Journal of Bone Research
Open Access
ISSN: 2572-4916
ISSN: 2572-4916
Research Article - (2023)Volume 11, Issue 4
It is difficult to find out primary site of origin in patients of bone metastasis. Skeletal metastasis is a common metastatic site in several cancers. Making a diagnosis of primary site is most crucial step in bone metastasis. Up to 30% of patients present with bone metastases of unknown origin, where the site of the primary neoplasm cannot be identified at the time of diagnosis despite a thorough history, physical examination, appropriate laboratory testing and modern imaging technology (CT, MRI, and PET). Sometimes only extensive histopathological investigations on bone specimens from biopsy can suggest the primary malignancy. This retrospect study analyses primary site in patients with bone metastasis.
Bone metastasis; Diagnosis; Histopathology
BMP: Bone Morphogenetic Proteins; BMA: Bone Modifying Agents; CR: Complete Response; CAPOX: Capecitabine and Oxaliplatin; DFS: Disease Free Survival; ECOG-PS: Eastern Cooperative Oncology Group-Performance Status; EMA: Epithelial Membrane Antigen; ER: Estrogen Receptor; EGFR: Epidermal Growth Factor Receptor; HCG: Human Chorionic Gonadotropin; H&E: Hematoxylin and Eosin; IHC: Immunohistochemistry; LFU: Loss to Follow Up; LFT: Liver Function Test; LDH: Lactate Dehydrogenase; MRI: Magnetic Resonance Imaging; MM: Multiple Myeloma; NSCLC: Non-Small Cell Lung Cancer; NSAIDS: Non-Steroidal Anti-Inflammatory Drugs; OPD: Out Patient Department; PTHrP: Parathyroid Hormone Related Protein Peptide; PSA: Prostate Specific Antigen; PR: Progesterone Receptor; PET-CT: Positron Emission Tomography; PR: Partial Response; PD: Progressive Disease; RANK: Receptor Activator of Nuclear Factor Kappa Ligand; RCC: Renal Cell Carcinoma; RFT: Renal Function Test; RT: Radiotherapy; Ra-223: Radium; Sr 89: Trontion; Sm-153: Samarium; SD: Standard Deviation
Metastatic bone disease forms due to interaction between bone and tumor cells. Bone metastases are highly responsible for the morbidity in cancer patients and third most frequent site of metastasis followed by lung and liver [1]. In recent times, the incidence of bone metastases has increased however, better cancer treatments have improved survival in patients [2]. This has resulted in a radical change in the perception of the clinicians. As per literature reports, up to 30% patients presenting with bone metastasis have unknown origin site of primary cancer [3]. Incidence of bone metastasis is higher in breast and prostate cancer [4]. However, it is difficult to quantify the prevalence of bone metastasis. Median survival rate of patients with bone metastasis is five months after the diagnosis, and survival rates are 5% after five years and 1% after ten years [5].
Patient’s quality of life is affected by presence of bone metastatic disease due to increased pain, impaired mobility, and incidence of fractures, spinal cord compression and decline of performance status [6]. The frequency of other major complications depends on the nature of bone lesions, their site, and their treatment [7].
Lytic lesions mostly present in breast, thyroid, kidney and lung cancer, predispose to severe complications such as pathological fractures and hypercalcemia. Some patients may also present with pathological fractures and their associated complications. One such complication is neurological impairment, which is more common in spine metastasis. The spine is infamously known to be the most common site of skeletal metastasis. The prevalence of osteoblastic lesions, as seen in prostate cancer for example could lead to such complications and bisphosphonates have been used to reduce the frequency of major complications in cancer patients. Use of sensitive diagnostic tools and better treatment measures could thus possibly reduce the severe outcomes associated with bone metastases and improve patient survival.
Nevertheless, effective treatments are available for some tumors, such as hormone-dependent cancers, thyroid cancer, neuroblastoma, germ cell cancers, colon cancer, and, less consistently, cancer of the endometrium, kidney, and ovary. Therefore, every effort should be made to identify the primary. The diagnostic strategy in this situation should focus on treating primary cancer to achieve treatment objectives. Several studies of small cohorts have prompted suggestions for different diagnostic strategies based on the number of bone metastases, their appearance (lytic, sclerotic, or mixed), and the presence of extra skeletal metastases [8]. Histological examination of biopsies from metastatic sites constitutes the cornerstone of these diagnostic strategies. Bone biopsy is a procedure that is part of the armamentarium for identifying an unknown primary.
