Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2020)Volume 11, Issue 3
Background: We aimed to compare the safety and efficacy of two techniques for the correction of subluxated
posterior intraocular lens (IOL): scleral fixation (SFIOL) and iris fixation of IOL (IFIOL).
Methods: 112 eyes of 105 patients that underwent SFIOL or IFIOL at the Kaplan Medical Center between 2008 and
2018 were retrospectively included, 73 eyes had SFIOL and 39 eyes had IFIOL. The main outcome measures were:
operation time, postoperative visual acuity and intra and post-operative complications.
Results: There was no significant difference in the mean operation time between SFIOL and IFIOL. The mean
follow-up time was significantly longer for the IFIOL compared with the SFIOL (34 ± 31 vs. 14 ± 20 months,
respectively [p>0.001]).Postoperative distance corrected visual acuity (DCVA) at the last follow-up was significantly
better than the preoperative DCVA in both groups (SFIOL: 0.52 ± 0.49 vs. 1.20 ± 0.84, [p<0.001], and IFIOL: 0.75 ±
0.88 vs. 1.31 ± 0.81 [p<0.001], respectively [LogMar]). No difference in DCVA was found between the groups.
Irregular pupil was found in 59% IFIOL vs. 20.5% of the SFIOL [p<0.001] and corneal edema was found in 10.3%
of the IFIOL vs. 1.4% of the SFIOL [p=0.05]. No other differences in intra and post-operative complications were
found between the two groups.
Conclusion: Both IFIOL and SFIOL are effective and safe for the secure of IOL in the absence of adequate capsular
support. Both techniques resulted in a significant improvement in DCVA. Pupil ovalization and corneal edema were
more common in the IFIOL group. Longer follow-up was noticed at the IFIOL group.
Cataract complication; IOL dislocation; IOL Subluxation; Sunset IOL; Scleral fixation; Iris fixation; Hoffman technique.
Posterior chamber intraocular lens (PCIOL) dislocation is a serious complication of cataract surgery. In recent years, PCIOL subluxation or dislocation following cataract extraction surgery has been reported with increasing frequency, with a cumulative risk of 0.1% after 10 years and 1.7% after 25 years [1]. Pseudoexfoliation and zonular laxity at surgery were found to be associated with late intraocular lens (IOL) dislocation [2,3].
When there is inadequate capsular support, options for secondary IOL implantation include: anterior chamber (AC) IOL, Iris supported IOL, iris fixation of IOL, and scleral fixation of IOL. Each technique offers unique advantages and disadvantages regarding surgical complexity, operative duration, and potential complications, and there is still no clear consensus on the optimal approach [4-6].
Szigiato et al. [7], in a population-based analysis of IOL exchange and repositioning in Ontario, Canada, found that from 2000 to 2013, sutured repositioning and IOL explantation procedures increased by 568% and 531%, respectively, whereas IOL exchanges without suturing decreased by 22.6%. They concluded that these increases might represent an increase in the number of surgeons who are comfortable using these techniques and could be a result of improved fellowship training in this area. Accordingly, a recent survey in Hershey, Pennsylvania, showed that 62% of surgeons were comfortable with placing scleral-fixated PCIOLs [8].
In our setting, the preferred surgical approach is repositioning of the dislocated IOL that provided adequate vision thus far, using scleral or iris fixation of the original IOL in a closed system. Kim et al. [9], in a retrospective study of 78 patients, concluded that both techniques had similar efficacy, but postoperative management should include a higher expectation of inflammation and slower recovery time for the IFIOL group. To the best of our knowledge, Kim ’ s study is the only direct comparative study between these two fixation methods.
In the present study, we aimed to retrospectively compare the safety and efficacy of SFIOL and IFIOL in a consecutive series of eyes with dislocated IOLs to ascertain any significant difference in visual outcome or complication rate in our setting.
A retrospective chart review of consecutive patients that underwent SFIOL and IFIOL of a dislocated IOL at the Kaplan Medical Center between January 1st 2008 and December 31 2018 was conducted. All operations were performed by three experienced surgeons (A.M., A.B. and G.K) using a standardized procedure.
