performed using the SPSS, version 25 software (IBM Corp., Armonk, NY, USA). Mean values and standard deviation were calculated for continuous variables. The Shapiro Wilk test was employed to assess normality of the data. The paired t-test was used to evaluate the differences between the preoperative and postoperative manifest refraction and keratometry values. The Wilcoxon Signed-Rank test was used to assess the differences between the preoperative and postoperative epithelial and central corneal thickness values. The Kruskal – Wallis test was used for the comparison of the central 2 mm zone and the mid-peripheral 2-5 mm superior and inferior zone thickness deviations at different time points in the postoperative period. The Pearson correlation coefficient was used to evaluate correlations between the postoperative central epithelial thickness, the preoperative manifest refraction and the optical zone diameter. Linear regression analysis was used to demonstrate the impact of the preoperative manifest spherical equivalent magnitude on the postoperative central epithelial thickness. P-values less than 0.05 were considered statistically significant.
The mean age of the patients at the time of surgery was 26 ± 5.78 years (median, 26 years and range, 18 to 37 years). The preoperative myopic distribution was even among the patients from low to high and the mean preoperative spherical equivalent was -4.75 ± 1.69 D (median, -4.43 D and range, -8.37 D to -2.50 D). Table 1 summarizes the preoperative clinical features and postoperative outcomes, including the postoperative changes in Manifest Refraction Spherical Equivalent (MRSE) and in mean K as measured by double Scheimpflug tomography. At 1 month postoperatively, mean MRSE and mean K were 0.27 ± 0.52 D and 39.58 ± 1.83 D respectively. At 3 months, a small myopic shift (MRSE, 0.14 ± 0.51 D, p=0.002) along with corneal steepening (Mean K, 40.23 ± 1.95 D, p=0.004) was observed compared to the first postoperative month, which remained stable at the 6-month time point (MRSE, 0.14 ± 0.40 D, p=0.791 and mean K, 40.27 ± 1.84 D, p=0.921) (Figures 2 and 3).
| Parameters | |||
|---|---|---|---|
| N=22 | MRSE (D) | Mean K (D) | OZ (mm) |
| Preoperative | -4.76 ± 1.69 (-8.37 to -2.50) |
44.82 ± 1.72 (44.00 to 48.87) |
6.63 ± 0.29 (6.50 to 7.00) |
| 1 month postoperative | 0.27 ± 0.52 (-1.12 to 0.87) |
39.58 ± 1.83 (35.25 to 43.87) |
- |
| 3 months postoperative | 0.14 ± 0.51 (-1.00 to 0.75) |
40.23 ± 1.95 (35.50 to 43.12) |
- |
| 6 months postoperative | 0.14 ± 0.40 (-0.62 to 1.12) |
40.27 ± 1.84 (35.50 to 43.37) |
- |
Abbreviations: MRSE: Manifest Refraction Spherical Equivalent; OZ: Optical Zone Diameter. Results are displayed as mean ± SD (Standard Deviation) and range.
Table 1: Preoperative characteristics and clinical outcomes at 1, 3 and 6 months after alcohol-assisted myopic PRK.
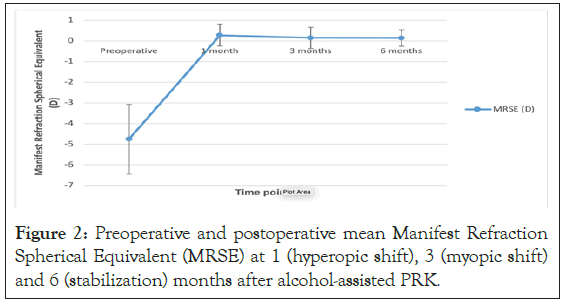
Figure 2: Preoperative and postoperative mean Manifest Refraction Spherical Equivalent (MRSE) at 1 (hyperopic shift), 3 (myopic shift) and 6 (stabilization) months after alcohol-assisted PRK.