Proper diagnosis of bone tumors requires careful examination of all available sources of information, including patient history, physical examination, plain films and other imaging techniques, such as Computed Tomography (CT) and Magnetic Resonance Imaging (MRI). Each imaging option has its own strengths, which must be considered during analysis. The most accurate diagnostic tool available to the clinician is bone biopsy which provides histological evidence, with in an accurate diagnosis of the tumor lesion. However, it provides no evidence as to the progression or aggressiveness of the lesion. Biopsy, therefore, is best used in conjunction with plain films to provide the most complete diagnosis. In any case, even when the primary cancer is unknown, the patient should always be referred as soon as possible to an oncologist after the diagnosis of bone metastasis has been confirmed at biopsy.
The delayed diagnosis has negative effects on the prognosis and also enhances the risk of skeletal-related events, including fractures or spinal cord compression. Therefore, accurate diagnosis and clinical profile assessment help oncologist to identify the primary site from which the skeletal metastasis originated. Assessment of the clinical profile for a patient may also help a clinician to predict the expected survival time for each type of patient with unknown primary cancer and this may help to decide about the treatment strategy [9]. Thus, investigating the primary cancer type using appropriate diagnostic tool could be a preliminary yet crucial step in treating bone metastasis.
In this study, there was significant findings in the Alkaline phosphatase levels in serum at baseline, a total of 20 (46%) patients had elevated levels of alkaline phosphatase which correlated with multiple bony metastasis. Median Hemoglobin and Calcium levels in patient were 11 gm% and 9.65 mg% respectively. Renal Function Test was abnormal in 12% of disease cohort. There was no significant correlation with respect to individual laboratory parameter and survival with insignificant p value. In a study by Krishnamurthy et al. [10], where they studied distribution pattern of metastatic bone disease found an elevated serum alkaline phosphatase in 37% of the patients. There was a correlation with number (Multiple) of bone lesions and elevated serum alkaline phosphatase. This is in comparison with present study, where an elevated serum alkaline phosphatase was seen in 46% of patients and multiple bone lesions correlating with higher serum alkaline phosphatase according to Figure 1.
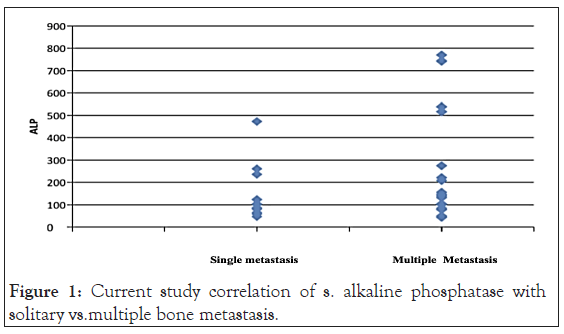
Figure 1: Current study correlation of s. alkaline phosphatase with solitary vs.multiple bone metastasis.
Histopathology and outcome
Most common histology in the present study was Adenocarcinoma in 65% patients, followed by poorly differentiated carcinoma in 14% patients. Other histologies were clear cell carcinoma, papillary carcinoma, small cell and squamous cell carcinoma. A similar histological distribution was seen in study by Takagi et al. [9], where Adenocarcinoma was the most commonly seen (56%). There is no statistically significant association of different histology and survival outcome with insignificant p value (Table 1).
| HPE | Mortality | Survival |
|---|---|---|
| Adenocarcinoma | 5 (17.9) | 23 (82.1) |
| Clear cell carcinoma | 1 (33.3) | 2 (66.7) |
| Papillary carcinoma | 1 (100.0) | |
| Poorly differentiated carcinoma | 2 (28.6) | 5 (71.4) |
| Small cell carcinoma | 1 (100.0) | |
| Squamous cell carcinoma | 3 (100.0) | |
| Note: P value=0.541 | ||
Table 1: Histopathology and outcome.