Dislocation of the IOL was corrected in the SFIOL group using the Hoffman technique [10] and in the IFIOL group using the McCannel suture technique [11] or the Siepser sliding knot technique according to the surgeon ’ s preference. The study complies with the provisions of the Declaration of Helsinki, and was approved by the Institutional Review Board of the Kaplan Medical Center (No. 0070-18--KMC).
Hoffman technique
Two scleral pockets were made 180 degrees from each other in a meridian that facilitates proper final positioning of the IOL optic. Four paracentesis sites were prepared (superior, inferior, nasal and temporal), and a small quantity of ophthalmic viscosurgical device (OVD), either 10 mg/ml sodium hyaluronate (Biolon, Bio-Technology General Israel LTD) or 3% sodium hyalurinate + 4% chondroitin sulfate (Viscoat, Alcon, Fort Worth, Texas)was placed in the AC through one of the paracentesis to stabilize the AC. A 27 gauge needle (Pic Solutions, Grandate, Italy,) was passed through the scleral pocket and inserted into the eye, behind the iris under the IOLhaptic and into the AC. A double-armed 10-0 polypropylene blue monofilament non-absorbable suture (Prolene, Ethicon, Bridgewater, New Jersey) was inserted through an opposite paracentesis, into the 27-Gauge needle, and both were removed externally through the scleral pocket and the conjunctiva. The 27-gauge needle was again passed through the conjunctiva and the full thickness of the scleral pocket and inserted into the eye, but this time anterior to the IOL haptic and into the AC. The second arm of the double-armed 10-0 prolene suture was passed through the same opposite corneal paracentesis into the 27- gauge needle; both were again retrieved outside of the eye. The same technique was performed on the opposite IOL haptic using the second scleral pocket and the opposing paracentesis. Sutures were retrieved outside of the scleral pocket and tied. The suture knot was trimmed. Vitrectomy was not routinely performed with the repositioning procedure, but when required, a limbal or pars plana approach, as indicated, was used.Two scleral pockets were made 180 degrees from each other in a meridian that facilitates proper final positioning of the IOL optic. Four paracentesis sites were prepared (superior, inferior, nasal and temporal), and a small quantity of ophthalmic viscosurgical device (OVD), either 10 mg/ml sodium hyaluronate (Biolon, Bio-Technology General Israel LTD) or 3% sodium hyalurinate + 4% chondroitin sulfate (Viscoat, Alcon, Fort Worth, Texas)was placed in the AC through one of the paracentesis to stabilize the AC. A 27 gauge needle (Pic Solutions, Grandate, Italy,) was passed through the scleral pocket and inserted into the eye, behind the iris under the IOLhaptic and into the AC. A double-armed 10-0 polypropylene blue monofilament non-absorbable suture (Prolene, Ethicon, Bridgewater, New Jersey) was inserted through an opposite paracentesis, into the 27-Gauge needle, and both were removed externally through the scleral pocket and the conjunctiva. The 27-gauge needle was again passed through the conjunctiva and the full thickness of the scleral pocket and inserted into the eye, but this time anterior to the IOL haptic and into the AC. The second arm of the double-armed 10-0 prolene suture was passed through the same opposite corneal paracentesis into the 27- gauge needle; both were again retrieved outside of the eye. The same technique was performed on the opposite IOL haptic using the second scleral pocket and the opposing paracentesis. Sutures were retrieved outside of the scleral pocket and tied. The suture knot was trimmed. Vitrectomy was not routinely performed with the repositioning procedure, but when required, a limbal or pars plana approach, as indicated, was used.
Iris fixation technique
Two or three paracentesis sites were prepared, and OVD (10 mg/ml sodium hyaluronate [Biolon, Bio-Technology General Israel LTD] or 3% sodium hyalurinate+4% chondroitin sulfate [Viscoat, Alcon]) was placed in the AC. The optic was prolapsed above the iris plane and captured by the pupil. After pupillary constriction with acetylcholine hydrochloride (Miochol, Bausch and Lomb, Rochester, New York) or Carbachol 0.01% (Miostat, Alcon) a 10-0 polypropylene blue monofilament non-absorbable suture (Prolene, Ethicon) on a long curved needle was used to suture the IOL to the iris using the McCannel suture technique or the Siepser sliding knot technique. Anterior vitrectomy was performed as needed.