Mean central corneal thickness (CCT) and Epithelial Thickness (ET) profiles, assessed by UHR AS-OCT preoperatively and over time are shown in Table 2. At 1 month postoperatively, statistically significant epithelial thickening was detected at the superior and inferior zones though not at the center of the cornea compared to the preoperative values (p=0.005, p=0.039, p=0.332, respectively). Non-parametric analysis revealed a trend for the inferior epithelium to be thicker compared to the superior one preoperatively (p=0.003) and during the postoperative period at 1 month (p=0.009), 3 months (p=0.003) and 6 months (p=0.012). Thus, the corneal epithelium continued to maintain the preoperative mid-peripheral epithelial profile pattern in the postoperative period. Additionally, regional analysis revealed the central epithelium to be thinner than the inferior one (p=0.005) and also thinner, though not significantly, than the superior (p=0.834) one at the 1-month time point (Figure 4). At 3 months postoperatively, statistically significant central epithelial thickening was detected (p=0.001) along with mild, though not significant, further thickening of the superior and inferior corneal epithelium (p=0.602, p=0.17, respectively) compared to the first postoperative month (Figures 4). Additionally, at the 3-month time point regional analysis revealed no significant difference between the central and inferior epithelial thickness (p=0.152) as well as between the central and superior epithelial thickness values (p=0.121) (Figure 4). At 6 months postoperatively, no significant change was noted in the central, superior and inferior epithelial thickness profiles compared to the third postoperative month (p=0.373, p=0,977 p=0.456 respectively), thus, suggesting stabilization of the central and mid-peripheral epithelial thickness remodeling (Figure 4).
| Parameters | ||||
|---|---|---|---|---|
| N=22 | CCT (μm) |
CET (μm) |
ET(S) (μm) |
ET(I) (μm) |
| Preoperative | 545.18 ± 26.07 | 51.77 ± 3.47 | 50.00 ± 4.20 | 53.54 ± 3.24 |
| 1 month postoperative |
464.90 ± 35.13 | 52.09 ± 3.70 | 53.42 ± 2.90 | 55.94 ± 3.80 |
| 3 months postoperative |
465.40 ± 35.25 | 54.50 ± 3.40 | 53.68 ± 3.38 | 56.44 ± 3.38 |
| 6 months postoperative |
468.66 ± 36.63 | 54.90 ± 4.46 | 53.63 ± 3.98 | 56.86 ± 3.48 |
Abbreviations: CCT: Central Corneal Thickness; CET:Central Epithelial Thickness (2mm), ET(S): Epithelial Thickness (Superiorly 2-5 mm), ET(I): Epithelial Thickness (Inferiorly 2-5 mm). Results are displayed as mean ± SD (Standard Deviation).
Table 2: UHR AS – OCT pachymetry and epithelial thickness profiles preoperatively and at 1, 3 and 6 months after alcohol-assisted myopic PRK.
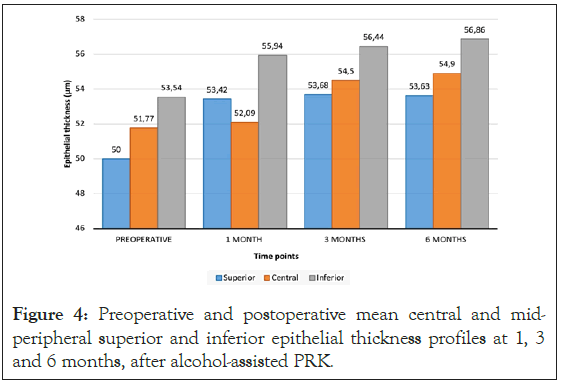
Figure 4: Preoperative and postoperative mean central and midperipheral superior and inferior epithelial thickness profiles at 1, 3 and 6 months, after alcohol-assisted PRK.