Primary site of origin
In the present study Lung cancer was the most common primary site of origin seen in 43% of patients. In a study by Singh et al. [6], where incidence and outcome of bone metastatic disease was done, where Lung cancer, breast cancer and prostate cancer had a survival of 16 months, 21 months and 20 months respectively. This is in comparison to present study. In the present study longest survival was with respect to Prostrate and Gynecological malignancies with 25 months and 24 months respectively. However, there is no significant with respect to outcome on survival with respect to primary malignancy with insignificant p value (Table 2).
| Studies | MUO Bone |
Identified primary cancers | Most common primary cancers | Primary cancer in order of frequency |
|---|---|---|---|---|
| Simon et al. [44] | 46 | 20 | Lung35% | Lung>Kidney>Breast=Prostate>Unknown |
| Nottebaert et al. [45] | 51 | 33 | Lung 51% | Lung>Others |
| Shih et al. [46] | 52 | 28 | Lung 32% | Lung>Kidney>Breast |
| Destombe et al. [8] | 107 | 94 | Lung 39% | Lung>Prostate>Breast |
| Current study | 43 | 39 | Lung 30.2% | Lung>Breast>Prostate |
Table 2: Comparison of primary site of origin with other studies.
Pain relief after local radiotherapy
Non-steroidal anti-inflammatory drugs and opioids cause symptomatic pain relief. In our study symptomatic relief was observed in 15% and 80% of the patients taking NSAIDS and opioids respectively. Radiotherapy as a treatment modality for pain relief causes significant symptomatic improvement [11-20].
In the present study 41 of the 43 patients received radiotherapy for pain relief among which 85% have had symptomatic improvement. This is in comparison with other studies as depicted in Table 3.
| Study | Number of patients treated with radiotherapy | Percentage of relief |
|---|---|---|
| Tong et al. [47] | 72 | 90 |
| Coleman et al. [4] | 16 | 100 |
| Kollender et al. [48] | 140 | 85 |
| Okawa et al. [49] | 27 | 75 |
| Present study | 41 | 85 |
Table 3: Pain relief after radiotherapy.
Response to systemic therapy
In present study, response rate to first line systemic therapy in Lung, Breast and Prostate is 38%, 33.3% and 50% respectively. The response rate of chemotherapy is not only dependent on primary but also on histopathology, Tumor biology, chemotherapeutic regimes used and demographic characteristics of the patient [21- 35]. However, there was no significant association between number of lines of therapy and outcome in present study (Tables 4 and 5).
| Primary | Response rate |
|---|---|
| Lung | 38.4% |
| Breast | 33.3% |
| Prostate | 50% |
| RCC | 33%- |
| GI & HB | 50% |
| Gynecological malignancy | 50% |
| Others | 50% |
Table 4: Comparison of response rate to systemic therapy.
| Number of lines of chemo | Mortality | Survival |
|---|---|---|
| 1 | 5 (31.3) | 11 (68.8) |
| 2 | 3 (11.5) | 23 (88.5) |
| 3 | 0 | 1 (100.0) |
| Note: P value=0.250 | ||
Table 5: Number of lines of therapy and survival outcome.
Solitary versus multiple bone metastases
In current study median survival over period of 2.5 years was 12 months with multiple bone metastasis while 20 months in patients with solitary metastasis (Table 6).
Mean (SD) |
Median |
|
|---|---|---|
| Solitary | 11.96 (5.08) | 12.00 |
| Multiple | 20.63 (7.62) | 19.50 |
| Note: P value<0.001 | ||
Table 6: Metastases and survival outcome.
This study was conducted on 43 patients with metastatic carcinoma to the bone at a presentation reporting to the Medical oncology department [35-43]. The results are summarized below.
1. The mean age of presentation in present study was 65 years, with the most common age group of presentation being 40 to 60 years. Male to Female sex ratio in present study was 1.5.
2. Most common presenting symptoms was back pain in 70% of patients followed by multiple sites of pain and pathological fracture.
3. In this study majority of our patients were ECOG PS1 37% followed by PS 2 and PS 3 21% and 23% respectively.
4. Most common laboratory parameter deranged with metastatic carcinoma to bone was S. Alkaline Phosphatase 46%.
5. Tumor markers were elevated in 19% of patients and were normal in 81% of patients; most common serum marker elevated was CEA followed by S. PSA.