The postoperative treatment included Ofloxacin 0.3% (Oflox, Allergan, Dublin, Ireland ) drops six times a day for seven days and dexamethasone sodium phosphate 0.1% (Sterodex, Dr. Fischer LTD, Bnei-Brak, Israel) six times a day for seven days and then tapered down for four weeks. Patients with diabetes mellitus were treated also with diclofenac sodium 1 MG/ML drops (Novartis, Basel, Switzerland) four times a day for 2-3 months.
Data collection
The patients ’ charts were retrospectively reviewed for patient demographics, systemic conditions at presentation, ophthalmic history, ophthalmic exam, follow-up duration, type of IOL implanted, the interval between the initial operation and the development of IOL dislocation, axial length measurement and automated keratometry (performed by an IOLMaster™ [version 5.4.4.006, Carl Zeiss, Meditec AG, Jena, Germany]( and intraand post-operative complications.
Charts were also reviewed for preoperative, first follow-up (usually seven days postoperatively) and last follow-up for distance-corrected visual acuity (DCVA). Visual acuity (VA) was measured using a Snellen chart, and converted to the logarithm of the minimal angle of resolution (logMAR) for analysis [12]. During the final follow-up visit after fixation surgery, subjective refraction was performed by a skilled hospital-based optometrist.
Statistical analysis
Statistical analyses were performed using SPSS, version 21.0 (SPSS Inc, Chicago, Illinois, USA). Continuous variables were compared between the two-groups using independent samples ttest or Mann Whitney U test, as indicated by a normality test (Shapiro-Wilk). Categorical variables were compared using Pearson X2 or Fisher's exact tests, as appropriate. Differences in visual acuities within each group were compared using Wilcoxon signed rank test. A P-value less than 0.05 was considered statistically significant.
One hundred thirty-two eyes had PCIOL reposition and fixation procedures. Six eyes that had a previous IOL repositioning operation, seven eyes that had less than three weeks of follow-up and seven eyes that underwent the Yamane technique [13] SFIOL were excluded. A total of 112 eyes of 105 patients that underwent SFIOL and IFIOL were included in this study, 73 eyes in the SFIOL group and 39 eyes in the IFIOL group.
Baseline characteristics of patients
The patients’ baseline demographic and ocular characteristics are summarized in Table 1. The mean age of patients in the SFIOL group was significantly older than that of the IFIOL group, (79.3 ± 7.8 years vs. 73.0 ± 13.8, p=0.02). Additionally, there were more male patients in the IFIOL group (71.8% vs. 42.5%, p=0.003). Time from the primary cataract surgery to fixation surgery was significantly longer for the SFIOL compared with the IFIOL (9.2 ± 6.3 years vs. 4.7 ± 6.1 years, p=0.002). Mean follow-up time was significantly longer for IFIOL compared with SFIOL (14.0 ± 20.0 vs. 34 ± 31 months, respectively, p>0.001). There was no intergroup difference in preoperative ocular characteristics and comorbidities. More eyes in the IFIOL group had intraoperative complications in the primary cataract surgery (23.1% vs. 4.1%, p=0.009). More eyes in the IFIOL group had postoperative complications after the primary cataract surgery (20.5% vs. 2.7%, p=0.002).
