Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2020)Volume 11, Issue 1
Introduction: Cataract extraction constitutes the largest workload through DBCS program in ophthalmic units in India. Both SICS & Phacoemulsification surgery are performed in a limited, confined space; however, securing adequate surgical space during cataract surgery can decrease the risk of corneal endothelial cell loss.1 Thus, anatomical and surgical factors, such as adequate Anterior Chamber Depth (ACD), are important for preserving these cells from the mechanical and thermal damage that can occur during the procedure. Under normal circumstances, corneal endothelial cells do not proliferate because they are stuck in G1 phase of cell cycle. The central corneal endothelial cell density gradually decreases at an average of about 0.6% per year, reducing approximately from 3400 cells/mm2 at age 15 to 2300 cells at age 80 years. Two important factors in maintaining corneal transparency are the number and the integrity of the corneal endothelial cells.3 Corneas with cell densities as low as 500 cells/mm2 and average cell area of approximately 2000-3000 μm2 can remain clear. Protection of corneal endothelium during cataract surgery is critical for achieving good visual outcomes.
Objectives: To study the endothelial cell loss in SICS and Phacoemulsification and compare the cell loss between two surgeries and to compare morphological and functional changes in corneal endothelium between the two surgeries.
Materials and methods: A comparative prospective study is performed in 200 eyes of 200 patients attending DBCS Camp at Babuji Eye Hospital and Chigateri General Hospital attached to JJM Medical College Hospital, Davanagere from July 2018 to October 2019 for cataract surgery. Patients were randomly allocated to two groups. One group underwent small incision cataract surgery and the other group underwent phacoemulsification. Corneal endothelial assessment was done for patients undergoing both the surgeries using non-contact specular microscopy Tomey EM 3000 preoperatively and postoperatively at 1 week and 6 weeks.
Results: In SICS group, corneal endothelial count was 2303.0 ± 329.1 preoperatively, postoperatively it was reduced to 2068.9 ± 381.1 at 1 week and 1980.3 ± 401.5 at 6 weeks. In phacoemulsification group, it was found to be 2213.9 ± 442.3 preoperatively and which reduced to 1878.7 ± 458.3 at 1 week and 1796.4 ± 467.3 at 6 weeks postoperatively. Cases in SICS group showed 10.2% loss at 1 week and 14% cell loss at 6 weeks while phacoemulsification group showed 15.1% cell loss at 1 week and 18.9% cell loss at 6 weeks. Polymegathism was increased in both the groups while hexagonality was decreased in both groups. No significant difference in functional parameters like central corneal thickness (CCT) and best corrected visual acuity (BCVA) was observed in both SICS and Phacoemulsification group at the end of 6 weeks.
Conclusion: The study shows that phacoemulsification is safe procedure in experienced hands. Compared to phacoemulsification, small incision cataract surgery is associated with lower post-operative endothelial damage. It is suggested that SICS should be used in patients at risk for endothelial damage in cataract surgery.
Bilateral blindness; Cataract surgery; Ageing process
Cataract is defined as any congenital or acquired opacity in the lens capsule or substance, irrespective of vision [1].
About 20 million people are aected worldwide with cataracts which seem to be a leading cause of visual deterioration progressing to bilateral blindness. 50%-90% of all the blindness in developing countries is caused by cataract [2]. Cataract is responsible for 62.4% of blindness in India and the prevalence of blindness is 5.3% [3].
Most common cause of cataract is the normal ageing process; other causes include injury, chronic eye disease and other systemic diseases such as diabetes mellitus [2]. The only eective treatment of cataract is to remove the opacified lens surgically. No diet or medication can stop cataract formation. Cataract surgery aims to improve vision and thereby the quality of life of aected people [4].
The largest workload in ophthalmic units throughout the world is constituted by cataract surgery [5].
Protection of the corneal endothelium is critical for achieving good visual outcomes [6]. Two important factors for corneal transparency are the number and the integrity of corneal endothelial cells [7].
Corneal endothelium is single layer of regularly arranged polygonal cells covering the entire cornea which is important factor for maintaining the corneal hydration. At least 400-700 cells/mm2 are required to maintain a normal endothelial function. If the count falls below 500 cells/mm2, it results in corneal oedema and decompensation [8]. Under normal circumstances, corneal endothelium cells do not proliferate because they are stuck in the G1 phase of cell cycle. Throughout life the central corneal endothelial cell density gradually reduces at an average rate of about 0.6% per year, approximately varies from 3400 cells/mm2 to 2300 cells/mm2 from age 15 to 85 respectively [9].
