Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Research Article - (2023)Volume 11, Issue 4
Many trauma patients die with secondary injury by immune dysregulation where lymphocytes play an important role in immune response. This was a retrospective cohort study of adult severe trauma patients. The patient’s lymphocytes were collected in 0-3(A), 6-12(B), 24-48(C), and 49-72(D) hours after trauma. The degree of secondary injury was determined according to laboratory and clinical records. Lymphocytes play crucial role in immune response, by attacking foreign substances, such as bacteria, viruses, and other pathogens, to help protect the body from infections and diseases. In case of cardiovascular system, lymphocytes can have both beneficial and detrimental effects. Blood lymphocytes, particularly T cells and B cells, can impact the cardiovascular system through their involvement in inflammation, immune responses, and autoimmune diseases. While their actions can contribute to the development and progression of cardiovascular conditions, they also have important regulatory functions that help maintain cardiovascular health. The correlation between lymphocytes and secondary injury was analyzed, in this study.
The lymphocytes in 71.2% of A group patients increased higher than the upper limit of normal range. On the contrary, the lymphocytes were less than the low limit of normal range in 62% of the other groups. The lymphocytes ratio of group B,C,D by that group A were calculated, the medians were 0.21-0.22. A significantly correlation between lymphocytes ratio and severe degree of secondary injury in the trauma patients (P=0.000), the lymphocyte counts ratio can be predicting degree of secondary injury of trauma patients. Lymphocytes significantly increased in the severe trauma patients within 3 hours, then decreased significantly in 6 to 72 hours after trauma. By calculating lymphocytes ratio in early time after trauma can be used to predict the degree of secondary injury, and there was better sensitivity and specificity.
Lymphocyte counts; Severe trauma; Secondary injury
Improvements in early resuscitation and promotion of damage control surgery ensure that many patients with trauma to survive. However, two-thirds of patients die from a secondary injury in the later trauma period. Tissue injury due to trauma initiates the release of a large number of cytokines that lead to immune activation and induce major immune dysregulation. Patients may present Severe Systemic Inflammatory Response (SIRS) or Compensated Anti-Inflammatory Immune Response Syndrome (CARS). The direct or indirect interactions between SIRS and CARS aggravate secondary injury [1-3]. In addition, the degree of secondary injury in patients with trauma is associated with level of inflammation. Severe inflammatory reaction eventually leads to tissue injury, Multiple Organ Dysfunction Syndromes (MODS), and severe shock [4,5]. In the treatment of patients with severe trauma, it is important to detect those at high risk for lethal outcomes early on. In clinical work, we have found that many patients with severe trauma have significant changes in the number of lymphocytes early after injury. Lymphocytes often play an important role in the immune response. Therefore, changes in lymphocyte counts and expression in patients with trauma could be associated with post-traumatic inflammatory response [6,7]. Lymphocyte count is a readily available parameter, it can be used as an index with high cost effective to evaluate the degree of secondary injury after trauma. In this study, we conducted a retrospective analysis of the trauma patients with Injury Severity Score (ISS) greater than 16 admitted to our Intensive Care Unit (ICU) to evaluate whether there is a correlation between changes in lymphocyte counts and the degree of secondary injury in patients with trauma and assess the feasibility of identifying the changes in lymphocyte counts to predict the degree of secondary injury
Study setting
This was a retrospective study on severe trauma patients (ISS scores ≥ 16) admitted between January 2018 and October 2021 in the ICU of Longgang Central Hospital of Shenzhen, a tertiary hospital of Shenzhen City, Guangdong, China. The aim of this study is to evaluate the feasibility of assessing the change of the lymphocyte counts in early time after trauma in trauma patients as a useful predictor of severe degree of secondary injury. To better evaluate the characteristics of lymphocyte count changes in trauma patients, a certain number of non-surgical and nontraumatic patients in ICU were randomly selected as control group in same period. The study setting and data collection were approved by the Medical Ethics Committee of the hospital. This retrospective study will not interfere with the treatment of patients, will not cause damage to the rights of patients. The clinical data collection of the patients were agreed with the written consent of the patients and their families, and all the study protocols were agreed by the patients or their families, the paper of approval content form was preserved in patient medical history records.