(flattening), 3 (steepening) and 6 months (stabilization) after alcoholassisted PRK. Corneal power was measured as mean keratometry readings via double Scheimpflug tomography.The residual stromal bed thickness for all patients was >300 μm after the procedure. The preoperative mean central corneal thickness of 545.18 μm was reduced at 1 month to 464.90 μm (p=0.001) and remained stable at 3 (465.40 μm, p=0.18) and 6 (468.66 μm, p=0.61) months after the ablation (Figure 5). A positive correlation was found between the magnitude of the preoperative myopic refraction and the central epithelial thickness at 3 and 6 months postoperatively (Pearson correlation coefficient r=0.41, p=0.04 and r=0.56, p=0.03, respectively). For every additional diopter of myopic correction, a central epithelial thickness increase of 1.004 μm was observed (Figure 6).
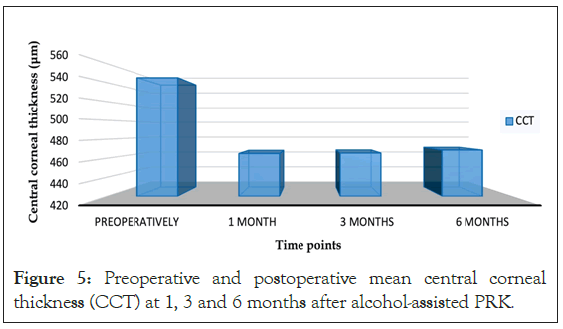
Figure 5: Preoperative and postoperative mean central corneal thickness (CCT) at 1, 3 and 6 months after alcohol-assisted PRK.
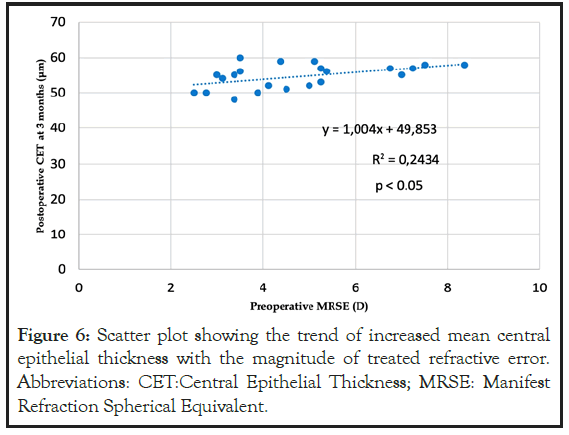
Figure 6: Scatter plot showing the trend of increased mean central epithelial thickness with the magnitude of treated refractive error. Abbreviations: CET:Central Epithelial Thickness; MRSE: Manifest Refraction Spherical Equivalent.
The mean optical zone diameter implemented during the procedure was 6.63 ± 0.29 mm (range, 6.50-7.00 mm). The total ablation zone was 8.08 ± 0.76 mm (range 7.39 – 9.00 mm). A negative correlation between the optical zone diameter and the postoperative central epithelial thickness was noted at 3 months after the procedure (Pearson correlation coefficient, r=-0.39, p=0.04), suggesting that a smaller optical zone diameter results in a thicker central epithelium.
This prospective longitudinal cohort study used UHR AS-OCT to investigate the epithelial thickness remodeling that occurs after epithelium-debridement myopic PRK with an aspheric aberration-neutral excimer laser module. We observed a statistically significant postoperative central epithelial thickening that correlated positively with the preoperative myopic refractive error and negatively with the optical zone diameter, along with a corresponding epithelial hyperplasia-induced regression that did not negatively affect the final refractive outcome.
In our study, UHR AS-OCT epithelial thickness analysis showed a mean preoperative Central Epithelial Thickness (CET) of 51.77 ± 3.47 μm (Table 2). Reinstein et al. used very high frequency ultrasound biomicroscopy to estimate the mean CET of a moderate myopic eye and obtained similar values of 51.79 ± 0.78 μm [18,19]. On the other hand, Erie et al. [14] and Patel et al. (2007) [20] used confocal microscopy and estimated considerably lower mean CET values of 46.00 ± 5.00 μm and 41.00 ± 4.00 μm respectively. This difference in mean CET values between our study and the ones using confocal microscopy can be attributed to thickness variations in the precorneal tear film, which is included in UHR AS-OCT measurements but not in the confocal microscopy ones, and can account for up to 5 μm of thickness variability [21]. Finally, the mean preoperative CET values recorded in our study with ultra-high resolution AS-OCT are similar to the ones recorded with high resolution AS-OCT in prior studies [9-13].