| IFIOL Group(n=39) | SFIOL Group (n=73) | p Value | |
|---|---|---|---|
| Baseline Demographic Characteristics | |||
| Age at operation (mean ± SD, yrs) | 73.0 ± 13.8 | 79.3 ± 7.8 | 0.021⃰1 |
| Sex (Male) | 0.718 | 0.425 | 0.003⃰2 |
| Laterality (OD) | 0.436 | 0.452 | 0.872 |
| Time from Primary Surgery˜ (mean ± SD, yrs) | 4.7 ± 6.1 | 9.2 ± 6.3 | 0.002⃰1 |
| Mean Follow-up Duration (months) | 33.8 ± 31.2 | 14.0 ± 20.0 | <0.001⃰1 |
| Ocular Characteristics | |||
| DCVA Before Operation (LogMAR) | 1.31 ± 0.80 | 1.2 ± 0.84 | 0.3951 |
| Corneal Astigmatism (diopters) | 1.4 ± 1.3 | 1.5 ± 1.4 | 0.5461 |
| Axial Length (mm) | 24.6 ± 1.9 | 24.5 ± 1.9 | 0.3751 |
| Average K | 43.70 ± 1.95 | 43.69 ± 1.54 | 0.6371 |
| Ocular comorbidities | |||
| Pseudoexfoliation | 0.41 | 0.493 | 0.42 |
| Glaucoma | 0.231 | 0.233 | 0.982 |
| AMD | 0.026 | 0.068 | 0.662 |
| Diabetic Retinopathy | 0.026 | 0.027 | 12 |
| Amblyopia of Operated Eye | 0.154 | 0.041 | 0.0632 |
| Myopia (AL>26 mm) | 0.077 | 0.137 | 0.5372 |
| Additional Surgeries to Cataract in the Past | 0.231 | 0.123 | 0.142 |
| Ocular Trauma | 0.051 | 0.086 | 0.712 |
| Primary Cataract Surgery˜ | |||
| Zunulolysis | 0.205 | 0.096 | 0.12 |
| Intra-surgical Complications* | 0.231 | 0.041 | 0.003⃰2 |
| Post-operative Complications° | 0.205 | 0.027 | 0.003⃰2 |
IFIOL: Iris Fixation Of Posterior Chamber Intraocular Lenses, SFIOL: Scleral Fixation of Posterior Chamber Intraocular Lenses, OD: Right Eye, DCVA: Distance Corrected Visual Acuity, AMD: Age-Related Macular Degeneration. AL: Axial Length.1 Mann-Whitney Test 2 Pearson Chi-SquareorFisher's Exact Test ˜Excluding cases of IOL fixation in primary cataract surgery.*Including: in-the-bag IOL dislocation (n=2), ruptured posterior capsule (n=2), cortical lens remnants (n=2), anterior vitrectomy (n=1), switching from Phacoemulsification to Extra Capsular Cataract Extraction (ECCE, n=1), deformity of iris that required iridoplasty (n=1), and others not documented (n=3)
Table 1: The Patients’ demographic and ocular characteristics.
IOL repositioning and fixation surgery
Four eyes (5.5%) in the SFIOL group and six (15.4%) in the IFIOL group, p=0.09, underwent IOL fixation in the primary cataract surgery. One eye (1.4%) in the SFIOL group and one eye (2.6%) in the IFIOL group had secondary fixation of IOL for aphakia. In the SFIOL group, five eyes (6.8%) had pars-plana vitrectomy (PPV) in the IOL fixation operation, and one eye (1.4%) was implanted with the Mini Ex-Press Glaucoma Shunt. In the IFIOL group seven eyes (17.9%) had PPV in the IOL fixation operation, one eye (2.6%) had a trabeculectomy (Ab Externo) and one eye (2.6%) was implanted with the Mini Ex- Press Glaucoma Shunt. In one eye (2.6%) IFIOL was performed after a failed attempt at performing SFIOL.
Outcomes and Complications
There was no significant difference in operation time between the SFIOL and the IFIOL (Table 2). Postoperative DCVA at last follow-up improved significantly compared with preoperative DCVA in both groups (p<0.001 in both groups). No significant differences in mean DCVA, spherical equivalent and absolute astigmatism at the last follow-up were found between the two groups. In the last follow-up, more than 50% of patients in both groups had a DCVA equal or better than 20/40 (Figure 1).