Patients
Demography: The patients’ age, sex, injury mechanism and site, time from the scene to the Emergency Department (ED); the kind (crystals, blood products, etc.) and quantity of fluid infusion on the patients within first three days after trauma were recorded, ISS score was calculated and recorded according to scoring Criteria published by China Trauma Treatment Alliance (http://www. ctrta.org.cn).
Exclusion criteria: The patient’s age was older than 70 years or younger than 14 years; the patients with burn injury; the patients died within 24 hours after trauma or death caused by trauma directly, the patients with infused crystal fluid more than 4000 ml or transfusion of packed red blood cells exceeding 10 units in first 8 hours after trauma; the patients with chronic important organs disease history, or with had been taken of any immune inhibitor or a history of autoimmune disorders Recently; the patients with a history of hospitalization or operation within the last month; the patients transferred from other hospitals, or the time from scene to ED was over 3 hours, or stayed in the hospital less than 24 hours; or the number of required laboratory results is less than 50%.
Data collection and evaluation
Lymphocyte count: All of the blood samples of the patients obtained by trained qualified medical staff in the ED and the ICU of the hospital and tested using automatic blood analyzer (XT-1800i, Sysmex Corporation, Tokyo, Japan) in the laboratory of the hospital. The results of the lymphocyte counts of the trauma patient were collected and recorded according to within the 3 hours (trauma group A, TrA), 6-12 hours (trauma group B, TrB), 24-48 hours (trauma group C, TrC), and 49-72 hours (trauma group D, TrD) after trauma. If there were two or more results in the same period, the maximum variation value was selected. The results of the lymphocyte counts of control group were obtained at the same time interval when admission in ICU, also divided four groups according to same time period.
Evaluation of the degree of secondary injury in the trauma patient
Three aspects of data for comprehensive evaluation were collected. The results of laboratory test which are the values of Lactic Dehydrogenase (LDH) and Creatine Kinase (CK), C Reactive Protein (CRP), Procalcitonin (PCT) and Neutrophile (NE) in each studied patient were collected as well from the clinical laboratory information system of the hospital within 24-72 hours after trauma.
Clinical evaluation: The analysis indicators include System Inflammatory Response Syndrome (SIRS) [8], Sequential Organ Failure Assessment (SOFA) [9] and infection diagnosis of the patients. SIRS score was calculated according the data obtained in first 24 hours after admission in hospital and SOFA score were evaluated according data obtained within 2-4 days after trauma (Maximum SOFA score [10]). Patient’s infection diagnosis was confirmed according to records of the patient’ history, laboratory and radiology findings during stay in hospital.
Clinical outcome: Include the length time of stay in ICU, time of received mechanical ventilation, the length time of stay in hospital, mortality in hospital.
Scores of degree on secondary injury with trauma patients: So far, no any standard has been universally accepted to confirm post-traumatic inflammatory response and secondary injury. In order to evaluate the degree of secondary injury in trauma patients, this study designed a comprehensive evaluation scale of secondary injury according the above data to determine the severe degrees of secondary injury in the trauma patients (Table 1). The patients with a cumulative score ≥ 8 were considered to have serious secondary injury (comprehensive score was 1), if the patient’s cumulative score was <8, considered no serious secondary injury (comprehensive score was 0). All of the patient’s comprehensive score calculate had completed by non-study group persons according the evaluation scale.
