International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Mini Review - (2020)Volume 8, Issue 3
Few reports have been published examining cervical foraminal stenosis as the cause of drop finger. This mini-review, therefore, will provide a summary of the findings of articles published on this topic, written in both English and Japanese. Cervical foraminal stenosis is difficult to diagnose from imaging findings alone; thus, physical examination findings are often needed to make a firm diagnosis. Numbness of the fingers, the extent of interscapular pain, and finger posture can be used to differentiate drop finger due to cervical foraminal stenosis from other diseases. It is crucial to provide sufficient explanation to the patient before a decompression surgery is performed because the recovery of muscle strength is often incomplete and the improvement may be small.
Drop finger; Cervical foraminal stenosis; C7 nerve root; C8 nerve root
CFS: cervical foraminal stenosis; PION; Posterior Interosseous Nerve; ECR; Extensor Carpi Radialis; EDM; Extensor Digiti Minimi; EIP; Extensor Indicis Proprius
Cervical foraminal stenosis (CFS) can often lead to the development of nerve palsy. It has been reported that C7 and C8 nerve root palsy are associated with drop finger, which can cause difficulty in grasping or pressing keys on a personal computer and thus significantly restrict daily life [1]. In fact, there are few reports on the diagnosis and surgical results of the drop finger derived from cervical spine disease, and the diagnosis algorithm is not generalized. Therefore, in this minireview, we examined papers on the topic published in both English and Japanese.
We searched the PubMed and the Japan Medical Abstracts Society databases with the key terms “drop finger and cervical” or “drop finger and C8” or “drop finger and C7” or “Kasuishi” (the Japanese term for drop finger), with the date restriction of 1980 to 2020.
The search obtained three case reports, one clinical feature, and one surgical outcome from PubMed, whereas two case reports and two reviews came from the Japan Medical Abstracts Society.
Diseases that need to be differentiated from cervical spine-derived drop finger
Drop finger due to CFS exhibits a similar finger posture to that which occurs due to ulnar nerve palsy (also referred to as “ pseudo-ulnar palsy ” and “ pseudo claw hand ” [2,3]); thus, differential diagnosis might be difficult to determine. Furthermore, posterior interosseous nerve (PION) palsy has also been suggested to exhibit similar symptoms and thus require differentiation [4].
Specific diagnosis of cervical foraminal stenosis-derived drop finger
It is often difficult to diagnose CFS at the C6/7 or C7/Th1 levels by imaging such as magnetic resonance imaging (MRI), computed tomography (CT), myelo-CT alone. We have tasked five spine surgeons, with more than 5 years of spine surgery experience, to identify the level of the decompressed nerve root from sagittal and axial MRI and CT images at the C6/7 and C7/Th1 levels; it was found out that the accuracy of their identification was only at 62% (unpublished data). Thus, it is clear that in order to make a comprehensive judgment, image findings must be considered alongside with the results of physical examinations.
A study involving 12 cases of drop finger due to CFS reported the following findings: (1.) Drop finger often follows pain in the interscapular region, (2.) it is not uncommon for patients to lack pain in the upper limb or finger, and (3.) muscle weakness in the triceps brachii and muscles of the hands is present in all cases of drop finger 4).
Among the 22 cases of drop finger due to CFS in the studies that our search returned, we identified 3 types of finger posture during fingers extension at the middle position of the wrist joint (Figure 1). Our classification into Type I, II, and III patterns included 6, 13, and 3 cases, respectively [1].
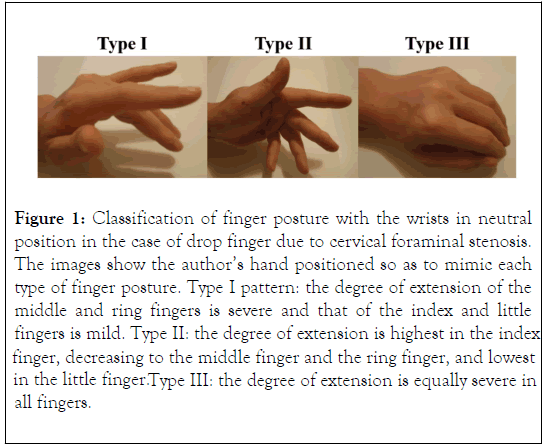
Figure 1. Classification of finger posture with the wrists in neutral position in the case of drop finger due to cervical foraminal stenosis. The images show the author’s hand positioned so as to mimic each type of finger posture. Type I pattern: the degree of extension of the middle and ring fingers is severe and that of the index and little fingers is mild. Type II: the degree of extension is highest in the index finger, decreasing to the middle finger and the ring finger, and lowest in the little finger.Type III: the degree of extension is equally severe in all fingers.
After evaluating the pre-operative macrophotographs, the study of Tanaka et al. included one case of Type II and one case of Type III, that of Hori et al. included one case of Type I, and the study of Kaneko et al. included one case of Type II. All the five cases examined on macrophotographs were found to align with one of our classifications [4-7].
Anatomically, the C7 and C8 nerve roots branch and join together in the brachial plexus, finally emitting nerve fibers to the radial, ulnar, and median nerves. Thus, understanding the difference between the drop finger postures that occur due to peripheral neuropathy and CFS requires an in-depth understanding of the innervation to the muscles.
Table 1 shows the level of upper limb muscle power in the case of each disease. Based on this, we developed an algorithm for the identification of diseases that need to be differentiated from drop finger due to CFS (Figure 2).