Reduction in corneal endothelial cell density may result from number of factors such as cataract extraction, ageing process, glaucoma, intraocular inflammation, blunt ocular trauma, corneal endotheliopathies like fuch’s endothelial dystrophy [8]. Hence, preoperative assessment of corneal endothelium as well as ruling out the existence of such conditions is important for the surgery to be successful.
Cataract extraction has been reported by several studies to be one of the factors contributing to the reduction of the corneal endothelia density. Endothelial cell injury during cataract surgery occurs due to a number of reasons, such as corneal distortion, ricocheting of nuclear fragments, intraocular lens contact and release of free radicals [10]. Likewise in phacoemulsification, the ultrasound power fluctuations, bouncing fragments, the fluid turbulence and the increased production of the free radicals cause great stress on endothelium [9].
The free radicals are produce due to the ultrasound energy and the ophthalmic viscoelastic devices. Ultrasound in aqueous induces cavitation, directly causing water molecule disintegration and resulting in formation of hydroxyl radicals, the most potent of reactive oxygen species [11].
After the loss of endothelial cells, adjacent cells enlarge and slide over to maintain the endothelial cell continuity, which can be seen as a change in endothelial cell density and morphology. A transient increase in corneal thickness is seen after moderate damage to the endothelium during the surgery. Endothelial cell density and the function can be assessed clinically using specular microscopy was shown in Figure 1 [12].
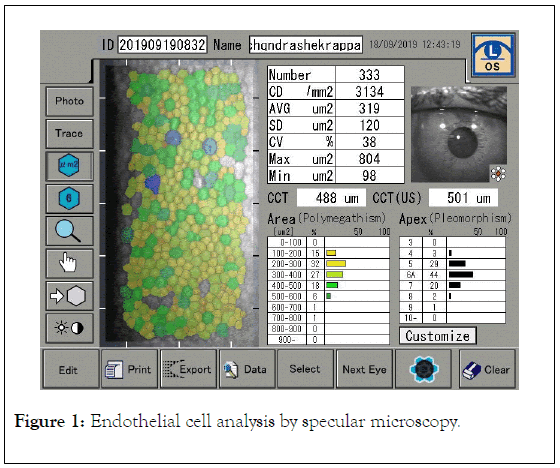
Figure 1. Endothelial cell analysis by specular microscopy.
Corneal endothelial cell layer can be viewed and recorded noninvasively by using specular microscopy. The clinical specular microscopes are all based on the laboratory microscope design by Maurice to provide a high magnification view of specular reflected light from the Corneal endothelium. The specular reflex occurs at a regular, smooth surfaced interface of two refractive indices with light from the subject having an angle of incidence equal to the angle of reflection to the observer. The endothelial cells can be imaged because the refractive index of the endothelial cells is greater than the 1.336 value of the aqueous humor, thus reflecting 0.022% of the projected light [13].
The response and eect of stress and trauma of cataract surgery on endothelial cells could not have been so well documented without the advent of specular microscopy [13].
Study design and study area
Study group included 200 patients aged above 40 years and both gender operated under DBCS camp at Babuji Hospital and Chigateri General Hospital attached to JJM Medical College Hospital, Davanagere from July 2018 to October 2019 for cataract surgery.
Prospective Comparative study
We analysed 200 patients (100 eyes for small incision cataract surgery and 100 eyes for phacoemulsification)
Inclusion criteria
• All patients operated for cataract surgery under DBCS camp at Babuji Hospital and Chigateri General Hospital attached to JJM Medical College Hospital, Davanagere from July 2018 to October 2019.
• Patients operated by uneventful manual SICS and Phacoemulsification.
• Preoperative Cataract grading by Lens Opacities Classification System III (LOCS
• III) Classification was done, which includes nuclear sclerosis grades 1-4, all cortical cataract grades and all posterior subcapsular grades (Figure 2).
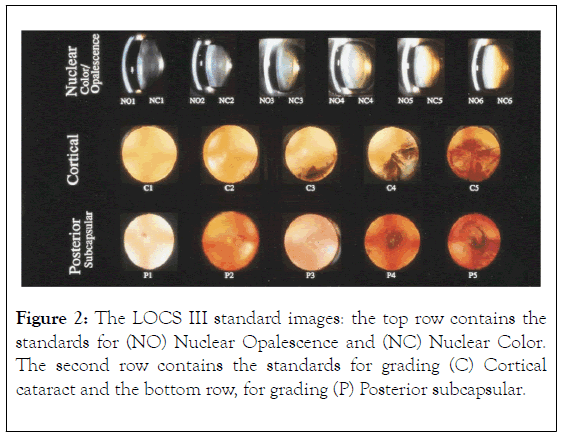
Figure 2. The LOCS III standard images: the top row contains the standards for (NO) Nuclear Opalescence and (NC) Nuclear Color. The second row contains the standards for grading (C) Cortical cataract and the bottom row, for grading (P) Posterior subcapsular.