| Group | Item | Evaluation standard | Comprehensive evaluate score | ||
|---|---|---|---|---|---|
| Lab result | Point | 2-3 points=1 score ≥ 4 points=2 scores |
|||
| 1 | 2 | 3 | |||
| LDH (U/L) | 700-1000 | 1001-2000 | >2000 | ||
| CK (U/L) | 500-1000 | 1001-2000 | >2000 | ||
| CRP (mg/L) | 50-100 | 101-200 | >200 | ||
| PCT (ng/L) | 0.5-1.0 | 1.1-2.0 | >2.0 | ||
| NE (× 109/L) | 8-10 | 11-20 | >20 | ||
| Clinical evaluation | SIRS score | ≥ 2 (within 48-72 hours after trauma) | Yes, 1 score | ||
| SOFA score | ≥ 4 (within 48-72 hours after trauma) | Yes, 1 score | |||
| Infect (y/n) | Systemic or local infection occurs after trauma | Yes, 1 score | |||
| Clinical outcome | MV (h) | Receive mechanical ventilation ≥ 24 h | Yes, 1 score | ||
| ICU (h) | Stay in ICU ≥ 48 h | Yes, 1 score | |||
| LOH (d) | Length of hospital ≥ 24 d | Yes, 1 score | |||
| Death | Death occurred 48 hours after the trauma | Yes, 1 score | |||
Note: Patients with cumulative scores of ≥ 8, be considered to have serious secondary injury, and the comprehensive score was 1 (serious), the patient with cumulative scores were <8, be considered non secondary injury, the comprehensive score was 0 (not serious); All patient’s comprehensive score calculate had completed by two non-study group persons.
Table 1: Score of degrees of secondary injury on trauma patient.
Statistical analysis
Statistical software package SPSS statistics 22 (Chicago, Illinois, USA) was used for statistics. Paired T test was used to compare the lymphocyte values between trauma groups and between each trauma group the corresponding control group. Binary logic analysis was used to analyze the correlation between blood lymphocyte count changes and the secondary injury score in all trauma patients. Receiver Operating Characteristic curve (ROC curve) and Youden index were used in the trauma patients to evaluate the feasibility of lymphocyte change in predicting secondary tissue injury, and the determination of cutoff values and sensitivity and specificity.
Patients
578 trauma patients admitted in the ICU during this study period, 371 cases were severe trauma patients (ISS score ≥ 16 ), 215 trauma patients (58% of the severe cases) were conformed to the inclusion criteria, 40 of these patients were died (18.6%). 60 medical patients were selected as control cases in the same period. The demographic characteristics of the trauma and control patients were shown in Table 2.
| Characteristics | Total |
|---|---|
| Trauma group characteristics | |
| Number of patients (M/F) | 215 (173/42) |
| Age median (IQR), y | 42 (33-52) |
| Traffic accident n (%) | 91 (42.3%) |
| High fall accident n (%) | 51 (23.7%) |
| Blunt wounded n (%) | 47 (21.9%) |
| Sharp instrument injury n (%) | 12 (5.7%) |
| Multiple injury n (%) | 105 (48.8%) |
| Mortality in hospital n (%) | 40 (18.6%) |
| Time from scene to ED (h) median (IQR) | 1.5 (1-2) |
| ISS median (IQR) | 32 (24-41) |
| SOFA median (IQR) | 6 (4-9) |
| Mechanical ventilation time (h) median (IQR) | 79 (19-267) |
| Stay time in ICU (h) median (IQR) | 215 (81-412) |
| Length time in hospital (d) median (IQR) | 34 (17-70) |
| Control group characteristics | |
| Number of patients (M/F) | 60 (37/23 ) |
| Age (year) median (IQR) | 49 (43,57) |
| Infection n (%) | 30 (50.0%) |
| Diabetic ketoacidosis n (%) | 7 (11.7%) |
| Drug poisoning n (%) | 4 (6.7%) |
| Severe heat stroke n (%) | 3 (5%) |
| Upper gastrointestinal hemorrhage n (%) | 2 (3.3%) |
| SOFA median (IQR) | 5 (4-8) |
Note: Inter Quartile Range (IQR); Injury Severity Score (ISS); Sequential Organ Failure Assessment (SOFA), 16 cases didn’t use mechanical ventilation.