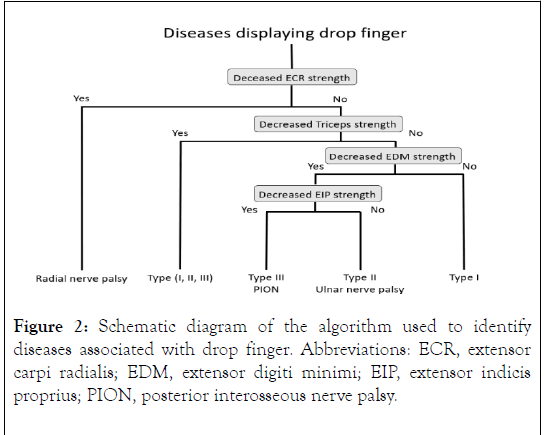
Figure 2. Schematic diagram of the algorithm used to identify diseases associated with drop finger. Abbreviations: ECR, extensor carpi radialis; EDM, extensor digiti minimi; EIP, extensor indicis proprius; PION, posterior interosseous nerve palsy.
| ECR (C6) | Triceps (C8) | EDM (C7,C8) | EIP (C7,C8) | |
|---|---|---|---|---|
| CFS Type I | → | → or ↓ | → | → |
| CFS Type II | → | → or ↓ | ↓ | → |
| CFS Type III | → | → or ↓ | ↓ | ↓ |
| PION palsy | → | → | ↓ | ↓ |
| Ulnar nerve palsy | → | → | ↓ | → |
| Radial nerve palsy | ↓ | → | ↓ | ↓ |
Definitions: →, within the normal range of muscle power, ↓, decreased muscle power. Abbreviation: CFS: Cervical Foraminal Stenosis; ECR: Extensor Carpi Radialis; EDM; Extensor Digiti Minimi; EIP; Extensor Indicis Proprius; PION: Posterior Interosseous Nerve.
Table 1: Degree of muscle power of upper limb associated with each disease and finger posture.
When drop finger is encountered in the clinic, and if triceps brachii muscle weakness is observed but no muscle weakness in the extensor carpi radialis (ECR), then it is highly likely that CFS is the cause of the condition.
Even when triceps muscle weakness is not seen, Type I finger posture is relatively unique, and, thus, it can be comparatively easy to diagnose.
Type II, which is similar to the finger posture reported by William et al. (pseudo-ulnar palsy), is more difficult to distinguish from ulnar nerve palsy [3].
The ring and little fingers are extended at the metacarpophalangeal joints and flexed at the interphalangeal joints, which results in an ulnar claw position. In contrast, drop finger that develops due to CFS is associated with a finger posture in which the ring and little fingers are extended at the interphalangeal joints and flexed at the metacarpophalangeal joints [1].
Type III, which was observed in the study of Tanaka et al. [4], exhibits similar finger posture as is seen in PION and involves severe paralysis.
Thus, it is difficult to discriminate between CFS presenting Type III posture and PION by finger posture alone. Since PION is solely paralysis of the motor nerve fibers, it is important to evaluate electromyography findings, numbness, and paresthesia in order to determine the cause of drop finger.
Differences between C7 and C8 radiculopathy as a cause of drop finger
It has been reported that, in the case of CFS with drop finger, impaired nerve roots in the range of interscapular pain are mostly associated with C8 root disorders, with some C7 root disorders being noted [4,8].
We defined that nerve root disorders abnormal perioperative findings included radicular flattening and hyperemia and researched the relation with drop finger type and nerve root disorders. The results are as follow.
Type I finger posture was identified in five cases of C7 and one case of C8 nerve root disorders, while Type II was observed in eight cases of C8 nerve root disorder and five cases of combined C7 and C8 nerve root disorders. Type III was only observed in cases of C8 nerve root disorders (three cases).
These results suggest that the Type I finger posture is indicative of C7 nerve disorders, while Types II and III are suggestive of C8 nerve disorders [1].
Surgical results
Tanaka et al. reported that the postoperative improvement in drop finger is related to duration of disease. They explained that drop finger due to radiculopathy should be treated promptly without conservative therapy in order to improve patient outcomes [4].
Hori et al. reported seven cases of surgical results, some of which showed recovery of muscle strength 1 year postoperatively, highlighting the importance of continuing observation over a long period [6].
Kawada and colleagues reported that five patients who underwent surgery for drop finger due to C8 radiculopathy experienced improved muscle strength, although none recovered to normal levels [8,9]. Koda et al. reported that, in 17 consecutive cases of drop finger associated with C8 nerve root lesions, 9 experienced improved extensor digitorum muscle following surgery, while 8 reported no improvement.
The authors also reported poor improvement in cases where severe paralysis was recorded before surgery [10].
Our review found that in all 22 cases, surgery resulted in the improvement of the strength of some muscles [1]. However, most cases did not experience complete recovery; These results are the same as those reported by Kawada et al.
Type I or Type II finger posture showed good improvement after surgery, whereas those with Type III posture reported strong preoperative paralysis and poor improvement after surgery. These results are in line with those of Koda et al. and Tanaka et al.
Before surgery, we find it necessary to explain to the patient that the recovery of muscle strength is often incomplete and the improvement may be small (Table 1).
Finger numbness, range of interscapular pain, and finger posture can be used to distinguish drop finger caused by CFS from other diseases. For most patients, surgery is recommended, but it is important to provide the patient with sufficient explanation prior to surgery, due to the risk that muscle strength will not be completely restored and the poor rate of improvement.
The authors declare that they have no conflict of interest.
Citation: Furukawa M, Kamata M (2020) Classification of Finger Posture in Drop Finger Due to Cervical Foraminal Stenosis: A Mini-Review. Int J Phys Med Rehabil. 8:548. DOI: 10.35248/2329-9096.20.08.548
Received: 20-Apr-2020 Accepted: 11-May-2020 Published: 18-May-2020 , DOI: 10.35248/2329-9096.20.08.548
Copyright: © 2020 Furukawa M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.