Exclusion criteria
• Congenital Cataract and Development cataract
• Traumatic Cataract
• Complicated cataract
• Corneal endothelial dystrophies or any other corneal diseases aecting endothelial cell function, corneal opacity
• Uveitis
• Glaucoma
• Pseudoexfoliation syndrome
• Patients with previous intraocular surgery
• Poorly controlled or uncontrolled type II Diabetes Mellitus i.e HBA1c>7%
• Nuclear sclerosis grading 5,6 by LOCS III classification
• Preoperative endothelial cell count of <1500 cells/mm
• Small pupil diameter less than 4 mm after a full dilatation
• Patients with intra operative complications like PC rent, dislocated IOL and iridodialysis.
Methods of collection of data
• Patients operated under DBCS programme in department of ophthalmology from July 2018 to October 2019.
• Informed consent taken in accordance with Helsinki Declaration
• A detailed history including demographics, ocular disease, past history and surgical history, drug history and personal history was taken.
Ophthalmological examination included
• Each eye was examined individually
• Visual acuity (best corrected) using Snellen’s chart
• Near vision with Times New Roman chart
• Slit lamp examination
• Intraocular pressure using Goldman ’ s Applanation Tonometry
• Funds examination using direct ophthalmoscope and indirect ophthalmoscope
• Corneal endothelial cell count assessed by non contact specular microscopy Tomey EM 3000 preoperatively and post operatively at one week and six weeks.
In the study the patients were divided into two groups
Group A: Patients with cataract undergoing small incision cataract surgery-100 eyes of 100 patients.
Group B: Patients with cataract undergoing phacoemulsification-100 eyes of 100 patients.
Operative procedure
The pupil was dilated using tropicamide 0.8% with phenylephrine hydrochloride 5% solution, cyclopentolate 1% and flurbiprofen 0.03% eye drops one hour prior to surgery for every 15 minutes.
Anaesthesia: Peribulbar Anaesthesia
5 ml mixture of lignocaine solution 2% (with adrenaline 1 in 100000 and without adrenaline for hypertensive and diabetic individuals) with hyaluronidase 5 IU/ml with Bupivacaine solution 0.5% is used.
Surgical technique
Procedure for SICS: A fornix based conjunctival flap was made at the superior limbus, and bleeding was cauterised. A 6.0 mm incision was made on the sclera 1.5 mm from the superior limbus. A tunnel was created with stainless-steel crescent knife. A side port was made at 3 o’clock or 9 o’clock. Hydroxypropyl methylcellulose (HPMC) 2% was injected to fill the anterior chamber. A 26 gauge bent capsulotomy needle was used to create a continuous curvilinear capsulorrhexis (CCC). An entry was made through the tunnel using 3.2 mm keratome. The tunnel was then extended using an extension blade.
Hydrodissection was performed using balanced salt solution. The anterior chamber was refilled with viscoelastic (HPMC 2%) and the nucleus rotated and tumbled into anterior chamber with dialler. The viscoelastic was again injected below to maintain the anterior chamber as well as above nucleus to protect endothelium. The nucleus was then delivered using visco-expression. The remaining cortical matter was removed with simcoe’s irrigation and aspiration cannula. After which a polymethylmethacrylate posterior chamber IOL was implanted in the capsular bag. Side port wound was closed by hydrating the stroma. A subconjunctival injection (0.3 ml) of 10 mg gentamicin and 2 mg dexamethasone was given. A drop of topical antibiotic steroid solution was administered and eye was patched. The procedure was carried out with meticulous aseptic precautions.
Procedure for Phacoemulsification: A superior clear corneal incision of 2.8 mm and two side port entries are made at 3 o’ clock and 9 o ’ clock followed by injection of viscoelastic substance (2% hydroxypropylmethylcellulose) to maintain the anterior chamber. Continuous curvilinear capsulorrhexis (CCC) of 5-6 mm was done by 26 gauge bent capsulotomy needle. Hydrodissection and hydrodelineation were performed using balanced salt solution. The viscoelastic was then injected and the nucleus stabilised with chopper. A divide and conquer technique was done using phacoemulsification inside the capsular bag. Cortex was removed by I/suction. Balanced salt solution was used for irrigation. A foldable acrylic IOL was then implanted into capsular bag. Wound was closed by hydrating the stroma. A subconjunctival injection (0.3 ml) of 10 mg gentamicin and 2 mg dexamethasone was given. A drop of topical antibiotic steroid solution was administered and eye was patched. The procedure was carried out with meticulous aseptic precautions.