Table 2: Demographic, characteristics of trauma patients and control patients.
Lymphocyte count
The value of lymphocyte counts in the trauma groups and the control groups were shown in Table 3. The median of lymphocyte counts in TrA was 4.09 × 109/L, that was significantly higher than that of other trauma groups and all of control groups, and there was statistical significant difference (P<0.000). There was no statistical difference on lymphocyte counts between each other trauma groups and the corresponding control group. The median of lymphocyte counts were less than or equal to 1.01 × 109/L in TrB, TrC and TrD.
| Group | Nu | Sample time Median (h) | Lymphocyte (n × 109/L) M ± SD (Median, IQR) |
Paired t-test | P |
|---|---|---|---|---|---|
| TrA | 215 | 1.5 | 4.25 ± 1.74 (4.09, 3.06-5.20) | TrA:ConA | P=0.000 |
| ConA | 60 | 2.5 | 1.11 ± 0.70 (0.93, 0.54-1.51) | TrA:TrB, C, D | P=0.000 |
| TrB | 215 | 7.5 | 1.04 ± 0.63 (0.91, 0.60-1.30) | TrB:ConB | P=0.187 |
| ConB | 60 | 8 | 0.97 ± 0.49 (0.91, 0.52-1.24) | TrB:TrC | P=0.510 |
| TrC | 215 | 20 | 0.94 ± 0.55 (0.84, 0.54-1.20) | TrB:TrD | P=0.142 |
| ConC | 60 | 21 | 1.11 ± 0.50 (1.03, 0.64-1.36) | TrC:ConD | P=0.611 |
| TrD | 25 | 57 | 1.04 ± 0.61 (0.90, 0.62-1.28) | TrC:TrD | P=0.503 |
| ConD | 60 | 60 | 1.20 ± 0.58 (1.09, 0.69-1.54) | TrD:ConD | P=0.867 |
Table 3: Blood lymphocyte count in trauma groups and control groups.
Proportion of patients with different lymphocyte counts
According to the normal reference range of lymphocyte counts adopted in the hospital (1.1-3.2 × 109/L), the patients in each trauma or control group were divided into three subgroups-greater than the upper limit of the normal range
(I); in the normal range (II) ; less than the lower limit of the normal range (III) .Within 3 hours after trauma (group TrA), there were 71.2% of the patients in the class I; only 1.4% of patients belonging the class III during this period. On the contrary, within 6-72 h after trauma, there were more than 62% of the patients (group TrB, TrC, TrD) in the class III.
The results are shown in Table 4 and Figure 1. During the same period, only 1 patient in the control group had a value of lymphocyte count higher than the upper limit. Conversely, more than 52% of the control patients had values of lymphocyte count lower than the lower limit of the normal range.
| Group | Lymph count (× 109/L) | ||
|---|---|---|---|
| ≥ 3.2 (Ⅰ) | 1.1‐3.2 (Ⅱ) | <1.1(Ⅲ) | |
| TrA (n.215) | 153 (71.2%) | 59 (27.4%) | 3 (1.4%) |
| ConA (n.60) | 1 (1.6%) | 25 (42%) | 34 (57%) |
| TrB (n.215) | 2 (0.9%) | 80 (37.2%) | 133 (61.9%) |
| ConB (n.60) | 0 | 29 (48%) | 41 (68%) |
| TrC (n.215) | 2 (0.9%) | 63 (29.3%) | 150 (69.8%) |
| ConC (n.60) | 0 | 26 (40%) | 34 (60%) |
| TrD (n.202) | 2 (0.9%) | 72 (33.5%) | 141 (65.6%) |
| ConD (n.60) | 0 | 29 (48%) | 31 (52%) |
Note: TrA, TrB, TrC, TrD, means trauma group A, B, C and D, respectively; ConA, ConB, ConC, ConD, means control group A, B, C and D, respectively.