Our results suggest that the thickness of the corneal epithelium varies across the entire corneal surface. Mean preoperative CET was higher at the inferior zone compared to the superior one, resulting in a superior-inferior difference of -3.54 μm (Table 2). This epithelial thickness disparity along the superior-inferior vertical axis has also been noted in other series of HR AS-OCT studies [4,6,9-13,22] and may be explained both by the thicker tear film located inferiorly and integrated in both UHR AS-OCT and HR AS-OCT system measurements, and by the constant epithelium-reducing upper lid movement.
At 3 and 6 months postoperatively the superior and inferior epithelium thickness profiles demonstrated an epithelium distribution pattern comparable to the preoperative one along the vertical meridian (Table 2 and Figure 4). The postoperative UHR AS-OCT acquired pattern showed a thicker epithelium at the inferior zone compared to the superior area, in accordance with the previous HR AS-OCT studies on LASIK, [9-11] alcohol-assisted PRK [12] and transepithelial-PRK[13]. Significant epithelial remodeling was observed at the first postoperative month, likely due to the Schwind Amaris excimer laser aspheric aberration-free module, which leads to a greater peripheral than central tissue photoablation. Consequently, a strong epithelial remodeling reaction is triggered which compensates for the underlying stromal irregularity. Thus, the corneal midperiphery is initially thicker than the center of the cornea. At the first postoperative month the mean change in superior and inferior mid-peripheral epithelium thickness was +3.42 μm and +2.40 μm, respectively, while the central one was only +0.32 μm (Table 2 and Figure 4). These findings are in accordance with the post-PRK HR AS-OCT studies by Chen et al. and Hou et al., who also used an aspheric aberration-free profile [12,13]. In contrast, Reinstein et al. reported greater epithelial thickening at the cornea center along with gradual peripheral thinning after LASIK done with a standard ablation profile [19].
This difference in corneal epithelial thickness between the central and mid-peripheral areas seems to subside over time. By 3 months postoperatively, the central epithelium was significantly thicker than at the first postoperative month (p=0.001), thus resulting in an epithelium distribution pattern similar to the preoperative one (Table 2 and Figure 4). A similar pattern of epithelial remodeling at the early postoperative period was also observed after myopic LASIK, [10,11,20,23] alcohol-assisted [12] and trans epithelial PRK [13] using HR AS-OCT [10-13] or confocal microscopy [20,23]. Of note, LASIK refractive surgery does not involve debridement of the epithelium, but rather creation of a flap over which the epithelium remains intact. This suggests that the significant postmyopic PRK central epithelial hyperplasia detected in this study and others [12,13] at 3 months postoperatively is not a reaction of the epithelium to debridement, but rather a compensatory change to the underlying ablation-induced stromal asymmetry. Between 3 and 6 months postoperatively we did not observe any statistically significant difference in the corneal epithelial thickness maps (Table 2 and Figure 4). This result is similar with the alcohol-assisted PRK study by Chen et al.[12] and the post- LASIK study by Rocha et al. [10], who reported corneal epithelial and flap thickness stabilization after the third postoperative month. A series of complex neurotrophic changes induced in the cornea by the implementation of excimer laser may explain the stabilization of the epithelial thickness profile after the third postoperative month. The corneal epithelium is innervated by a compact sub-basal plexus of nerve fibers originating from the ophthalmic division of the trigeminal nerve [24]. Excimer laser ablation causes the transection of these subepithelial sensory nerves, resulting in reduced corneal sensation, under-secretion of trophic modulators, [25,26] and, in turn, reduced production of type VII collagen, which is thought to be necessary for the stabilization of the corneal epithelium over the underlying stroma [27]. Confocal microscopy studies have shown that corneal nerve fiber regeneration after excimer laser ablation becomes first noticeable at the third postoperative month [28] and is completed by 6 to 8 months postoperatively [29]. In addition, a positive correlation has been observed between the timing of post-PRK corneal epithelial thickening and subepithelial nerve plexus regeneration[30]. Thus, proper stromal and epithelial healing occurs alongside corneal nerve regeneration, which explains the stabilization of the corneal epithelium thickness profile between 3 and 6 months postoperatively reported in our study.