Post-operative care
The post-operative care was given with course of topical antibiotics, topical steroid in tapering doses for 6 weeks to all the patients.
All patients were followed after 1st week and 6th week. At each visit preliminary examination like visual acuity, slit lamp examination, intraocular pressure and specular microscopy was done.
Statistics
Statistical analysis was done using SPSS (version 17) software.
Results are presented as mean, standard deviation and range values for continuous data, number and percentages for categorical data. Intergroup comparisons are done by unpaired t test and intra group comparisons by paired t test. Chi square test of association was used to analyse categorical data. p value of 0.05 or less was considered for statistically significance.
Age group
In Group A, 56 patients (56%) were in the age group 61-70 years. In group B, 44 patients (44%) were in the age group of 51-60 years. There is statistically significant dierence in age and p value <0.05 was shown in Table 1 and Figure 3.
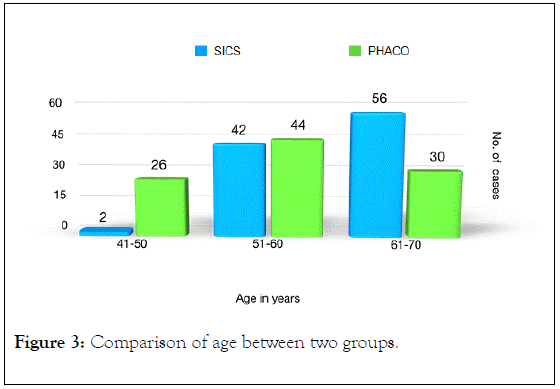
Figure 3. Comparison of age between two groups.
| Age Groups | Group A (SICS) | Group B (PHACO) |
|---|---|---|
| Number (percentage) | Number (percentage) | |
| 41-50 | 2 | 26 |
| 51-60 | 42 | 44 |
| 61-70 | 56 | 30 |
| Total | 100 | 100 |
Table 1: Comparison of age between two groups.
Sex distribution
The data signifies that the incidence of cataract is higher among women. It may also signify lower cataract surgical coverage for women in previous DBCS camps was shown in Table 2 and Figure 4.
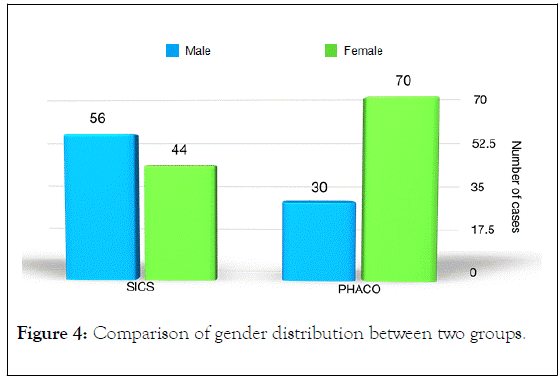
Figure 4. Comparison of gender distribution between two groups.
| Characteristics | Group A (SICS) | Group B (PHACO) | Unpaired t Test | p value | |
|---|---|---|---|---|---|
| Age | Mean SD | 62.3 ± 6.2 | 56.9 ± 7.2 | 4.07 | <0.05, S |
| Range | 49-70 | 43-70 | |||
| Sex | Male | 56 | 30 | X2=6.89 | <0.05, S |
| Female | 44 | 70 | |||
| EYE | LE | 52 | 50 | X2=0.04 | p=0.95, NS |
| RE | 48 | 50 | |||
Table 2: Descriptive information between two groups (unpaired t test, p<0.05, significant. p>0.05, Not significant).
Best corrected visual acuity
BCVA was measured in terms of LogMAR. In Group A, the mean BCVA preoperatively was 1.25, post operatively improved to 0.50 and 0.28 at 1 week and 6 weeks respectively. In Group B, the mean BCVA preoperatively was 1.09, post operatively improved to 0.52 and 0.26 at 1 week and 6 weeks respectively.