Table 4: Proportion of patients with different lymphocyte counts in the trauma and control groups.
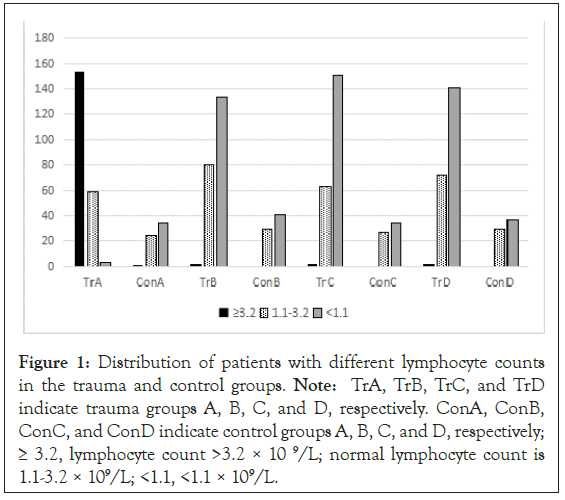
Figure 1: Distribution of patients with different lymphocyte counts in the trauma and control groups. Note: TrA, TrB, TrC, and TrD indicate trauma groups A, B, C, and D, respectively. ConA, ConB, ConC, and ConD indicate control groups A, B, C, and D, respectively; ≥ 3.2, lymphocyte count >3.2 × 10 9/L; normal lymphocyte count is 1.1-3.2 × 109/L; <1.1, <1.1 × 109/L.
Assessment the influence of fluid infusion quantity to lymphocyte count
To assess influence of fluid infusion volume to lymphocyte counts, we collected the data of infusion volume and loss volume (hemorrhage volume, urine volume, drainage volume) on the two time periods (0-6 hours (subgroup A) and 12-24 hours (subgroup B)), 110 studied trauma patients admitted between January 2018 and December 2019. Liquid equilibrium quantity was calculated on every patient by the infusion volume minus the loss volume, and Interquartile Range (IQR) values were calculated, the study patients divided into two subgroups according to more than the high quartile range (>75%) and less than low quartile range (25%), and the lymphocyte counts compared. The lymphocyte counts no statistical difference (Table 5). The results showed that fluid infusion did not significantly affect the blood lymphocyte counts.
| Subgroup item | Balance volume (Nu) | Lymph (× 109/L, mean ± x ) | P |
|---|---|---|---|
| A low quartile | 1890 ml (25) | 3.81 ± 1.69 | 0.678 |
| High quartile | 4780 ml (28) | 3.66 ± 1.39 | |
| B low quartile | 860 ml (25) | 1.10 ± 0.77 | 0.6 |
| High quartile | 760 ml (23) | 1.26 ± 0.77 |
Note: The subgroups were divide according to the value of the low quartile (<25%) and high quartile (>75%) of the fluid value of the inter quartile interval; subgroup A and B divided according 0-6 hours and 12-24 hours on patient admission time.
Table 5: Comparison of the lymphocyte count between the low quartile and the high quartile of fluid balance in the trauma group.
Ratio of lymphocyte count
To analysis change degree of the lymphocyte counts in the trauma patients between the four time periods in the study, the lymphocyte counts ratio of TrA to TrB, TrC, TrD was calculated through the division of the absolute lymphocyte counts of TrB, TrC, and TrD by that of TrA , respectively. The median value of lymphocyte counts in TrB, TrC and TrD were only 0.21 to 0.22 times of the TrA (Table 6).
| Group | Nu | Ratio of lymphocyte count | |
|---|---|---|---|
| Mean | Median (IQR) | ||
| B/A | 215/215 | 0.28 ± 0.18 | 0.22 (0.15, 0.33) |
| C/A | 215/215 | 0.27 ± 0.22 | 0.21 (0.13, 0.34) |
| D/A | 215/215 | 0.29 ± 0.22 | 0.22 (0.15, 0.34) |
Note: B/A means lymphocyte counts ratio of trauma group B to that of group A ratio, C/A, D/A as the same meaning.