| IFIOL Group (n=39) | SFIOL Group (n=73) | P Value1 | |
|---|---|---|---|
| Surgery Time (min), mean ± SD | 84.1 ± 39.3 | 77.36 ± 35.4 | 0.39 |
| DCVA 7 days postoperatively (LogMAR)mean ± SD | 1.24 ± 0.84 | 1.03 ± 0.82 | 0.12 |
| DCVA at Last Follow-up (LogMAR)mean ± SD | 0.74 ± 0.88 | 0.52 ± 0.49 | 0.57 |
| Spherical Equivalent Dmean ± SD | (-)1.8 ± 3.1 | (-)1.8 ± 1.9 | 0.31 |
| Astigmatism (absolute) D mean ± SD | 1.8 ± 1.0 | 1.7 ± 1.9 | 0.93 |
| Astigmatism (centroid) D mean ± SD @ axis | 0.8 ± 1.9 @ 177 | 1.1 ± 2.3 @ 19 | X-Axis=0.71 Y-Axis=0.11 |
IFIOL: Iris Fixation of Posterior Chamber Intraocular Lenses, SFIOL: Scleral Fixationof Posterior Chamber Intraocular Lenses, DCVA – Distance Corrected Visual Acuity, LogMAR: Logarithm of the Minimum Angle of Resolution.
1Mann-Whitney Test
Table 2: Postoperative Outcomes: IFIOL Group vs. SFIOL Group.
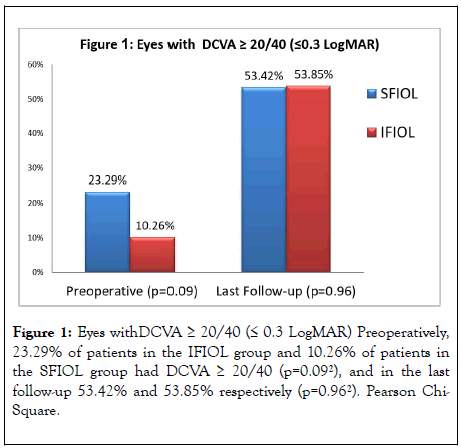
Figure 1: Eyes withDCVA ≥ 20/40 (≤ 0.3 LogMAR) Preoperatively, 23.29% of patients in the IFIOL group and 10.26% of patients in the SFIOL group had DCVA ≥ 20/40 (p=0.092), and in the last follow-up 53.42% and 53.85% respectively (p=0.962). Pearson Chi- Square.
Early and late postoperative complications are detailed in Table 3. Irregular pupil was significantly more common in the IFIOL group (21.3% in the SFIOL group and 59% in the IFIOL group, p<0.001). Persistent corneal edema (more than one month postoperatively) was observed more in the IFIOL group (1.4% in the SFIOL group vs. 10.3% in the IFIOL group, p=0.05). Two eyes in the IFIOL group had descemet stripping automated endothelial keratoplasty (DSAEK). Hypotonic eye (intraocular pressure<5 mmHg) was noted postoperatively in three cases in the SFIOL group and in none of the cases in the IFIOL group but the difference was not statistically significant (p=0.55).
| IFIOL Group (n=39) | SFIOL Group (n=73) | p-Value2 | |
|---|---|---|---|
| Early Complications (<1 month) | |||
| Subconjunctival Hemorrhage | 10 (25.6%) | 28 (38.4%) | 0.18 |
| Transient Corneal Edema | 25 (64.1%) | 46 (63.0%) | 0.91 |
| Fibrin in Anterior Chamber | 2(5.1%) | 2 (2.7%) | 0.61 |
| Intraocular pressure>30 mmHg | 4 (10.3%) | 7 (9.6%) | 1 |
| Intraocular pressure<5 mmHg | 0 (0%) | 3 (4.1%) | 0.55 |
| Hyphema | 5 (12.8%) | 10 (13.7%) | 0.9 |
| Vitreous Hemorrhage | 2(5.1%) | 4 (5.5%) | 1 |
| Retinal Detachment | 0 (0%) | 1 (1.4%) | 1 |
| Choroidal Hemorrhage | 1 (2.6%) | 1 (1.4%) | 1 |
| Lens Decentration/Tilt | 4 (10.3%) | 9 (12.3%) | 1 |
| Late Complications (>1 month) | |||
| Irregular Pupil | 23 (59%) | 15 (20.5%) | <0.001⃰ |
| Elevated Intraocular Pressure>21 mmHg | 0 (0%) | 3 (4.1%) | 0.55 |
| Corneal Edema | 4 (10.3%) | 1 (1.4%) | 0.05⃰ |
| Anterior uveitis | 0 (0%) | 1 (1.4%) | 1 |
| Pseudophakic Cystoid Macular Edema | 1 (2.6%) | 2 (2.7%) | 1 |
| Recurrent Fixation Operation | 3 (7.7%) | 6 (8.2%) | 1 |
IFIOL: Iris Fixation Of Posterior Chamber Intraocular Lenses; SFIOL: Scleral Fixation Of Posterior Chamber Intraocular Lenses
2 Pearson Chi-Square
Table 3: Early and Late Complications:IFIOL Group vs. SFIOL Group.