No statistically significant dierence was found in BCVA between two groups at the end of 1 week and 6 week post operatively, suggesting best corrected vision was comparable in both SICS and PHACO was shown in Table 3.
| Group A | Group B | Group A v/s B | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Unpaired t Test | p value | |
| Pre-op | 1.25 | 0.24 | 0.09 | 3.04 | 0.003 | S |
| Week 1 | 0.5 | 0.18 | 0.52 | 0.31 | 0.76 | NS |
| Week 6 | 0.28 | 0.15 | 0.26 | 0.46 | 0.65 | NS |
Table 3: Comparison of BCVA preoperatively and postoperatively between two groups (unpaired t test, p<0.005, significant. p>0.005, Not significant)
Endothelial cell count preoperatively and postoperatively
In Group A, mean endothelial cell count preoperatively was 2303.0 cells/mm2 and was 2068.9 cells/mm2 and 1980.3 cells/mm2 post operatively at the end of 1 week and 6 weeks respectively. In Group B, mean endothelial cell count preoperatively was 2213.9 cells/mm2 and post operatively was 1878.7 cells/mm2 at 1 week and 1796.4 cells/mm2 at 6 weeks was shown in Table 4.
| Group A | Group B | Group A v/s B | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | p | |
| Pre-op | 2303 | 329.1 | 2213.9 | 442.3 | 1.14 | 0.26, NS |
| Week 1 | 2068.9 | 381.1 | 1878.7 | 458.3 | 2.26 | 0.03, S |
| Week 6 | 1980.3 | 401.5 | 1796.4 | 467.3 | 2.11 | 0.04, S |
Table 4: Comparison of Endothelial Cell Count preoperatively and postoperatively between two groups (unpaired t test, p<0.05, significant., p>0.05, Not significant).
Statistical significant dierence in endothelial cell count was seen between two groups at the end of 1 week and 6 weeks post operatively.
Endothelial cell loss preoperatively and postoperatively
In Group A (SICS), mean endothelial cell loss at the end of 1 week was 234.1 cells/ mm2 (10.2%) and 332.7 cells/mm2 (14%) at the end of 6 weeks. In Group B (PHACO), mean endothelial cell loss at the end of 1 week was 335.2 cells/mm2 (15.1%) and 417.5 cells/mm2 (18.9%) at the end of 6 weeks.
Highly statistical significant dierence in the mean endothelial cell loss was observed between both the groups at the end of 1 week and 6 weeks was shown in Table 5 and Figure 5.
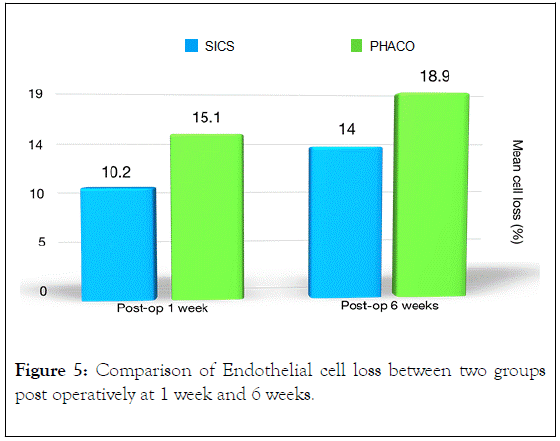
Figure 5. Comparison of Endothelial cell loss between two groups post operatively at 1 week and 6 weeks.
| Groups | Mean CD (cells/mm2) | Mean cell loss | SICS v/s PHACO | ||||
|---|---|---|---|---|---|---|---|
| Preop | 1 week | 6 weeks | 1 week | 6 week | At 1 week | At 6 week | |
| SICS | 2303.0 ± 329.1 | 2068.9 ± 381.1 | 1980.3 ± 401.5 | 234.1 | 332.7 | t=6.85, | t=5.21, |
| 10.20% | 14.00% | p<0.001, HS | p<0.001, HS | ||||
| PHACO | 2213.9 ± 442.3 | 1878.7 ± 458.3 | 1796.4 ± 467.3 | 335.2 | 417.5 | ||
| 15.10% | 18.90% | ||||||
Table 5: Comparison of Endothelial Cell loss postoperatively at 1 week and 6 weeks between two groups (unpaired t test, p<0.005, significant, p>0.005, Not significant).
Co-efficient of variation
Polymegathism as measured by Coecient of Variation (CV) increased in both the groups postoperatively. In group A, mean CV increased from 41.1% to 45.5% at the end of 6 weeks. Similarly in group B, mean CV increased from 41.7% to 46.4% at the end of 6 weeks.