Table 6: The ratio of lymphocyte count in trauma group B, C and D to trauma group A.
To evaluate the degree of secondary injury in trauma patients
To evaluate the degree of secondary injury in trauma patients the comprehensive evaluation scale was designed and used in this study, details as Table 1. In this study, 188 (87.4%) trauma patients were assessed as serious secondary injury (secondary injury cumulative score was 1 point), 27(12.6%) trauma patients no serious secondary injury (0 point). In order to confirm effective the comprehensive evaluation scale on secondary injury, lymphocyte ratio, the data of SOFA scores, time stay in ICU, time stay in hospital, mortality and lymphocyte ratio were compared between the severe secondary injury group and the non-severe secondary injury group. The results showed a significant statistical difference between the two groups of patients (Table 7).
| Lymphocyte ratio | Severe | Non‐severe | P | ||
|---|---|---|---|---|---|
| Mean | Median | Mean | Median | ||
| B/A | 0.11 | 0.12 | 0.49 | 0.37 | 0 |
| C/A | 0.11 | 0.13 | 0.77 | 0.63 | 0 |
| D/A | 0.2 | 0.24 | 1.02 | 0.92 | 0 |
| SOFA | 7 | 7 | 3 | 4 | 0 |
| MV time (h) | 152 | 155 | 97 | 97 | 0 |
| ICU time (h) | 172 | 218 | 102 | 101 | 0 |
| Hospital time (d) | 125 | 129 | 14 | 19 | 0 |
| Death (n) | 38 (20.2%) | - | 2 (7.4%) | - | 0.006 |
Note: B/A, lymphocyte counts of trauma group B to that of group A ratio, C/A, D/A as the same meaning ;Sequential Organ Failure Assessment (SOFA).
Table 7: Comparison the results between the two trauma groups that divided according to the comprehensive evaluation scale.
There was a significant positive correlation between the ratio values of the lymphocyte counts and the the results of comprehensive evaluation scale on secondary injury of trauma patients (P=0.000). This result showed it is feasible to evaluating lymphocyte count ratio on predict severe degrees of secondary injury of trauma patients (AUC was 0.800, 0.899, 0.908, respectively), the predictive thresholds of lymphocyte ratio on severe degree of secondary injury in trauma patients were 0.28 to 0.35, the prediction sensitivity were 76% to 85.6% and specificity 72% to 96% (Tables 8 and 9) (Figure 2).
| Group | B | S.E. | Wald | p | Exp (B) | Cut off value | Sensibility | Specificity | AUC | Youden index |
|---|---|---|---|---|---|---|---|---|---|---|
| B/A | 3.76 | 0.476 | 62.355 | 0 | 42.952 | 0.32 | 0.78 | 0.74 | 0.8 | 0.523 |
| C/A | 4.265 | 0.513 | 61.69 | 0 | 71.19 | 0.28 | 76.00% | 96.30% | 0.899 | 0.724 |
| D/A | 4.496 | 0.543 | 67.113 | 0 | B/A | 3.76 | 0.476 | 62.355 | 0 | 42.952 |
Note: B/A means lymphocyte counts of trauma group A to that of group B ratio, C/A, D/A as the same mean.
Table 8: The results of bivariate logistic regression analysis, ROC curve and Youden index of lymphocyte ratio in the trauma group.
| Group | AUC | σ | P | 95% CI | |
|---|---|---|---|---|---|
| Low | High | ||||
| BrA | 0.8 | 0.045 | 0 | 0.713 | 0.887 |
| CrA | 0.899 | 0.028 | 0 | 0.844 | 0.953 |
| DrA | 0.908 | 0.024 | 0 | 0.861 | 0.956 |
Note: BrA, lymphocyte counts of trauma group B to that of group A ratio; CrA and DrA with the same meaning.