In one case, it was due to choroidal detachment and in the two other cases, there was a leaking suture. The incidence of IOL decentration noted in the first follow-up examination with pharmacologically dilated pupils (usually 1 week postoperatively) was 10.3% in the IFIOL group and 12.3% in the SFIOL group (p=1.00). The incidence of recurrent dislocation that required an additional fixation procedure was around 8% for both groups (p=1.00).
In this study, we found that IFIOL and SFIOL are effective and safe for the treatment of IOL subluxation. Visual acuity improved significantly in both groups, and remained stable for a mean follow-up time of more than 12 months. We found no significant difference in the last follow-up DCVA or the spherical equivalent between the two fixation techniques.
Our findings are in line with results of prior studies of IOL fixation in the absence of capsular support, which show that visual outcomes improve regardless of IOL selection and surgical techniques.6-8 Kim et al.9 compared the outcomes of IFIOL (n=35) vs. SFIOL (n=44) and showed that both groups had significant improvements in DCVA. They found that visual acuity improvement in the SFIOL group was faster than in the IFIOL, and there were fewer astigmatic errors in the SFIOL group. Preoperatively, DCVA was 0.58 LogMAR in the IFIOL and 0.57 LogMAR in the SFIOL and postoperatively 0.25 and 0.19 respectively. The patients in our study were older than in Kim et al’s study; the mean age in their study was 61.2 years in the SFIOL group and 56.9 in the IFIOL while it was 78.2 and 73.0 respectively in our study. This difference might explain the better preoperative and postoperative DCVA in the preceding work. Nevertheless, the study population baseline characteristics in our study are comparable to published IOL fixation data, and so is the mean DCVA at the last follow-up [1,6,14-20].
Pseudoexfoliation syndrome, the most common risk factor for late IOL dislocation1 was observed in more than 40% of patients in both groups in the present study. Other associated conditions predisposing to IOL subluxation: additional ocular surgeries, axial length of more than 26 mm and ocular trauma in the past, were noted in a smaller percentage of the patients.
When there ’ s insufficient capsular support in the primary cataract surgery, management decisions are based on the surgeon’s preference and experience. Iris fixation is easier in this situation due to the relative difficulty to create scleral pocket in an open hypotonic eye. Therefore, more cases in the IFIOL group (15.4% vs. 5.5%) were performed in the primary cataract surgery. This may explain some of the differences in the patients’ baseline data: age (younger for IFIOL), complications in the primary cataract surgery (more for IFIOL) and mean interval between primary cataract surgery and fixation surgery (shorter for IFIOL). Additionally, this may also explain the longer mean surgery time in the IFIOL group in the present study (84.1 ± 39.3 minutes) compared with Kim et al (37.9 ± 68.5 minutes) [9].
Pupil ovalization, a well-known complication of IFIOL, was significantly more common in the IFIOL group (59% vs. 21.3% in the SFIOL group). The degree of pupil ovalization was variable, from only mildly distorted pupil to oval pupil. Pupil ovalization is mainly an aesthetic concern, but it may also cause visual symptoms such as glare or halo. Most published studies did not report the incidence of eyes with surgically induced irregular pupil [9,21-24]. Michaeli et al. [19] reported an incidence of 48% pupil ovalization, which is comparable to our findings (59%).