In neither of the groups there was observed no statistical significance either at the end of 1 week or 6 weeks was shown in Table 6.
| Group A | Group B | Group A v/s B | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | p | |
| Pre-op | 41.1 | 9 | 41.7 | 8.9 | 0.35 | 0.76, NS |
| Week 1 | 44.8 | 8.5 | 46.4 | 10.6 | 0.85 | 0.40, NS |
| Week 6 | 45.5 | 8.3 | 46.4 | 12.6 | 0.42 | 0.67, NS |
Table 6: Comparison of CV (co-efficient of variation) preoperatively and postoperatively between two groups (unpaired t test, p>0.05, Not significant)
Hexagonality
In group A, mean preoperative mean % of hexagonality (pleomorphism) was observed to be 42.68% which reduced to 39.74% at the end of 1 week and 37.54% at the end of 6 weeks.
In group B, mean preoperative mean % of hexagonality (pleomorphism) was observed to be 41.26% which reduced to 37.66% at the end of 1 week and 36.26% at the end of 6 weeks. Suggesting no statistical significance in both groups was shown in Table 7.
| Group A | Group B | Group A v/s B | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | p | |
| Pre-op | 42.68 | 5.32 | 41.26 | 7.9 | 1.06 | 0.29, NS |
| Week 1 | 39.74 | 5.79 | 37.66 | 1.26 | 1.26 | 0.21, NS |
| Week 6 | 37.54 | 6.41 | 36.26 | 0.74 | 0.74 | 0.46, NS |
Table 7: Comparison of Hexagonality (6A) preoperatively and postoperatively between two groups (unpaired t test, p<0.05, significant, p>0.05, Not significant).
In both the groups the following parameters like BCVA, intraocular pressure, CDMM, co-ecient of variability, hexagonality and central corneal thickness showed high significance at the end of 6 weeks when compared to preoperative mean values was shown in Table 8.
| Variable | Groups | Pre-op | At 6 weeks | Mean diff | t value | p value |
|---|---|---|---|---|---|---|
| BCVA | SICS | 1.25 ± 0.24 | 0.28 ± 0.15 | 0.97 ± 0.30 | 22.76 | ** HS |
| PHACO | 1.09 ± 0.29 | 0.26 ± 0.25 | 0.82 ± 0.21 | 27.86 | ** HS | |
| IOP | SICS | 17.44 ± 1.94 | 18.46 ± 1.91 | 1.02 ± 0.14 | 51 | ** HS |
| PHACO | 17.50 ± 1.54 | 19.26 ± 1.31 | 1.76 ± 0.43 | 28.85 | ** HS | |
| CD/mm2 | SICS | 2303.0 ± 329.1 | 1980.3 ± 401.5 | 322.7 ± 118.3 | 19.28 | ** HS |
| PHACO | 2213.9 ± 442.3 | 1796.4 ± 467.3 | 417.5 ± 50.4 | 58.57 | ** HS | |
| CV% | SICS | 41.08 ± 8.96 | 45.46 ± 8.31 | 4.38 ± 4.15 | 7.46 | ** HS |
| PHACO | 41.70 ± 8.87 | 46.36 ± 12.61 | 4.66 ± 5.48 | 6.02 | ** HS | |
| 6A | SICS | 42.68 ± 5.32 | 37.54 ± 6.41 | 5.14 ± 3.33 | 10.93 | ** HS |
| PHACO | 41.26 ± 7.9 | 36.26 ± 10.49 | 5.00 ± 5.05 | 6.99 | ** HS | |
| CCT | SICS | 512.52 ± 32.41 | 532.20 ± 31.22 | 19.78 ± 5.66 | 24.72 | ** HS |
| PHACO | 511.92 ± 35.72 | 531.96 ± 38.02 | 20.04 ± 10.23 | 13.85 | ** HS |
Table 8: Comparison of changes in various parameters preoperatively and postoperatively at 6 weeks between two groups (paired t test, p<0.001, highly significant).
This study titled “Comparison of morphological and functional corneal endothelial changes after cataract surgery under DBCS program at a tertiary care centre” was conducted in Department of ophthalmology, JJM Medical College, Davanagere using specular microscopy as the imaging modality, corneal endothelial cell analysis was done in 200 eyes of 200 patients.
Corneal endothelial cells can be damaged by many factors during and after cataract surgery. Intra-operative factors associated with corneal endothelial injury include bubble and free radical formation during phacoemulsification, ultrasound energy, and mechanical trauma by instruments, and presence of lens fragments.