Table 9: The lymphocyte ratio and secondary injury score.
Figure 2: ROC curve of lymphocyte ratio and secondary injury score.
Improvements in early resuscitation and promotion of damage control surgery have improved the survival outcomes if trauma patients. However, two-thirds of patients die from secondary injury caused by traumatic immune dysregulation, mostly presented as anti-inflammatory and pro-inflammatory responses [10-12]. Tissue destruction and cell death caused by trauma lead to a large number of cytokines being released in the blood, thus activating the immune system. Patients may present severe systemic inflammatory reactions, and the degree of local or systemic inflammatory reaction is related to the severity of tissue injury caused by trauma [13-16]. Lymphocytes play an important role in the immune system, and changes in lymphocyte counts in patients with trauma are associated with post-traumatic inflammatory response [17].
In this retrospective study, 215 trauma patients with ISS scores greater than 16 admitted were enrolled. We found the lymphocyte counts increased above the upper limit of normal range in 71% of the trauma patients the first 3 hours after trauma, then decreased significantly. The data of this study showed that following 6 to 72 hours after trauma, the value of lymphocyte counts was less than the low limit of normal range in more than 62% of the patients. Because that there is no gold standard for evaluating the inflammatory response after trauma, to determine whether this changes of lymphocytes is related to post-traumatic inflammatory response, we collected laboratory results in 7 days on the patients after trauma and clinical manifestations of the patients in hospital stay to comprehensive evaluate whether there is second injury and the extent, and analyze whether the changes in the lymphocyte count of patients within 72 hours are related to it. The results of this retrospective study showed the decrease degree of lymphocyte counts was significant relationship with the degree of secondary tissue injury, the degree of the change can be used to predict the severe degree of secondary tissue injury occurred by inflammatory reaction in trauma patients. Likewise, Cabrera, et al. [18] reported that in patients with ISS>25, there was a sharp increase in lymphocyte counts within 2 h after injury and decreased after 24 h, T cells decreased by 40% within 24 h after trauma. Manson, et al. [19] reported that lymphocytosis was noted in severely injured patients within 2 h after the trauma, then decreased and could be sustained for up to 24 h after the trauma. But they more concerned the changes of lymphocyte subsets, without the relationship between changes in lymphocyte counts and post traumatic secondary injury. In another report, Manson, et al. [6] observed that the peripheral blood lymphocyte counts decreased significantly after trauma, they authors suggests that lymphocyte count at 48 h could be an early indicator of poor prognosis, and they consider that if lymphocytes decreased to <0.5 × 109/L after 48 h of trauma, the mortality rate could be as high as 45%. But they found that the greatest changes in these cells are occurring between 0 and 2 h following injury, is different from our results. Still need more evidences to strengthen that lymphopenia may be involved in the pathogenesis of adverse outcomes and that restoration of lymphocyte count may be essential to recovery.
The function of lymphocytes in the human body can be inhibited or activated by trauma [7], but the mechanism is complicated. Jo, et al. [20] reported that the numbers of CD3+ T cells in the peripheral blood lymphocytes was found to be comparable between patients with multiple trauma and a healthy control group. They demonstrated that absolute numbers of innate-like T lymphocytes were reduced early and markedly in patients with trauma compared with that in the healthy control group.
One factor associated with post-traumatic lymphopenia is cortisol release after trauma, this can lead to the excretion of neutrophils and induce lymphocyte apoptosis [11]. On the other hand, in the bone marrow, it rose after 6 h and remained elevated after 24 h. Posttraumatic lymphocyte counts and function changes are complex and not fully understood [20]. However, changes in lymphocyte counts in patients with trauma are related to the post-traumatic inflammatory response. Addition, increased extravasation of regulatory T cells into both lymphoid and non-lymphoid organs may explain the decrease in lymphocyte counts in the peripheral blood [21,22]. Despite the profound influence of lymphocytes on inflammation in all these processes, little is known about the mechanisms of lymphocyte counts change [23].