We observed a positive correlation between the magnitude of the preoperative myopia and the postoperative central epithelial thickening. Every additional diopter of myopic correction resulted in a compensatory central epithelial thickness increase of 1.004 μm (Figure 6). Similarly, Chen et al.12, using HR ASOCT after alcohol-assisted PRK, reported a 1.15 μm epithelium thickening for every additional diopter treated, and Hou et al. [13] noted postoperative central epithelial thickening that was dependent on the amount of the preoperative myopia treated. Comparable results were reported in previous studies using HR AS-OCT after myopic LASIK refractive surgery [9-11].
The gradual central epithelial thickening observed between the first and the third postoperative months explains the mild myopic regression seen during the same time period in our study. Mean manifest refraction spherical equivalent became less hyperopic at the third postoperative month, thus showing a myopic shift, which stabilized by the sixth postoperative month (Table 1 and Figure 2). Additionally, mean K became steeper at 3 months without any further change between 3 and 6 months postoperatively (Table 1 and Figure 3). The initial hyperopic shift at the first postoperative month may also be explained by the aspheric ablation profile of the Schwind Amaris excimer laser. The initial mid-peripheral epithelial hyperplasia, which was induced by the greater stromal tissue removal in the periphery than in the center of the treatment area, had an impact on the corneal contour, thus resulting in the initial overcorrection. Between the first and third postoperative months, the statistically significant epithelial thickening at the center of the ablation area explains the reduction of the initial hyperopic shift and the detected corneal steepening.
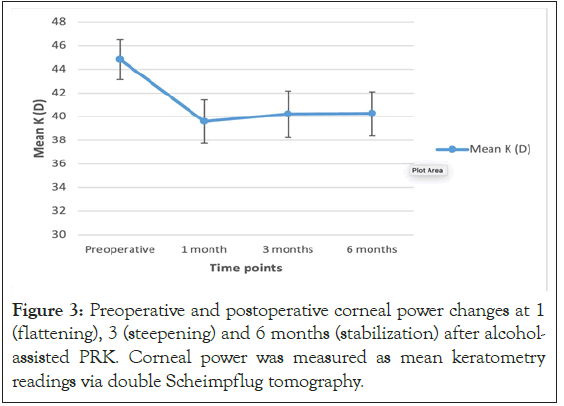
Figure 3: Preoperative and postoperative corneal power changes at 1
The UHR AS-OCT pachymetry mapping in our study did not reveal any statistically significant differences in central corneal thickness (CCT) at 1, 3 and 6 months after PRK (Table 2 and Figure 5). Thus, any postoperative changes in manifest refraction and mean K were only due to epithelial hyperplasia and not due to the thickening of the underlying corneal tissue. This is in agreement with the alcohol-assisted PRK HR AS-OCT study by Chen et al., [12] where no CCT changes were detected up to 6 months postoperatively, and the study by Erie et al., [24] which also recorded no significant post-PRK changes in stromal thickness between the first and the 36th postoperative month.
A negative correlation was observed between the optical zone diameter and the mean central epithelial thickness at 3 months after PRK. In accordance with prior myopic PRK and LASIK studies, [12,13,31] the smaller the optical zone diameter, the greater the observed epithelial thickening. Moreover, greater myopic regression and refractive instability have been previously associated with a treatment diameter smaller than 6 mm [31]. Given that epithelial hyperplasia is associated with myopic regression at the third postoperative month, the use of a smaller optical zone diameter may lead to an even greater myopic shift. Furthermore, since the magnitude of epithelial hyperplasia is positively correlated with the magnitude of the preoperative myopic refractive error, the use of a larger optical zone diameter is crucial when treating moderate and high myopic refractive errors.