An ideal procedure is one that protects the Intraocular tissue from surgical damage particularly the corneal endothelium, as the count usually decreases with age.1 Study of Endothelial alterations are important parameters to access surgical trauma and to study ecacy of dierent surgical techniques [1].
Our study showed most of the patients to be above the age of 60 years, which is similar to other studies which found high prevalence of cataract as the age progresses. Our study included a total of 86 males and 114 females showing higher rates of cataract in women. Another study by Vashist et al. also observed higher rates of cataract in females [14].
Mean endothelial cell loss
It was found in our study that in case of SICS 10.2% cell loss at 1 week and 14.0 % cell loss at 6 weeks. The phacoemulsification group showed 15.1% cell loss at 1 week and 18.9% cell loss at 6 weeks.
endothelial cell loss of 331.9 cells/mm2 (11.1%) at week and 456.1 cells/mm2 (15.3%) at 6 weeks compared to the phacoemulsification group where the endothelial cell loss was 404.1 cells/mm2 (13.2%) at 1 week and 474.2 cells/mm2 (15.5%) at 6 weeks.7 Our study showed similar percentage of endothelial cell loss in both SICS and PHACO group preoperatively, post operatively at 1 week and 6 weeks.
Tejinder et al. stated in a study the mean endothelial cell loss in SICS was 274.03 cells/mm2 (10.95%) at 1 week and 427.51 cells/mm2 (17.17%) at 6 weeks. In Phaco group the mean loss was 326.81 cells/mm2 (12.96%) at 1 week and 494.04 cells/mm2 (19.53%) at 6 weeks post operatively [15].
Our study showed similar percentage of endothelial cell loss in both SICS and Phaco group.
A study done by Ganekal et al. found in SICS group there was a decrease in cell density of 315.08 cells/mm2 (13.49%) and 76.12 cells/mm2 (3.27%) in phacoemulsification group [12].
The results for SICS are similar to our study but there is gross dierence in ECL in Phacoemulsification.
Co-efficient of variation
Polymegathism as measured by co-ecient of variation was increased in both the groups. Preoperatively CV was 41.08 ± 8.96% SICS group and in 41.70 ± 8.87% in phacoemulsification group. Here we found that at one week postoperative mean CV was increased significantly in both groups.
However the change was not significant when compared at the end of 6 weeks.
Hexagonality
In our study, mean % of hexagonality was seen around 42.68 ± 5.32 in SICS group and around 41.26 ± 7.90 in phacoemulsification group respectively. Post operatively it was observed to decrease in both the groups.
The loss of hexagonal cells over the time after surgery was not clinically significant. Percentage of hexagonality and co-ecient of variation considered as indices of repair mechanism. When the endothelium is stabilised after a period of rearrangement, the CV and 6A shifts toward the preoperative status.
Best corrected visual acuity
In our study, no significant dierence was found in between both SICS group and Phaco group at the end of 6 weeks. A study done by Gogate et al. found that in corrected distance visual acuity at 6 weeks showed no significant statistical dierence between SICS and Phacoemulsification which was similar to our study [7].
Several other studies like Kaur et al., Jagani et al. also shows the same inference [15,16].
Central corneal thickness
Central corneal thickness was increased in both the groups. Preoperatively CV was 512.52 ± 32.41 SICS group and in 511.92 ± 35.72 in phacoemulsification group. Here we found that at one week postoperative mean CCT was increased significantly in both groups. However the change was not significant when compared at the end of 6 weeks.
One of the limitation of our study was that only one technique of phacoemulsification and one technique of SICS was compared; other techniques may give variable results.
The dierence was more likely a result of the divide and conquer technique used for phacoemulsification and the sandwich technique using vectis and dialler used for nucleus delivery in SICS. A study done by Storr-Paulse et al. compared endothelial cell damage during cataract surgery performed using divide and conquer or phaco-chop nuclear fracturing technique suggested that phaco-chop technique is less harmful to the endothelium as it uses less power [17].
The higher cell loss in our study is probably because cases of harder cataracts were not completely excluded. The lower loss of endothelial cells in complicated cases in the SICS group may have been due to easier maneurverability, especially of hard cataracts, through the large incision used in the technique.
According to study done by Mehra et al. endothelial cell loss is also depending on grading of nuclear sclerosis at the time of surgery [18].
A study done by Ravalico et al. showed no significant decrease in mean endothelial cell density with the use of four viscoelastic (HPMC, Healon, Healon GV and Viscoat) [19]. Hence we opted for HPMC in both group cases.