The biochemical and physiological changes caused by trauma are related to the nature and extent of the inflammatory response [5]. In humans, LDH is seen in the liver, the heart, the kidney, the muscle tissue, and the gastrointestinal tract. In traumatic patients, once these parts are damaged, inflammatory mediators are released, microcirculation is obstructed, lactic acid can accumulate in the body, lactate dehydrogenase synthesis and secretion increase; combined with the increase of membrane permeability caused by injury, the level of blood lactate dehydrogenase increases.
Therefore, blood LDH concentration is closely related to cell injury severity. In addition, serum LDH levels can reflect the status of systemic inflammation, oxygen necrosis, and haemolysis of local tissue [24-26]. CRP and PCT can also be used as indicators of the degree of inflammatory damage, and CK is a response indicator of muscle tissue injury. SIRS score is still valuable for judging systemic inflammatory response and tissue reperfusion injury [27]. The SOFA score is an increasingly important tool in defining both the clinical condition of the individual patient and the response to therapies in the context of clinical trials [10], but SOFA is a better indicator of tissue and organ dysfunction [28]. In this study, the above indicators were used as comprehensive scoring indicators of secondary injury.
The relationship between secondary injury after trauma and changes in lymphocyte counts and functions remains unclear and needs to be further studied. The important inclusion criterion in this study was the ISS score, but some patients with brain injury or sharp injury did not show more changes in lymphocyte ratio, and presented severe degree of secondary injury. We consider that changes in lymphocytes in patients with trauma may be related to the severity of damage and the local blood circulation status of injured organs and damaged regions, but it need to find enough evidence to prove in the future. In addition, we do not comparing changes in lymphocyte counts after 72 h and the clinical condition of the patients with trauma. But we found that the time of secondary injury relief in patients with trauma may be related to the time of lymphocyte count recovery after trauma. However, these findings need further study.
This retrospective study on 215 patients with severe trauma (ISS score ≥ 16) found that lymphocyte counts in most patients with trauma significantly increased within the first 3 h after trauma. Median count was 4.09 × 109/L, which decreased significantly in the following 6-72 h (median: 0.84-0.91 × 109/L). The lymphocyte count can impact the cardiovascular system, maintaining a balanced and healthy lymphocyte count which is crucial for proper immune function and cardiovascular health. Regular monitoring and appropriate medical interventions may be necessary in cases where the lymphocyte count is significantly elevated or imbalanced, to minimize the risk of cardiovascular complications. In this retrospective study, we observed that the changes in the lymphocyte count early after trauma had a significant relationship with severity of secondary injury in patients with trauma. Therefore, the changes in the degree of the lymphocyte count can be used to predict the degree of severity of secondary injury in patients with trauma. However, the mechanism of lymphocyte count change has not clear. Therefore, the cause of the relationship between the change in lymphocyte counts and the degree of secondary injury in patients with trauma still needs further study.
[Crossref][Google Scholar][PubMed]
Citation: Cao F, He R, Huang Y, Li Z, Wu X, Chen R, et al (2023) Changes of the Blood Lymphocytes on Severe Trauma Patients in Early Time: A Retrospective Cohort Study. Angiol Open Access.11:345.
Received: 08-May-2023, Manuscript No. AOA-23-23968; Editor assigned: 12-May-2023, Pre QC No. AOA-23-23968 (PQ); Reviewed: 26-May-2023, QC No. AOA-23-23968; Revised: 02-Jun-2023, Manuscript No. AOA-23-23968 (R); Published: 09-Jun-2023 , DOI: 10.35248/2329-9495.23.11.345
Copyright: © 2023 Cao F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.