The mean overcorrection of 0.27 D at 1 month after PRK was reduced to 0.14 D by 6 months postoperatively, resulting in a total regression value of 0.13 D due to epithelial hyperplasia (Table 1). This myopic shift was induced by 3.13 μm of central epithelial thickening, which implies that 1 D of regression corresponds to epithelial hyperplasia of approximately 24 μm. This mild hyperplasia-induced regression did not result in a residual myopic refractive error (undercorrection). On the contrary, combined with the overcorrection detected at the first postoperative month, it resulted in a more emmetropic final refractive outcome, closer to the initial surgical aim.
Regression due to epithelial hyperplasia differs from regression due to stromal remodelling and collagen regeneration or the effect of factors such as the use of mitomycin-C on the corneal healing process [32,33]. It results from compensatory epithelial thickening due to the flattening of the corneal profile after myopic ablation and is of significant clinical importance. For example, any surgical enhancement should preferably be performed after the third postoperative month, in order for the epithelial hyperplasia-induced regression to be detected and measured. In case of under correction, the hyperplasia-related myopic shift value would have to be added to the remaining refractive error. Additionally when planning myopic PRK surgery for moderate and high myopia a mild initial overcorrection is preferable as it will be reduced by the epithelial hyperplasia-generated myopic regression, thus ultimately resulting in a refractive outcome closest to emmetropia.
A limitation of this study is the inability of the UHR AS-OCT to separate the thickness of the tear film from the epithelial thickness values. Thus, tear film thickness deviations, which may occur in the early postoperative period due to corneal denervation and altered lacrimal gland function, could not be evaluated in this study [34,35].
In summary, the present study demonstrated strong ablationinduced compensatory epithelial thickening at 3 months postmyopic PRK with further stabilization by the sixth postoperative month. The magnitude of the myopia treated and the optical zone diameter appear to contribute to the postoperative epithelial thickness profile. The epithelial hyperplasia-induced regression reduced the hyperopia caused by the aspheric aberration module of the excimer laser in the early postoperative period, leading to a final refractive outcome closer to the initial surgical plan. In future studies, a mathematical model that incorporates variables such as the preoperative refractive error and the optical zone diameter along with UHR AS-OCT-derived epithelial profiles can be developed in order to predict the expected epithelial hyperplasia-generated regression for each patient.
• Excimer laser myopic ablations cause changes in the postoperative epithelial thickness profile.
• Postoperative epithelial thickness deviations have been reported both centrally and mid-peripherally.
• Regression due to postoperative epithelial thickening differs from regression due to stromal remodeling and collagen regeneration.
• Postoperative compensatory epithelial hyperplasia was detected at 3 months and stabilized onwards, as seen using UHR AS-OCT.
• Post-PRK epithelial hyperplasia is not related to epithelial debridement, but rather to a strong response to laser-induced corneal flattening.
• Postoperative epithelial thickening is proportional to the treated myopic error and inversely proportional to the optical zone diameter.
• Post-PRK refractive and mean K deviations are due to epithelial hyperplasia and not due to the underlying stromal thickening.
• Epithelial hyperplasia-induced regression reduces the initial overcorrection seen in the early postoperative period, thus leading to an emmetropic refractive outcome.
Citation: Bachtalia K, Plakitsi A, Charonis A, Charonis G, Kyroudis D, Palioura S (2021) Compensatory Corneal Epithelial Thickness Changes after Myopic Photorefractive Keratectomy Imaged with Ultra High Resolution Anterior Segment Optical Coherence Tomography. J Clin Exp Ophthalmol. S12:002.
Received: 11-Jan-2021 Accepted: 25-Jan-2021 Published: 01-Feb-2021 , DOI: 10.35248/2155-9570.21.s12.002
Copyright: © 2021 Bachtalia K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.