The incidence of persistent corneal edema, representing endothelial decompensation, and longer follow-up period, also found to be higher in the IFIOL group than in the SFIOL group.That could suggest a less favorable outcome, but this finding may be related to the higher intraoperative and postoperative complication rate in the primary cataract surgery in the IFIOL group, and not to the fixation technique. It is important to note that in one of the two cases of corneal edema that eventually led to DSAEK, the IFIOL was performed in the primary cataract surgery. Kim et al9 also showed a trend towards more endothelial cell loss in the IFIOL group (12.7 ± 8.7% vs. 10.9 ± 9.2%, p=0.16), but the difference was not statistically significant.
Other specific complications associated with IFIOL include pigment dispersion, chronic iritis, peripheral anterior synechia formation, and pupillary distortion [19,21,22]. SFIOL also carries potential risks, including: refractive instability owing to lens tilt and decentration, intraocular hemorrhage owing to the passage of a needle through vascular uveal tissue, suture breakage and late endophthalmitis [25-27].
The reported incidence of recurrent dislocation ranges from 2% to 10%.3,24-29 In the current study, similarly to Kim et al. [9], recurrence rates were comparable in the SFIOL and IFIOL groups (7.7% in the IFIOL vs. 8.2% in the SFIOL). Postoperative retinal detachment developed in only 1 patient, 0.8%, while previous reports describe higher incidence of 1 to 8%.3,6,16,17,20,24-26,28 However, this can be related to the length of the follow-up period. Postoperative hyphema, including micro-hyphema, was noted in around 12% of the patients in both groups, and vitreous hemorrhage in 5-6%. All the cases of vitreous hemorrhage cleared spontaneously and none of the patients underwent vitrectomy due to the postoperative hemorrhage. Postoperative CME was previously reported in 1% to 12% of patients [3,16,17,24-29] in our study less than 3% of the eyes developed CME post operatively in both groups.
While immediate postoperative inflammation was significantly more severe in IFIOL in Kim et al. [16] study, in the present study AC cells were observed at first follow-up in around 60% of patients in both groups. Uveitis more than a month postoperatively was observed only in one case, in the SFIOL group. There were no cases of endophthalmitis, and in the SFIOL group no knot exposure reported.
The strength of the current study lies in its relatively large number of participants: a total of 112 eyes. To the best of our knowledge, this is the largest direct comparative study between these two fixation methods. This study has some limitations, including the retrospective nature of the study and the lack of randomization.
In conclusion, we suggest that IFIOL and SFIOL have similar efficacy in terms of visual outcome and safety, with a mean follow-up of more than 12 months. We found comparable rates of complications, except for more pupil ovalization and more endothelial cell decompensation in the IFIOL group. The latter finding maybe partially related to the higher rates of IFIOL in the primary cataract operation. Longer follow-up period was noticed at the IFIOL group, which could suggest less favorable outcome. A larger, prospective study with a longer follow-up time is needed to confirm our results.
Value statement
What was known:
• IOL Subluxation frequency has increased in recent years.
• Techniques to correct IOL subluxation include: IOL exchange, scleral-sutured and iris-sutured fixation of the subluxated IOL.
• Ocular comorbidities and postoperative complications may limit the outcomes of IOL reposition and fixation procedures.
What this paper adds:
• Visual acuity improves significantly in both iris and scleral fixation groups.
• Pupil ovalization and longer follow-up time were more common in the Iris fixation group. This could suggest a less favorable outcome in this group.
Citation: Levy-Neuman S, Marcovich A, Bukelman A, Reitblat O, Kleinmann G (2020) Clinical Outcomes of Iris vs. Scleral Intraocular Lens Fixation. J Clin Exp Ophthalmol. 11:840. DOI: 10.35248/2155-9570.20.11.840
Received: 04-May-2020 Accepted: 18-May-2020 Published: 25-May-2020 , DOI: 10.35248/2155-9570.20.11.840
Copyright: © 2020 Levy-Neuman S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.