6. In this study, most common cross-sectional imaging performed was CECT [A+P+T] 91% of patients followed by PETCT, Bone scan and MRI Local part respectively.
7. Most common site of bone metastasis in our study was multiple sites of metastasis in axial skeleton, in 63% patients followed by dorsal and lumbar vertebrae.
8. Most common bone biopsy site in this study was ilium 46.5% followed by Vertebral biopsy and sacrum.
9. Most common histopathology in this study was Adenocarcinoma 65.2% followed by poorly differentiated carcinoma 14% followed by Squamous cell carcinoma 7%.
10. In this study IHC was done to decipher primary origin of malignancy using various markers like CK, PSA, TTF1, Vimentin, Desmin, ER, PR, Her2Neu, CA19.9, CEA, PAX8 etc.
11. Lung carcinoma was the most common primary origin in this study 30.5% followed by breast carcinoma 14% and Prostate cancer 9.3%.
12. Zoledronate was the most common Bone modifying patient used in this study 81%.
13. Most common modality used for pain relief in this study was Radiation therapy and Systemic therapy followed by Corticosteroids and Bisphosphonates.
14. During the follow up period a total of 7 patients died due to disease progression and 1 patient was lost to follow-up. The rest are under treatment.
15. In this study Poor performance ECOG PS 3 and 4 was associated with poor survival outcomes i.e., 12 months versus ECOG PS 0, 1 and 2 was (19 months).
16. In this study multiple bone metastasis was associated with poor survival as compared to solitary metastasis at presentation 12 months versus 19.5 months which was statistically significant.
17. In this study association between primary tumour origin and overall survival was not statistically significant.
18. In this study 95% of patients underwent radiation treatment for pain management and 2 patients [5%] underwent vertebroplasty followed by radiation for spinal stabilization.
19. Number of lines of Chemotherapy was not associated with a statistically significant outcome.
20. The most common chemotherapy regimen was Paclitaxel and Carboplatin based therapy followed by Carboplatin and Pemetrexed based [44-49].
Present study is retrospective and compared clinical and demographic profile, investigations and treatment outcome of patients presenting with Metastatic carcinoma to bone with other studies. There is limited data on the clinical profile, treatment outcomes in this cohort of patients. There is paucity data in literatur e and to date there is no similar study conducted in India.
It would be kind to notice that is a few of its kind of observation study in India and literature which takes into account various aspects of metastatic carcinoma to bone ranging from epidemiological profile to treatment outcomes. None of the other studies have included the whole spectrum of metastatic carcinoma to bone under a single roof. Most of the studies in literature have not done a comprehensive analysis of various modalities of treatment like Radiation, Surgery, Chemotherapy, Endocrine therapy with response rates and overall survival hence it is difficult to get an appropriate comparative study. Few studies in literature have used radiopharmaceutical agents like Ra223, Strontium98 for management for bone metastasis, however in the present study there was no access to this treatment modality and was heavily dependent on patient financial and logistical concerns. It would be necessary to mention surgical modality was used to limited extent, similarly immunotherapy was also underutilized due to various reasons. Further prospective interventional studies with larger sample size and collaboration with orthopedic oncology surgeons, Neurosurgeons might help improve overall outcomes. Despite all such limitations every effort was made to represent the data in a very simple manner.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Rulaniya MK, Jasuja SK, Choudhary S, Dayma A, Batra H, Saknani D (2023) Clinical Profile of Patients with Metastatic Carcinoma to the Bone. J Bone Res. 11:236.
Received: 15-Mar-2023, Manuscript No. BMRJ-23-22178; Editor assigned: 17-Mar-2023, Pre QC No. BMRJ-23-22178 (PQ); Reviewed: 31-Mar-2023, QC No. BMRJ-23-22178; Revised: 07-Apr-2023, Manuscript No. BMRJ-23-22178 (R); Published: 14-Apr-2023 , DOI: 10.35248/2572-4916.23.11.236
Copyright: © 2023 Rulaniya MK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.