A study by Beltrame et al., compared endothelial cell damage between scleral tunnel incisions and clear corneal tunnel [20]. Supporting our study concluded that scleral tunnels led to less postoperative endothelial cell damage than clear corneal tunnels. Because SICS was performed through the scleral tunnel incision, it may have caused less endothelial cell loss than phacoemulsification performed through a clear corneal tunnel incision.
Another major weakness of our study was short term follow up (6 weeks) however prospective study from United States evaluating the long term safety (5 years) of phakic found that the rate of endothelial cell loss decreases over time. This agrees with short term studies, which reports a higher rate of endothelial cell loss than the longer studies [21-23].
Endothelial cell loss is more likely related to corneal endothelial cell remodelling after the trauma of surgery than to on-going age related cell loss. A study comparing the eect of dierent phacoemulsification techniques on corneal endothelial cells found similar outcomes at 3 months and 1 year, postoperatively. Based on these outcomes, we believe the short term follow-up is adequate to predict the long term outcomes. Additionally, by using 6 weeks follow up cuto helped us reduce the number of patients lost to follow up, which increase the validity of the present study [12].
The decrease in ECD of healthy corneas with increasing age varies from 0.2% to 2.8% per year, whereas ECL after ultrasound phacoemulsification varies from 3.2% to 23.2%.
However with the introduction of new phacoemulsification systems, cataract surgery has become a safe procedure [12]. New machines combine fewer surges, lower amounts of ultrasound, and more controlled anterior-chamber depth, as wells lower incidence of thermal burns at the incision site [24-26].
More recent cataract surgical technologies have been developed without ultrasound. These systems include laser, sonic energy, and the new water jet-based technology for removing cataracts through a small self-sealing incision. The non-ultrasound equipments uses high-energy, high-velocity pulses of warmed solution (balanced salt solution at 50-100 Hz) to break up cataracts, which are simultaneously aspirated. The water jet fluid pulse temperature is 125 F, the irrigation fluid is 75 F, and the temperature of the mix of these 2 fluids is 89 F. The impact of the heated fluid rapidly strains the cataract, causing emulsification that works only on the lens and not on the lens capsule, reducing the risk of incisional burns and potentially reducing the risk for posterior capsule rupture.
In our study we used the Infinity Phaco System (Alcon Laboratories) which uses OZiL technology. It utilises torsional phaco ultrasound energy. It reduces the ultrasound energy delivered to corneal endothelium [10].
In the study most of the patient was found to be more than the age of 60 years with the total of 86 males and 114 females showing higher rates of cataract in women.
Cases of SICS group showed 10.2% cell loss at 1 week and 14.0 % cell loss at 6 weeks. The phacoemulsification group showed 15.1% cell loss at 1 week and 18.9% cell loss at 6 weeks.
Polymegathism was increased in both the groups while hexagonality was decreased in both groups. No significant dierence was found in between both SICS group and Phaco group at the end of 6 weeks.
A wide variation in endothelial cell loss between the various studies even when the mode of surgery is same (e.g., SICS) was due to various factors like dierent inclusion and exclusion criteria, dierent grades of cataract, dierent types of nucleus delivery in SICS, dierent types of irrigating solution and viscoelastic. The reported endothelial loss varies between 4% to 25%, and the period of increased postoperative endothelial cell loss remains unknown. Endothelial cell loss begins soon after surgery, continues for at least 10 years postoperatively and may be throughout the patient’s life.
Various modifications of SICS (irrigating vectis, viscoexpression of the nucleus, anterior chamber maintainer, high density viscoelastics) have significantly reduced the endothelial cell loss. In phacoemulsification, the manoeuvring is mechanical and performed in the bag; distantly from the endothelium and newer advanced phacoemulsification units with better fluidics may reduce the chances of endothelial damage.
The study shows that phacoemulsification is safe procedure in experienced hands. Compared with Phacoemulsification, SICS is associated with lower post-operative endothelial damage. It is suggested that SICS should be used in patients at risk for endothelial damage in cataract surgery.
Citation: Gupta M, Manjunath BH, Shedole SS (2020) Comparison of Morphological and Functional Corneal Endothelial Changes after Cataract Surgery under DBCS Program at a Tertiary Care Centre. J Clin Exp Ophthal. 11:823. DOI: 10.35248/2155-9570.20.11.823
Received: 13-Jan-2020 Accepted: 28-Jan-2020 Published: 04-Feb-2020 , DOI: 10.35248/2155-9570.20.11.823
Copyright: ©2020 Gupta M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.